Palliative care for patients with esophageal cancer: a narrative review
Mr. A is a 58-year-old man with a medical history of hypertension, hyperlipidemia and coronary artery disease s/p myocardial infarction and 4-vessel CABG, as well as a 40 pack-year history of tobacco use who had four months of difficulty swallowing. He saw his primary care physician who prescribed him a 14-day course of a proton pump inhibitor, which did not improve his symptoms, and he also started having pain initially with swallowing and then more consistently. He was referred to a gastroenterologist and underwent an endoscopy. During the procedure, a 6-cm mass was found in the distal esophagus with near complete obstruction. Biopsy revealed adenocarcinoma of the esophagus and he was referred to oncology for evaluation and management. He did not have any metastatic disease at diagnosis, but due to his medical comorbidities, he was deemed a poor surgical candidate. He underwent curative-intent chemoradiation with complete response to treatment. He had persistent pain during treatment and required an esophageal stent placement for dysphagia, which was moderately helpful, although he was never able to eat certain foods easily. Nine months after completion of treatment, he developed chest pain and fatigue and imaging revealed metastatic spread. He was treated with palliative chemotherapy for six months with two different regimens before shifting to comfort-focused care. He elected hospice care and died peacefully at home 16 months after initial diagnosis.
Introduction
Defining palliative care
Palliative care is supportive care for patients with serious illness and can be provided at any stage of illness from initial diagnosis to end of life. Palliative care takes a multifaceted approach that integrates the physical, psychological, spiritual, and practical needs of patients and families living with serious illness. Aspects of palliative care include advance care planning and support with medical decision making, intensive symptom management, and provision of spiritual and emotional support. The underlying mission of palliative care is to help patients with serious illness live as well as possible.
Palliative care is recommended for all cancer patients alongside cancer-directed treatment—regardless of whether the cancer treatment is of curative intent, or with the goal to control the spread of the disease and prolong life. Studies have shown that cancer patients who receive early palliative care concurrent with disease-modifying treatments have better symptom control, higher satisfaction, more focused goals of care, and overall better quality of life without accelerated mortality (1). A study of early palliative care in patients with metastatic non-small cell cancer suggested that in some cancers, the provision of palliative care alongside standard cancer treatment may even result in longer survival (2). Like all people with cancer, patients with esophageal cancer benefit from palliative care because of the heavy symptom burden and emotional distress caused by this serious diagnosis.
There are two tiers of palliative care for cancer patients. Primary palliative care, which is symptom management and goals of care conversations provided by the patient’s primary oncology team, is the first tier and is available to all cancer patients. For patients with complex needs, referral to a palliative care specialist is recommended. Specialist palliative care is ideally provided by a transdisciplinary team of expertly trained specialty physicians, nurses, social workers, chaplains, and pharmacists who work alongside a patient’s typical healthcare providers to provide comprehensive and integrated symptom management, psychosocial and spiritual support, and advance care planning. This two-tiered approach is essential given the shortage of specialist palliative care providers. While the incidence of esophageal cancer is low overall, approximately 18,000 cases annually in the United States, the morbidity and mortality rates are high, and many patients have complex and extensive symptoms that make support from specialty palliative care providers valuable. The remainder of this article discusses how to recognize and meet the routine palliative care needs of esophageal cancer patients and provides guidance on when to seek specialist-level palliative care consultation. We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/atm-20-3676).
Palliative care needs of esophageal cancer patients
Communication
Clear and effective communication is essential to the provision of high-quality palliative care for esophageal cancer patients. Discussing serious medical news, eliciting patient and family values, making patient-centered recommendations, and providing support in difficult times all require skilled communication. Contrary to the prevailing myth that certain people are innately good communicators while others are not, serious illness communication is a skillset that is honed with training and practice. Communication with patients and families must be bidirectional: it requires clinicians to ask questions and listen deeply, as well as provide clear information that is tailored to the individual patient and family. Finally, serious illness communication requires a willingness to sit with emotions that arise—whether in the patient and family, or in oneself—and respond with empathy. There are many resources available for clinicians who wish to build their comfort and skill with serious illness communication, such as those developed by the nonprofit organization VitalTalk (www.vitaltalk.org), and the Serious Illness Conversation Guide developed by Ariadne Labs (www.ariadnelabs.org/areas-of-work/serious-illness-care/) (3,4). Considering the case of Mr. A, the palliative care team can provide communication support that helps Mr. A and his family process the diagnosis and the emotional toll that comes with a cancer diagnosis.
