
Determinants of intraocular lens tilt and decentration after cataract surgery
Introduction
Misalignment of the intraocular lens (IOL) is an important risk factor for the deterioration of visual quality after cataract surgery. Previous studies have found that an IOL tilt greater than 7° or decentration greater than 0.4 mm affects visual quality after IOL implantation by increasing wavefront aberrations, such as astigmatism and high-order aberrations (HOA) (1-3). Especially for toric and multifocal IOLs, their optical performances were more sensitive to tilt and decentration. Tilt and decentration may cause fewer predictable astigmatisms for toric IOLs and induce larger comas for multifocal IOLs (4-7). To achieve better postoperative visual quality, it is necessary to understand the main factors that contribute to IOL tilt and decentration after cataract surgery.
Scheimpflug photography, Purkinje images, and anterior segment optical coherence tomography (AS-OCT) have been used in the past to measure the tilt and decentration of IOLs (8-13). However, none of the above methods can measure the tilt and decentration of crystalline lenses and IOLs automatically, which need to be combined using image processing software. The accuracy and repeatability of measurements therefore depend on the alignment and quality of images. CASIA2, a novel second generation of AS-OCT, has been demonstrated to measure the tilt and decentration of crystalline lenses and IOLs automatically and quantitatively with high repeatability (14). It can clearly outline the crystalline lens or IOL and generate three-dimensional (3D) results of tilt and decentration using the visual line as a reference. Compared with the pupil center, the visual line is considered a better reference for assessing IOL tilt and decentration, because it is not affected by the shape of the pupil.
Although several studies have found that the magnitude and direction of tilt of postoperative IOLs were correlated with the tilt of preoperative crystalline lenses, these results were inconsistent (15,16). Hirnschall et al. reported that the tilt directions of crystalline lenses and IOLs were strongly correlated, while their magnitudes of tilt were more weakly correlated (15). Wang et al. demonstrated that preoperative crystalline lens tilt was strongly correlated with IOL tilt (r=0.707) (16). Moreover, axial length (AL) may be another critical factor that affects the tilt and decentration of crystalline lenses and IOLs. A greater tilt of both crystalline lenses and IOLs has been reported to be associated with shorter AL (16). Furthermore, anterior chamber depth (ACD) and lens thickness (LT) have also been found to be negatively correlated with crystalline lens tilt (16). However, whether crystalline lens decentration is associated with IOL decentration has yet to be established.
In this study, we measured the tilt and decentration of patients’ crystalline lenses and IOLs before and after cataract surgery using CASIA2 and then analyzed their characteristics, identifying the main determinants of IOL tilt and decentration following phacoemulsification with IOL implantation. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-1008).
Methods
Study population and design
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This prospective cohort study was approved by the Institutional Review Board of Zhongshan Ophthalmic Center in Sun Yat-Sen University (Guangzhou, China) (NO.: 2019 KYPJ033) and informed consent was obtained from all patients. A total of 56 patients (56 eyes) that planned to undergo phacoemulsification with IOL implantation between August and September, 2019, at Zhongshan Ophthalmic Center were continuously recruited in this study. Patients with the following conditions were excluded: (I) ocular disease that may affect the function of the suspensory ligament of lens, such as previous ocular trauma, lens subluxation, pseudoexfoliation, or retinal pigment degeneration; (II) previous intraocular surgery; or (III) intraoperative or postoperative complications.
General examinations
Patient data, including age, gender, and medical history, were obtained from the patients’ medical records. AL was measured using IOL Master 700 (Carl Zeiss, Meditec, Dublin, CA, USA) in a dark room following anterior slit-lamp biomicroscopy examination. Nuclear opacities and cortical opacities were graded by two ophthalmologists (XY-C and XX-G) according to the Lens Opacities Classification System III (LOCS III).
