Application of double circular suturing technique (DCST) in repair of giant incision hernias
Introduction
Incisional hernia of the abdominal wall is a common complication after abdominal surgery, in which the occurrence rate reported at 23.8 months was 12.8% in a systematic review and meta-regression study (1-3). It is correlated with the local and systemic factors, including the incision type, suture material and technique, wound infection, obesity, malnutrition, advanced age, diabetes, chronic obstructive lung disease, etc (4-6). Incidence rates up to 69% have been reported in high-risk patients with prospective long-term follow-up (7). The giant incisional hernia of the abdominal wall whose maximal diameter exceeding than 12 cm or the ratio of the volume of hernia sac to abdominal cavity was greater than 20%, was found hard to treat and with a high recurrence rate and more complications (8-10). It was reported the recurrence rate of giant incisional hernia repair of abdominal walls performed by experienced surgeons ranged from 10% to 30%, and the occurrence rate of postoperative complications was as high as 50% (11-13). One of the most challenging problems was that after many contents of hernia returned to the abdominal cavity, postoperative intra-abdominal pressure would increase, resulting in multiple organ dysfunction, then abdominal compartment syndrome (ACS), and even death (14-16). There is currently no agreement reached on the surgical approach for such giant incisional hernias of the abdominal wall. In order to obtion lower recurrence some articles recommend that the hernia mesh should be placed in the sublay or underlay position (17,18). And in order to obtain better mesh augmentation, component separation technique (CST) may be a suitable solution but with a considerable risk of complications and recurrence (2). Underlay mesh implantation can be performed with mesh bridging and mesh augmentation. Therefore, a truly successful giant hernia repair requires effective bridging or augmentation that will prevent recurrence with acceptable risk of complications (17).
We found that a double circular suturing technique (DCST by its initials), which substance is mesh bridging, is very applicable to the repairation of giant incision hernias. Operation points of DCST are discontinuously sling immobilization of the outer ring and continuously suturing fixed method of the inner ring, which will be elaborated in the method section. DCST also can be used in the repair of large abdominal wall defects after resection of abdominal wall tumor, especially for the defects that can not be closed by traditional surgical techinique. We have reported its application in repair defects after abdominal wall tumor resection in journal of Ann Transl Med (19). From January 2010 to December 2018, DCST was applied to treat 221 patients with giant incisional hernia with favorable efficacy in West China School of Medicine, Sichuan University. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-4572). Now it is reported as follows.
Methods
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the institutional research ethics committee of the West China Hospital of Sichuan University. Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
General data
The inclusion criteria of our study is patients with incisional hernia of the abdominal wall whose maximal diameter of hernia defects were exceeding than 12 cm or the ratio of the volume of hernia sac to abdominal cavity was greater than 20%. The exclusion criteria is that the surgical procedure is not DSCT. General data of patients were showen in Table 1.

Full table
Preoperative preparation
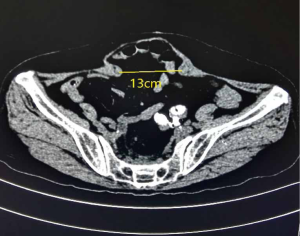
A CT examination was need to confirme preoperative diagnosis which can measure the maximal diameter of hernia defect and calculate the volume ratio of hernia sac to abdominal cavity. A representative CT diagnostic image of giant incision hernia was shown in Figure 1. Patients with respiratory diseases, including bronchitis and emphysema and prostatic hyperplasia, were given medical treatment. Blood pressure and blood glucose are adjusted to normal levels. Patients with coronary heart disease treated with aspirin or clopidogrel suspend for 3–7 days. The laxative was given the day orally before surgery with no routine gastrointestinal decompression. Prophylactic use of antibiotics was routinely given 30 minutes before surgery.
The operation method
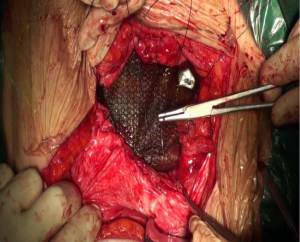
With general anesthesia, the skin and subcutaneous tissue were cut layer by layer along the original incision. After the scar tissue and excess skin of the original incision were removed, the abdominal cavity was approached at the weak part of the hernia sac. The adhesion between the abdominal cavity and the abdominal wall was carefully separated to measure the defect range of the abdominal wall. The patch with the appropriate size would be placed in the defect of the abdominal wall, exceeding the defect range at least 5 cm of the edge of the patch, and the patch was flattened. The double circular suturing technique (DCST) was adopted when the patch fixed. The outer ring was discontinuously sling immobilization surrounding the patch every 3–4 cm and the puncture needle placed close to the edge of the patch, the suture to fix the patch was pulled out of the full-layer abdominal wall by threading the needle, tightened and knotted subcutaneously (shown in Figure 2). The inner ring was sutured with a 2-0 prolene suture and a continuous suture with the actual hernia ring, with a drainage tube placed inside and outside the patch, respectively (shown in Figure 3).