Advance care planning (ACP)
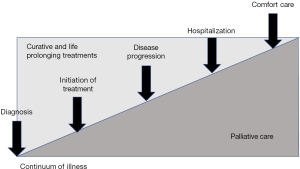
ACP is the process of thinking about future healthcare decisions and communicating those decisions to others. Patients can communicate their decisions and plans orally or in writing—ideally by documenting them in an advance healthcare directive (AD). ACP is a way of planning for future health problems and crises and is meant to provide an opportunity to be proactive about health care decisions rather than reactive during a medical crisis. ACP empowers patients and families to be the leading voice in their own health decisions and allows clinicians to provide medical care that aligns with the patient’s values and makes sense medically. While ACP can and should occur in healthy patients, many people do not engage in any meaningful planning until they receive a serious diagnosis. Beginning at diagnosis, there are ample opportunities along the disease continuum to engage in ACP (Figure 1). ACP in cancer patients is particularly valuable because there are many unexpected complications that can occur in the course of disease.
Patients with esophageal cancer, like all patients with a cancer diagnosis, benefit from advance care planning and completion of an advance directive. There are numerous reasons to engage in ACP and few risks associated with the process. ACP includes several different components: identifying a surrogate decision maker, preparing for unexpected events as best as possible, having a plan to mitigate crises, as well as considering end-of-life wishes. Although clinicians often worry about upsetting patients by discussing ACP, studies show that most patients welcome the opportunity and express satisfaction after having meaningful conversations with health care providers. In addition, family members and friends who may be thrust into a decision-making role in the future benefit from conversations and documents that help them know a patient’s wishes before an emergency hits.
A key component of advance care planning is identifying a surrogate decision maker, also known as a durable power of attorney for healthcare (DPOA-HC) or healthcare proxy. This is a person who is legally designated to make medical decisions for a patient when the patient is unable to do so for him- or herself. The role is not to take over the patient’s decision-making powers, but rather to be available as a backup to represent the patient’s voice if the patient is unable to make or communicate a decision. Patients should be advised to choose a surrogate that they trust, who will ask doctors good questions, and who will respect their previously stated wishes. A medical POA is different from a general or financial POA and must be separately identified to have legal authority to make medical decisions. Most state forms recommend having a main proxy and one or two alternate proxies to step in or assist if the primary person is unavailable or needs additional support.
A second component of advance care planning is documenting a person’s wishes about the kind of medical care that they do and do not want. This part of ACP helps people think about and prepare for what may come throughout the course of their illness and starting the conversation in a time of calm—rather than amidst a medical crisis—is essential. This is less about anticipating every possible scenario or decision that may arise, and more about eliciting an individual’s unique values and goals and understanding how those would guide or drive medical decision-making in a difficult situation. There are some specific decisions that are helpful to consider ahead of time, such as preferences around life support, resuscitation, ongoing medical treatments and end-of-life preferences. Documenting these preferences in an AD increases the likelihood that the patient receives medical care aligned with his or her values and helps ease the burden of decision-making shouldered by the patient’s DPOA-HC in the future when facing emotionally-charged decisions such as intubation or feeding tube placement.