AS-OCT examination
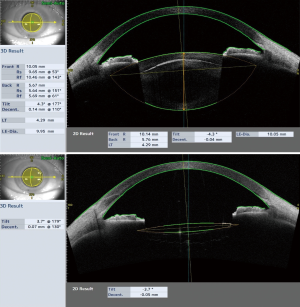
All subjects underwent anterior segment imaging before and 1 week after cataract phacoemulsification with IOL implantation surgery using CASIA2 (TOMEY, Japan) under non-mydriatic conditions. Crystalline lenses and IOLs were measured using the Lens Biometry and IOL Scan modes, respectively. Using the Lens Biometry mode, CASIA2 generated 16 distinct AS-OCT images from 16 different angles of each patient’s crystalline lens (0–180, 11–191, 23–203, 4–214, 45–225, 56–236, 68–248, 79–259, 90–270, 101–281, 113–293, 124–304, 135–315, 146–326, 158–338, and 169–349). Using the IOL Scan mode, 8 distinct AS-OCT images from 8 different angles (0–180, 90–270, 23–203, 113–293, 45–225, 135–315, 68–248, and 158–338) were obtained. The outlines of the crystalline lenses and IOLs were automatically recognized and 3D analyses of tilt and decentration were directly generated by built-in software (Version SS2000) relative to the visual line. The same examiner checked and adjusted the crystalline lens and IOL outlines to ensure tilt and decentration were measured accurately. Examples of 3D results from a crystalline lens and an IOL are shown in Figure 1.
Surgical techniques
All subjects underwent cataract phacoemulsification with IOL implantation surgery after receiving local anesthesia. Each patient received a 2.2 mm temporal corneal incision that was self-sealing. After continuous circular capsulorhexis and cataract phacoemulsification, the patients were implanted with a one-piece hydrophobic IOL (SN60WF, Alcon Laboratories, Texas, USA). All surgeries were performed by two experienced ophthalmologists (YZ-L and LX-L).
Statistical analysis
All statistical analyses were carried out with StataSE15 (version 15.0, Stata Corp LP, TX, USA). All continuous variables were expressed as mean ± standard deviation. Categorical variables were expressed as counts and percentages. A paired-sample t-test was performed to assess tilt and decentration differences between preoperative crystalline lenses and postoperative IOLs. Univariate and multivariate regression analyses were used to determine the correlation of IOL tilt and decentration with preoperative crystalline lenses tilt and decentration, age, gender, presence of diabetes mellitus, AL, and LT. A P value <0.05 was considered statistically significant.
Results
Patients
A total of 56 patients (56 eyes) who finished preoperative and postoperative examinations (1 week after surgery) were recruited in this study. The mean age was 69.25±10.81 years with a range of 28 to 91 years, and 62.5% of the participants were women. The mean AL was 24.27±2.25 mm with a range of 21.38 to 32.27 mm. The basic characteristics of the patients are shown in Table 1.
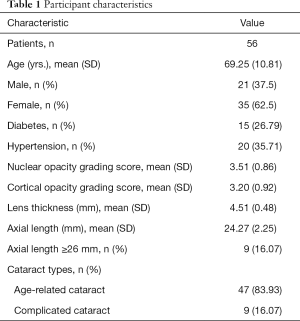
Full table
Tilt and decentration of preoperative crystalline lenses and postoperative IOLs
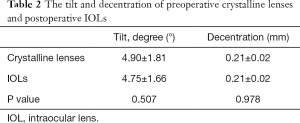
Table 2 shows the mean values of the tilt and decentration of preoperative crystalline lenses and postoperative IOLs relative to the visual line. For the crystalline lenses, the mean magnitude of tilt was 4.90°±1.81° and the mean decentration was 0.21±0.02 mm under non-mydriatic conditions. For the IOLs, the mean magnitude of tilt was 4.75°±1.66° and the mean decentration was 0.21±0.02 mm. No significant difference existed in magnitude of tilt or decentration between preoperative crystalline lenses and postoperative IOLs (P=0.507 and P=0.978, respectively).
Full table
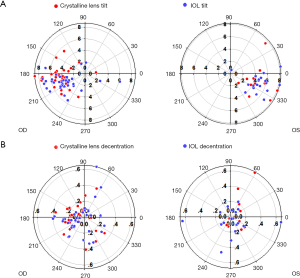
As illustrated in Figure 2, preoperative crystalline lenses and postoperative IOLs were both tilted toward the inferotemporal direction in the right and left eyes. Although the directions of decentration were relatively scattered, more crystalline lenses and IOLs were decentered towards the temporal direction. Additionally, the directions of tilt and decentration for crystalline lenses and IOLs were found to be essentially the same.