Video of the operation can be found at Video 1.
Postoperative management
The patient’s vital signs were closely checked postoperatively, especially the breath and urine volume, to observe the occurrence of ACS. Gastrointestinal decompression would be conducted if necessary, or ventilator assisted breathing or even decompression by laparotomy. Intravenous antibiotics were continued for one day postoperatively, and the drainage tube would be removed when the volume of drainage was <10 mL/d. The abdominal band would be tied for 3–6 months postoperatively.
Efficacy evaluation
Preoperative preparation time, operating time, postoperative hospital stays, and postoperative complications were recorded. Visual analog scale (VAS) was used to evaluate the incidence of chronic pain of the incision, e.g., 0 cm represented that there was no pain; 10 cm represented that there was intolerable pain.
Results
All the 221 operations were completed successfully. There were no postoperative death cases. Results of patients performed DCST were shown in Table 2. Two of the patients that experienced an intestinal fistula had recovered after they were forbidden to drink and eat, strengthened nutritional support, and continuous negative pressure suction treatment. One of the intestinal fistula had the mesh removed. Two cases of mesh infection patients had the mesh removed. Four of the patients experienced wound infection who underwent wound dressing when the wound reopened, secretions cultured, and strengthened anti-infection treatment and cured afterward. Seven of the patients experienced serum tumescence and cured after aseptic puncture aspiration and pressure dressing by the abdominal band. Three cases of pulmonary infection patients cured after anti-infection treatment. Two cases of wound dehiscence patients underwent wound dressing and suturing and cured afterward. Nine patients recurred and received reoperations. Fourteen patients occurred chronic pain after six months whose VAS was 2–4 cm with activity, with an average of 2.7 cm.

Full table
Discussion
Once a giant abdominal incision hernia occurs, it cannot heal itself and will increase further with the extension of time, and the only effective treatment is surgery (20). We should pay attention to prevent the postoperative ACS for the repair of giant incisional hernia (21). It is presumed to be necessary to improve the abdominal wall compliance of patients with giant incisional hernia preoperatively to reduce the possibility of ACS (22). It was reported abroad that progressive preoperative pneumoperitoneum (PPP) was used to treat hernia with giant volume, and the biocompatibility was enhanced when hernia contents back to the abdominal cavity, to be sufficiently repaired (23). However, some complications may happen, including subcutaneous emphysema, intraabdominal hemorrhage, and intraabdominal organ injury (24). While in China, the local compression method was commonly adopted when returning the hernia contents to the abdominal cavity, and it may take 2–3 weeks to prepare preoperatively, or even longer. Among the 221 patients with giant incisional hernia repaired by DCST, no PPP and few abdominal compressions were done preoperatively, which significantly decreased the preoperative waiting time and potential complications during the preoperative preparation time. The average preparation time before the operation was 3.7 days, with a range of 1–6 days, and there was no ACS after surgery. DCST is a low-tension herniorrhaphy method avoiding direct suture of the hernia ring, showing that the surgical method can effectively prevent postoperative ACS.
Nowadays, there are many ways to repair the giant abdominal incisional hernia (2,9,21,23). The key to being solved in the procedure of giant incisional hernia on the abdominal wall is to treat the protruding organ tissues in the hernia sac and repair the giant abdominal wall defect. As for the treatment, when the hernia ring could not be closed due to the giant defect are as follows: (I) the component separation technique (CST), adapted for the defect at the midline of the abdominal wall, can expand the volume of the abdominal cavity, maintain the compliance of the abdominal wall, and can be used for contaminated wounds. However, the procedures are complicated, with a giant separation surface and many postoperative complications. It was reported the incidence rate of postoperative complications of the repair of incisional hernia or defect used by CST was 23.8%, of which the most common, the incidence rate of incision infection was 18.9%, serum tumescence and hematoma were both 2.4%, and skin flap necrosis was 1.5%. The recurrence rate ranged from 9.1% to 32% (25-27). (II) Autologous tissue transplantation. The materials of autologous tissue, including fascia lata, the anterior sheath of rectus abdominis, and gracilis muscle, are convenient to obtain, with low cost, favorable tissue compatibility, and strong tolerance to infection. However, it may result in prolonged operation time, damage to normal body tissues, affecting the appearance and function of the sampling sites, a giant trauma and prone necrosis, and infection of the graft material, which often leads to the failure of the operation and the recurrence (28,29). (III) Initiative content reduction surgery. The initiative content reduction is the active removal of non-necrotic hernia contents, including omentum, adhesive bowels, and related mesenteries, in the repair of incisional hernia to reduce the contents of the abdominal cavity and avoid the occurrence of postoperative ACS (18,27). At present, it is still controversial whether to adopt initiative content reduction for giant incisional hernia. There is no such evidence on whether the resection of bowels may decrease the intra-abdominal pressure and reduce the potential of ACS occurrence at home and abroad. There would be a considerable risk of intraoperatively and postoperatively. The surgical indications should be observed in the repair of giant incisional hernia used by an initiative content reduction to avoid serious postoperative complications.