For most patients, identifying a surrogate decision-maker is straightforward. Mr. A, for example, may pick his wife of 30 years with his adult children as alternates. However, there are some patients that have a difficult time identifying a surrogate. This generally occurs for one of two main reasons: the first reason is that some patients do not have a strong support person in their lives that they trust to make medical decisions and the second reason is that some patients are unwilling to impose the burden of decision making onto their loved ones. In either scenario, engaging in comprehensive advance care planning becomes even more essential so that the patient has clear plans and expectations for their care, and that this information is documented and accessible to the patient’s health care providers.
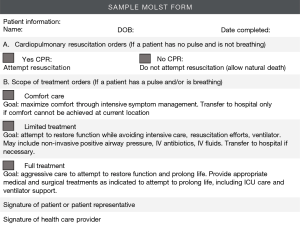
Physician Orders for Life-Sustaining Treatment (POLST), also called Medical Orders for Life-Sustaining Treatment (MOLST), are state-approved out-of-hospital medical orders that specify a patient’s end-of-life preferences. Whereas an AD is a legal document, a POLST form is a medical order signed by a patient or DPOA-H and a licensed health care professional such as a physician or nurse practitioner, and available in most but not all states. If a patient wishes to die naturally without cardiopulmonary resuscitation (CPR) or life support, completing a POLST with his or her physician is essential, because CPR is the default option when medical personnel encounter a patient who is pulseless and not breathing. A typical POLST form allows patients to specify their “code status” (i.e., Perform CPR versus Do Not Resuscitate/Allow Natural Death) and select the desired intensity of medical interventions (Full treatment, Limited treatment, or Comfort-focused treatment only). Some also allow patients to specify their decisions regarding specific types of life-sustaining treatments such as mechanical ventilation or artificial nutrition. This form protects patients from receiving unwanted aggressive care at the end of life (Figure 2).
Living with a diagnosis of esophageal cancer can be unpredictable and frightening. Engaging in ACP helps patients and their families navigate these unpredictable situations with the best preparedness possible—to “hope for the best and prepare for the rest.”
Symptom management
Another essential role that palliative care plays in the care of patients with esophageal cancer is symptom management. The symptomatic burden in patients with esophageal cancer is intense and includes pain, nausea and vomiting, dysphagia, malnutrition, anxiety, and depression among other less common symptoms. Treating symptoms aggressively improves quality of life for patients and allows them to more effectively tolerate lifesaving and life-prolonging treatments. The most common symptoms experienced by patients with esophageal cancer are addressed below.
Dysphagia
Dysphagia is one of the most common presenting symptoms of esophageal cancer, as it was for Mr. A, and it continues to be problematic for many patients throughout the course of the disease. Many patients with esophageal cancer require some form of palliative treatment for dysphagia during their disease course. Effective management of dysphagia is essential; when left untreated, it has a hugely negative impact on quality of life, nutritional status, and function. If patients become malnourished, tolerating chemotherapy is very difficult and can affect the patient’s ability to continue with treatment. Dysphagia can also lead to psychosocial distress, such as struggles with body image due to severe weight loss or changes to social relationships due to the inability to share meals with others.
Options for management of dysphagia include interventional treatments and dietary modifications as well as medications to shrink the tumor and palliate the symptoms (5). The interventional management strategies include endoscopic procedures aimed at minimizing the size of the tumor and opening a compressed esophagus, including several varieties of dilatation, stent placement and ablative procedures. Surgical treatment options include palliative resections and bypass surgeries. Radiation for palliation of dysphagia is a commonly used tool, and of course chemotherapeutic agents to reduce disease burden can improve symptoms. Mr. A’s dysphagia improved after he had a complete response to treatment, although there may not be a complete return to normal swallowing due to scarring even when no disease remains. Palliative radiation is a particularly valuable tool in managing dysphagia due to tumor obstruction. Even when curative intent treatments are no longer options either due to metastatic spread or patient comorbidities, cancer-directed therapies provide valuable palliation of symptoms.