Determinants of IOL tilt and decentration
Table 3 shows the univariate and multivariate regression analysis results for IOL tilt and decentration. In the univariate analysis of IOL tilt, the tilt of preoperative crystalline lenses alone had the highest determinate coefficient (R2=0.512, P<0.001), followed by AL (R2=0.154, P=0.003). In the multivariate analysis, a greater IOL tilt was significantly associated with a greater preoperative crystalline lens tilt (P<0.001), thicker lens (P=0.011), and a shorter AL (P=0.033) (Figure 3A). Age, sex, and the presence of diabetes were not significantly associated with IOL tilt. Of the 5 patients with a tilt greater than 7°, 4 also had a crystalline lens tilt greater than 7° before surgery and their average AL (22.82±0.98 mm) was shorter than the overall mean AL (24.27±2.25). These findings indicated that preoperative crystalline lens tilt and shorter ALs were the main determinants of postoperative IOL tilt.
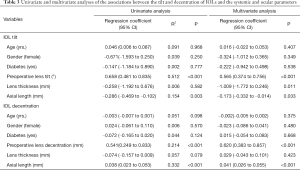
Full table
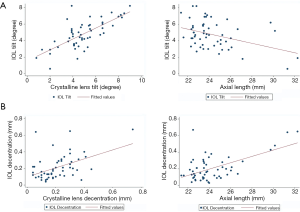
AL was the factor most highly associated with IOL decentration (R2=0.332, P<0.001), rather than preoperative crystalline lens decentration (R2=0.214, P<0.001). AL and crystalline lens decentration explained 54.6% of the variability in IOL decentration. Greater IOL decentration was dramatically associated with longer AL (P<0.001) and greater decentration of preoperative crystalline lenses (P<0.001) (Figure 3B). No correlation existed between IOL decentration and age, gender, the presence of diabetes, or LT. Of the 6 patients with a decentration greater than 0.4 mm, 4 had an AL longer than 29 mm, and the remaining 2 patients already had a crystalline lens decentration greater than 0.4 mm before surgery. These results suggested that IOL decentration is greater in cataract patients with longer ALs and greater decentration of preoperative crystalline lenses.
Discussion
Large misalignments of IOLs can result in the deterioration of postoperative visual quality in pseudophakic patients (17). Previous studies have demonstrated that preoperative crystalline lens tilt can predict postoperative IOL tilt (15). In the current study, using a novel AS-OCT CASIA2 method, we found that preoperative crystalline lenses and postoperative IOLs both tended to tilt approximately 5° towards the inferotemporal direction and shifted 0.21 mm towards the temporal direction. The directions of tilt and decentration for crystalline lenses and IOLs were almost the same. Additionally, greater IOL tilt was significantly associated with greater preoperative crystalline lens tilt, thicker lenses, and shorter ALs. Preoperative crystalline lens tilt was the strongest determinant of IOL tilt, followed by AL. Moreover, we demonstrated for the first time that AL and preoperative crystalline lens decentration were the two most important factors in determining IOL decentration.
Several studies have previously reported that the mean tilt of normal crystalline lenses ranged from 2.85° to 4.6° using magnetic resonance imaging (MRI) or Purkinje images (18-20). Chang et al. reported that crystalline lens tilt was 3.7°±2.5° for the anterior surface and 3.3°±1.4° for the posterior surface, while the horizontal decentration of crystalline lenses was 0.11±0.07 mm and the vertical decentration was 0.06±0.38 mm relative to the corneal axis using MRI 3D-image reconstruction (18). Schaeffel et al. found using Purkinje images that all natural lenses tilted about 4.6° toward the temporal side and decentered approximately 0.3 mm downward relative to the pupil center (19). Findings in another study showed that crystalline lenses decentered 0.25 mm toward the temporal direction and tilted 2.85° toward the inferotemporal direction (20). Kimura et al. were the first to use a second generation AS-OCT (CASIA2, TOMEY) to measure the tilt and decentration of crystalline lenses and IOLs. They found that both crystalline lenses and IOLs had inferotemporal tilts of 4.22–5.30° and temporal decentration of 0.03–0.12 mm (14). The magnitude of tilt and decentration of crystalline lenses and IOLs in our study were greater than that found by some previous studies. We believe the primary reason for this is that the patients enrolled in our study had a greater AL range, being 21.38 to 32.27 mm.