Dietary changes can also be effective in palliating dysphagia. Small meals and softer foods are easier to tolerate when a patient has a partially obstructed esophagus. Patients often find drinking fluids when eating can ease swallowing. Liquid diets are important and using nutritional supplement drinks may help people maintain nutritional status when unable to eat adequately. There is also the option of bypassing the esophagus and using gastrostomy tubes or total parenteral nutrition (TPN) if oral intake is unsuccessful despite dietary modifications. While enteral feeds or TPN provide adequate nutrition, the emotional impact of not eating by mouth can be devastating for patients and oral intake should be preserved as long and as much as possible.
Medication management of dysphagia is marginally effective. Typical medications used include antacid medications, anti-emetics, promotility agents, and anti-spasmodic agents, but none of these medications treat the underlying cause in the case of a mechanical obstruction. Management of pain as outlined below is essential when odynophagia is limiting swallowing.
Nausea and vomiting
Nausea and vomiting are common symptoms in patients with esophageal cancer and have many causes, including the cancer and mechanical obstruction, mucosal irritation, chemotherapy, radiation, pain medications, dehydration, and anxiety. Identifying the root cause(s) of nausea most effectively guides treatment. For example, both chemotherapy-induced nausea/vomiting (CINV) and opioid-induced nausea/vomiting are mediated by the chemoreceptor trigger zone, and thus 5HT-3 antagonists such as ondansetron and D2-antagonists such as prochlorperazine and haloperidol are effective first-line antiemetics. Anxiolytics are helpful for anxiety-driven or anticipatory nausea, particularly in those who are receiving highly emetogenic chemotherapy regimens. Patients experiencing early satiety or nausea related to slow gut motility may benefit from metoclopramide, a dopamine antagonist with prokinetic properties. Mechanical or physiologic obstruction causing nausea is more effectively managed with interventional procedures than with medications. In patients with heavy and thick secretions, using anti-cholinergic medications to dry secretions or mucolytic medications may ease nausea associated with secretions. Table 1 summarizes commonly used symptom management medications and recommended starting doses.
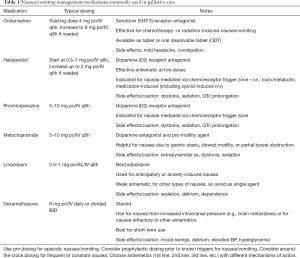
Full table
Pain
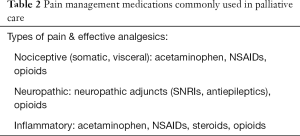
Pain occurs in almost all patients with esophageal cancer at some point during the disease course. Pain was one of the first symptoms that Mr. A had when he first presented for medical care, and signaled metastatic spread of disease as well. The underlying etiology of the pain in esophageal cancer can be related to many different causes: direct compression from tumor, effects from treatments, and neuropathic pain. Pain arising from the esophagus usually manifests in one of two ways: pain with swallowing and eating, or chest and back pain at rest. Initial management with a non-opioid analgesic such as acetaminophen is a reasonable first step for patients presenting with mild pain. Although non-steroidal anti-inflammatory drugs (NSAIDs) can also be considered, they are relatively contraindicated in patients who are elderly or suffer from existing cardiovascular or renal disease. Furthermore, NSAIDs can cause gastritis, esophagitis, dyspepsia, or bleeding—and thus are often avoided in esophageal cancer patients. For moderate or severe cancer pain, opioids are the mainstay of pain management. We recommend starting with as-needed dosing of a short-acting opioid. For patients suffering from dysphagia, liquid formulations of short-acting opioids are often preferable to the tablet form. Sublingual preparations are also an excellent option when swallowing is painful or difficult. When a patient requires more than three doses of a short-acting opioid in a 24-hour period, adding a long-acting (sustained-release) opioid can improve pain control. Typically, using approximately 75% of the 24 h opioid requirement as a long-acting medication is an effective way to manage persistent, cancer-related pain. For patients with dysphagia and pain, swallowing pills may be problematic. There are two types of long-acting opioids that can obviate the need to swallow pills. Transdermal fentanyl is a good option for long-acting coverage, and Xtampza (branded oxycodone ER) and Kadian (branded morphine SR) are specific abuse-deterrent capsules that have the option of being opened and the microsphere contents can be swallowed with applesauce or administered through a feeding tube. All patients prescribed opioids should be educated on the expected side effect of opioid-induced constipation (OIC) and started on a bowel regimen. Senna and polyethylene glycol are effective laxatives for OIC, while docusate is no longer recommended due to evidence pointing to a lack of efficacy (6). Tables 2-4 summarize commonly used pain management medications.
Full table
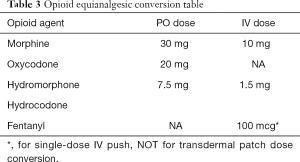
Full table
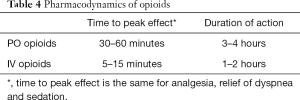
Full table
While pain arising from the primary tumor is usually nociceptive or visceral in nature, some esophageal cancer patients may also experience neuropathic pain—for example, from tumor invasion into a nerve plexus, or as a side effect of platinum-based chemotherapy agents such as cisplatin and oxaliplatin used in esophageal cancer treatment. For these patients, neuropathic agents such as gabapentin, pregabalin, or SNRIs (duloxetine or venlafaxine) may be helpful adjuncts.
Palliative radiation is also an effective treatment for pain caused by localized metastases. When a patient has a prognosis on the order of months, hypofractionated courses of radiation provide excellent pain relief while minimizing the burden of repeated radiation treatments. Peak pain relief occurs two to four weeks after completion of radiation, so this treatment should be coupled with medication management.
Safe and effective pain management requires meticulous patient education and close collaboration between patient and prescriber. Opioid agreements are an important safeguard to help patients effectively and appropriately use opioids and ensure proper prescribing practices. Although prescribing the opioid reversal agent naloxone (i.e., OEND—opioid education and naloxone distribution) is not routinely recommended for palliative care and hospice patients, it may be appropriate for some patients and should be considered on a case-by-case basis. Consultation with a palliative care specialist and/or pain pharmacist is recommended for esophageal cancer patients with pain refractory to initial management and any cases that are particularly complex or difficult to manage. Finally, a select group of patients with refractory pain may find relief with interventional techniques such as neurolytic procedures to target specific peripheral or autonomic nerves, or placement of an intrathecal pump.
Psychosocial needs of esophageal cancer patients
Psychological distress
Psychological distress is widespread for patients with esophageal cancer and take a major toll on quality of life. Upon initial diagnosis, shock and anxiety are near universal emotions experienced by cancer patients—especially when the disease is already advanced at the time of diagnosis, as it is for the majority of esophageal cancer patients, 32% of whom present with metastases to regional lymph nodes and 40% of whom present with distant metastases. Even with locally advanced disease, the prognosis is still poor and up to 70% of patients may relapse. Patients and families commonly describe feelings of stress, worry, sadness, anger, disbelief, or guilt. Symptoms of depression and anxiety are common in patients with serious illness: in palliative medicine settings, depressive symptoms are reported in up to 42% of patients, and significant anxiety in as many as 70% of patients (7). While data is lacking on the prevalence of psychiatric disorders such as major depressive disorder and anxiety disorders among esophageal cancer patients specifically, studies of patients with serious illness suggest a significantly higher prevalence compared to the general population. For example, a 2007 study of patients with advanced cancer suggested that 21% of patients met criteria for major or minor depression, and 14% of patients met the diagnostic threshold for an anxiety disorder (7).