More than 10 years ago, Hu et al. hypothesized that IOL misalignment might be caused by malposition of the crystalline lens (20). In recent years, several studies have reported the relationship between the tilt of crystalline lenses and that of IOLs. Hirnschall et al. reported that the mean tilts of crystalline lenses and IOLs were 4.3° and 6.2°, respectively, using IOL Master 700. A strong correlation was found between the tilt direction of crystalline lenses and that of IOLs (r=0.71), whereas there was a weaker correlation between their magnitudes of tilt (r=0.39) (15). In a larger sample study, Wang et al. found a stronger correlation between preoperative crystalline lens tilt and postoperative IOL tilt (r=0.707) (16). Using CASIA2, we found the mean tilt of crystalline lenses to be 4.9° and the mean tilt of IOLs to be 4.75°, and the tilt of crystalline lenses explained 51.2% of the variability in IOL tilt. These measurements were within the range of previous findings.
However, the correlation between preoperative crystalline lens decentration and that of postoperative IOLs is unclear. In the current study, we found a clear correlation between preoperative crystalline lens decentration and postoperative IOL decentration (R2=0.214, P<0.001), but this correlation was weaker than that found for tilt. Interestingly, AL, rather than preoperative crystalline lens decentration, was the factor most highly associated with IOL decentration (R2=0.332, P<0.001). Greater IOL decentration was dramatically associated with longer AL. A possible explanation is that IOLs are more likely to shift in the loose lens capsular bags of eyes with long ALs. Furthermore, we found that AL was negatively correlated with IOL tilt. This result is consistent with that of a previous study (16). IOLs are therefore more prone to tilt in patients with short ALs. Therefore, the use of toric or multifocal IOLs should be appropriate for cataract patients with long or short ALs.
Our study had some limitations. Firstly, the number of participants was small, meaning the relevance of tilt and decentration between crystalline lenses and IOLs may be underestimated. Secondly, the duration of our study was short, meaning we could not observe the long-term stability of IOLs. Therefore, large-scale and long-term studies are necessary to verify our results.
In conclusion, our study showed that preoperative crystalline lens tilt was the strongest determinant of postoperative IOL tilt, followed by AL. Greater IOL tilt was significantly associated with greater preoperative crystalline lens tilt and shorter AL. AL, rather than crystalline lens decentration, was the factor most highly associated with IOL decentration. Greater IOL decentration was dramatically associated with longer AL and greater preoperative crystalline lens decentration. These findings indicate that the tilt and decentration of postoperative IOLs are greater in patients with more tilted and decentered crystalline lenses, as well as those with shorter or longer ALs.
Acknowledgments
We gratefully acknowledge B. Madden and J. Reynolds for English language editing.