Despite its high prevalence, clinical depression is underdiagnosed and undertreated in patients with cancer. In a busy oncology practice where there is not enough time to perform comprehensive psychiatric assessments of all patients, a simple two-question screen is recommended as a starting point. The screen is considered positive if a patient answers “Yes” to both of the following questions: “Are you depressed?” and “Have you experienced loss of interest in things or activities that you would normally enjoy?” (8). In a meta-analysis of 5 studies of cancer patients and patients receiving palliative care, this two-question screen had a pooled sensitivity of 91% and a specificity of 86% (9). Patients who screen positive should undergo a more in-depth evaluation for clinical depression. It is worth noting that in cancer patients, the somatic symptoms of depression such as changes in appetite and weight, sleep, and fatigue are often caused by the underlying cancer. Thus, assessment of depression in cancer patients often gives greater weight to the emotional and cognitive symptoms of depression, and clinicians must consider the time course of symptoms, changes from baseline, and proportionality of symptoms relative to the medical situation in order to arrive at a clinical diagnosis. “Look-alike” conditions to major depression include adjustment disorder with depressed mood, demoralization syndrome, and prolonged grief (10).
Patients with esophageal cancer may experience anxiety symptoms as the result of an underlying psychiatric anxiety disorder, a physiologic problem, or as a reaction to psychosocial stressors and existential/spiritual concerns. Examples of anxiety disorders include adjustment disorder with anxiety, generalized anxiety disorder, panic disorder, and posttraumatic stress disorder. Physiologic conditions leading to anxiety include respiratory failure, weakness, uncontrolled pain or other physical symptoms, insomnia, medications (including steroids or opioids), and delirium. Psychosocial stressors can range from fears about cancer treatment and prognosis, lack of clear information, financial concerns, inadequate support, or disrupted social relationships. For patients with esophageal cancer who have undergone highly morbid surgical procedures, there may be the additional burden of body image issues and communication difficulties from surgical scars and hardware, such as tracheostomies, feeding tubes and possibly even laryngectomies limiting communication. Finally, existential and spiritual concerns such as loss of purpose and fear of losing independence can lead to anxiety.
Addressing psychological distress in patients with esophageal cancer leads to significant gains in their quality of life. Management falls into several buckets. First, efforts should be made to identify and address any underlying physiological issues contributing to mood symptoms as best as possible. Second, all patients and families should receive education and psychosocial support. Evidence from RCTs in cancer patients shows that interactions that convey empathy for the patient’s distress and active listening promote psychological adjustment; provision of anticipatory guidance promotes psychological well-being; and opportunities to discuss feelings with a health professional reduces a patient’s psychosocial distress. Third, referral for nonpharmacologic interventions such as psychotherapy and complementary/alternative therapies (e.g., relaxation training, hypnotherapy, mindfulness, meditation, acupuncture) can be considered. Finally, pharmacologic management with antidepressants or anxiolytics should be considered for patients diagnosed with clinical depression or an anxiety disorder. Studies show that antidepressant use is effective and appropriate for the treatment of major depression in patients with serious or life-threatening illness (11,12). The evidence base for pharmacologic treatment of anxiety in adult palliative care patients is less robust, so medication use is guided by evidence from non-palliative care patients and recommendations of clinical experts.
While oncologists can do much to support patients experiencing psychological distress, it can be a heavy burden to bear alone. We recommend a collaborative approach that brings together the expertise and support of professionals in cancer centers and in the community: social workers, chaplains, mental health professionals, palliative care specialists, and community practitioners.
Caregiver burden
Being a caregiver to any person is challenging; being a caregiver to a person who has needs for medication administration and feeding assistance multiple times a day can quickly become overwhelming. The same high symptom burden that causes significant emotional distress for patients likewise can be overwhelming for loved ones involved in the patients’ care. Palliative care is often unique in its focus on the patient within the context of their family and support network. While neither oncologists nor palliative care specialists can prescribe medications for a patient’s family members, they can provide support by inquiring about caregivers’ emotional and physical wellbeing and coping. Providing help with logistical or practical issues—for example, identifying additional resources that families can access to augment or offset their caregiving or financial burden—or suggesting ways to support coping and self-care are usually highly appreciated by caregivers. It is essential to take a team-based approach to caregiver support by calling upon the expertise of social workers, chaplains, psychologists, case managers, and others. Palliative care providers encourage family members to practice self-care with the old mantra: “You can’t take care of someone else if you aren’t taking care of yourself.”
End of life care
In the unfortunate but common circumstance that a patient’s esophageal cancer progresses, and further cancer-directed treatment will not prolong life or improve quality of life, it is important to communicate the poor prognosis to the patient and family. This is a challenging conversation, but prior advance care planning discussions prove helpful if patient’s goals and wishes have been elucidated. Hospice is a philosophy of care that focuses on maximizing comfort and minimizing suffering for however long a patient has left to live. Hospice is an essential service that helps patients to die peacefully at home or in a hospice facility, as Mr. A was able to do in the initial case history. Importantly, hospice also provides thirteen months of bereavement services for a patient’s loved ones to help families navigate the first year after a loss. This is an extension of how palliative care treats the patient as part of a family and community.
Conclusions
Patients with esophageal cancer benefit from palliative care and we encourage a collaborative approach to care. Many patients with esophageal cancer come to medical attention with a heavy symptom burden and therefore early involvement of specialty palliative care can improve the symptom management and quality of life for these patients. Palliative care offers supportive care while focusing on curative-intent treatments and continues to support and treat the patient and family throughout the disease trajectory, from diagnosis to cure or death. For those without access to specialist palliative care, we advocate for using a comprehensive approach to the management of the numerous symptoms that occur and providing emotional, spiritual, logistical, and decision-making support for patients and families dealing with the many challenges of esophageal cancer. More trials are needed to further clarify the palliative needs of esophageal cancer patients and opportunities to enhance the palliation of these patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Dr. Khaldoun Almhanna) for the series “Gastroesophageal Cancer 2020” published in Annals of Translational Medicine. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-3676
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-3676). The series “Gastroesophageal Cancer 2020” was commissioned by the editorial office without any funding or sponsorship. KA served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Translational Medicine from Nov 2019 to Oct 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009;302:741-9. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Back AL, Fromme EK, Meier DE. Training Clinicians with Communication Skills Needed to Match Medical Treatments to Patient Values. J Am Geriatr Soc 2019;67:S435-41. [Crossref] [PubMed]
- Paladino J, Bernacki R, Neville BA, et al. Evaluating an Intervention to Improve Communication Between Oncology Clinicians and Patients With Life-Limiting Cancer: A Cluster Randomized Clinical Trial of the Serious Illness Care Program. JAMA Oncol 2019;5:801-9. [Crossref] [PubMed]
- Ramakrishnaiah VP, Malage S, Sreenath GS, et al. Palliation of Dysphagia in Carcinoma Esophagus. Clin Med Insights Gastroenterol 2016;9:11-23. [Crossref] [PubMed]
- Tarumi Y, Wilson MP, Szafran O, et al. Randomized, double-blind, placebo-controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage 2013;45:2-13. [Crossref] [PubMed]
- Wilson KG, Chochinov HM, Skirko MG, et al. Depression and anxiety disorders in palliative cancer care. J Pain Symptom Manage 2007;33:118-29. [Crossref] [PubMed]
- Payne A, Barry S, Creedon B, et al. Sensitivity and specificity of a two-question screening tool for depression in a specialist palliative care unit. Palliat Med 2007;21:193-8. [Crossref] [PubMed]
- Mitchell AJ. Are one or two simple questions sufficient to detect depression in cancer and palliative care? A Bayesian meta-analysis. Br J Cancer 2008;98:1934-43. [Crossref] [PubMed]
- McKee KY, Kelly A. Management of Grief, Depression, and Suicidal Thoughts in Serious Illness. Med Clin North Am 2020;104:503-24. [Crossref] [PubMed]
- Rayner L, Price A, Evans A, et al. Antidepressants for depression in physically ill people. Cochrane Database Syst Rev 2010.CD007503. [PubMed]
- Rayner L, Price A, Evans A, et al. Antidepressants for the treatment of depression in palliative care: systematic review and meta-analysis. Palliat Med 2011;25:36-51. [Crossref] [PubMed]