Funding: This study was supported by the National Key R&D Program of China (2017YFC1104603), the National Natural Science Foundation of China (81770905, 81873675), and the Construction Project of High-Level Hospitals in Guangdong Province (303020102).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-1008
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-1008
Peer Review File: Available at http://dx.doi.org/10.21037/atm-20-1008
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-1008). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This prospective cohort study was approved by the Institutional Review Board of Zhongshan Ophthalmic Center in Sun Yat-Sen University (Guangzhou, China) (NO.: 2019 KYPJ033) and informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holladay JT, Piers PA, Koranyi G, et al. A new intraocular lens design to reduce spherical aberration of pseudophakic eyes. J Refract Surg 2002;18:683-91. [PubMed]
- Lawu T, Mukai K, Matsushima H, et al. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye. J Cataract Refract Surg 2019;45:662-8. [Crossref] [PubMed]
- He W, Qiu X, Zhang S, et al. Comparison of long-term decentration and tilt in two types of multifocal intraocular lenses with OPD-Scan III aberrometer. Eye (Lond) 2018;32:1237-43. [Crossref] [PubMed]
- Montés-Micó R, López-Gil N, Pérez-Vives C, et al. In vitro optical performance of nonrotational symmetric and refractive-diffractive aspheric multifocal intraocular lenses: impact of tilt and decentration. J Cataract Refract Surg 2012;38:1657-63. [Crossref] [PubMed]
- Zhu X, He W, Zhang K, et al. Factors influencing 1-year rotational stability of AcrySof Toric intraocular lenses. Br J Ophthalmol 2016;100:263-8. [Crossref] [PubMed]
- Viestenz A, Seitz B, Langenbucher A. Evaluating the eye's rotational stability during standard photography: effect on determining the axial orientation of toric intraocular lenses. J Cataract Refract Surg 2005;31:557-61. [Crossref] [PubMed]
- Liu X, Xie L, Huang Y. Effects of decentration and tilt at different orientations on the optical performance of a rotationally asymmetric multifocal intraocular lens. J Cataract Refract Surg 2019;45:507-14. [Crossref] [PubMed]
- Turuwhenua J. A theoretical study of intraocular lens tilt and decentration on perceptual image quality. Ophthalmic Physiol Opt 2005;25:556-67. [Crossref] [PubMed]
- Crnej A, Hirnschall N, Nishi Y, et al. Impact of intraocular lens haptic design and orientation on decentration and tilt. J Cataract Refract Surg 2011;37:1768-74. [Crossref] [PubMed]
- Wang X, Dong J, Wang X, et al. IOL tilt and decentration estimation from 3 dimensional reconstruction of OCT image. PLoS One 2013;8:e59109. [Crossref] [PubMed]
- Nishi Y, Hirnschall N, Crnej A, et al. Reproducibility of intraocular lens decentration and tilt measurement using a clinical Purkinje meter. J Cataract Refract Surg 2010;36:1529-35. [Crossref] [PubMed]
- Cinar E, Yuce B, Aslan F, et al. Intraocular lens tilt and decentration after Nd:YAG laser posterior capsulotomy: Femtosecond laser capsulorhexis versus manual capsulorhexis. J Cataract Refract Surg 2019;45:1637-44. [Crossref] [PubMed]
- Li L, Wang K, Yan Y, et al. Research on Calculation of the IOL Tilt and Decentration Based on Surface Fitting. Comput Math Methods Med 2013;2013:1-7.
- Kimura S, Morizane Y, Shiode Y, et al. Assessment of tilt and decentration of crystalline lens and intraocular lens relative to the corneal topographic axis using anterior segment optical coherence tomography. PLoS One 2017;12:e184066. [Crossref] [PubMed]
- Hirnschall N, Buehren T, Bajramovic F, et al. Prediction of postoperative intraocular lens tilt using swept-source optical coherence tomography. J Cataract Refract Surg 2017;43:732-6. [Crossref] [PubMed]
- Wang L, Guimaraes De Souza R, Weikert MP, et al. Evaluation of crystalline lens and intraocular lens tilt using a swept-source optical coherence tomography biometer. J Cataract Refract Surg 2019;45:35-40. [Crossref] [PubMed]
- Oshika T, Kawana K, Hiraoka T, et al. Ocular higher-order wavefront aberration caused by major tilting of intraocular lens. Am J Ophthalmol 2005;140:744-6. [Crossref] [PubMed]
- Chang Y, Wu H, Lin Y. The axial misalignment between ocular lens and cornea observed by MRI (I)—At fixed accommodative state. Vision Res 2007;47:71-84. [Crossref] [PubMed]
- Schaeffel F. Binocular lens tilt and decentration measurements in healthy subjects with phakic eyes. Invest Ophthalmol Vis Sci 2008;49:2216. [Crossref] [PubMed]
- Hu CY, Jian JH, Cheng YP, et al. Analysis of crystalline lens position. J Cataract Refract Surg 2006;32:599-603. [Crossref] [PubMed]