Giant abdominal incisional hernia treated with DCST may have benefits as follows: (I) the preoperative preparation only takes a short period, and the preparation of abdominal band compression and artificial pneumoperitoneum are not necessary. The only need is to complete the preoperative examination and get the intestine prepared the day before the operation; (II) the procedures are simple, and with short duration and minor trauma. The operation time ranged from 43–195 min, with an average of 83 min, which was much shorter than CST or initiative content reduction surgery or autologous tissue repair (2,28,30); (III), rapid postoperative recovery. The patients did not receive routine gastrointestinal decompression and took fluids the first day after surgery to reduce the time of gastrointestinal function recovery. The average postoperative hospital length of stay was 7.5 days, with a range of 2–16 days; (IV) low occurrence of postoperative complications. Only 6 patients (2.7%) recurred after the operation; (V) wide adaptability. It cannot only be used for giant incisional hernia of the abdominal wall but also giant defects after abdominal tumor resection and hernia in particular parts of whose ring could not be closed due to the poor tissue mobility.
When performed DCST, it should be noted that: (I) both sharp and blunt dissection should be conducted combinedly and it would rather wound the abdominal wall than the bowels; (II) the patch can be trimmed to form the patch flat. The edge of the patch ought to be at least 5 cm away from the ring of the hernia. A certain tension should be supported to avoid over relaxation; (III) when fixing the patch at the outer ring, flatting the patch is proper. The outer ring surrounding the patch every 3–4 cm and the needle placed close to the edge of the patch, the suture to fix the patch should be knotted subcutaneously; (IV) while suturing the patch at the inner ring continuously, the depth of needle inserting must be shallow to prevent the damage to the bowels underneath. The hernia ring should be sutured near the center of the patch and tighten the suture to shrink the hernia ring; (V) negative pressure sucks, and a closed drainage tube should be placed at the deep and superficial surface of the patch. Negative pressure drainage can effectively remove the blood and effusion in the incision and subcutaneously, causing the patch, skin, and tightly bonded peritoneum to ensure the incision heals and low incidence rate of infection. However, there are some defects in the procedure, as follows: (I) the size of the patch is a little bit giant and expensive; (II) because the texture of the patch is soft, when the defect of the abdominal wall is substantial, the patch may bulge out; (III) in local severe pollution conditions, the non-absorbable material repair is not recommended (31,32).
In conclusion, DCST in the repair of giant incisional hernia of the abdominal wall is straightforward to operate, and with low complications and recurrence rate. It can be recommended when the hernia ring cannot be closed.
Acknowledgments
Funding: The National Natural Science Foundation of China (Grant No. 71804117).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-4572
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-4572
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-4572). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional research ethics committee of the West China Hospital of Sichuan University. Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Muysoms FE, Antoniou SA, Bury K, et al. European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 2015;19:1-24. [Crossref] [PubMed]
- Cornette B, De Bacquer D, Berrevoet F. Component separation technique for giant incisional hernia: a systematic review. Am J Surg 2018;215:719-26. [Crossref] [PubMed]
- Yang X, Aihemaiti M, Zhang H, et al. Mesh-preservation approach to treatment of mesh infection after large incisional ventral hernia repair—how I do it. Ann Transl Med 2019;7:698. [Crossref] [PubMed]
- Seo GH, Choe EK, Park KJ, et al. Incidence of clinically relevant incisional hernia after colon cancer surgery and its risk factors: a nationwide claims study. World J Surg 2018;42:1192-9. [Crossref] [PubMed]
- Sneiders D, Yurtkap Y, Kroese LF, et al. Risk Factors for Incarceration in Patients with Primary Abdominal Wall and Incisional Hernias: A Prospective Study in 4472 Patients. World J Surg 2019;43:1906-13. [Crossref] [PubMed]
- Henriksen NA, Helgstrand F, Vogt KC, et al. Risk factors for incisional hernia repair after aortic reconstructive surgery in a nationwide study. J Vasc Surg 2013;57:1524-30. [Crossref] [PubMed]
- Alnassar S, Bawahab M, Abdoh A, et al. Incisional hernia postrepair of abdominal aortic occlusive and aneurysmal disease: five-year incidence. Vascular 2012;20:273-7. [Crossref] [PubMed]
- Muysoms F E, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia 2009;13:407-14. [Crossref] [PubMed]
- Clay L, Stark B, Gunnarsson U, et al. Full-thickness skin graft vs. synthetic mesh in the repair of giant incisional hernia: a randomized controlled multicenter study. Hernia 2018;22:325-32. [Crossref] [PubMed]
- Jensen KK, Backer V, Jorgensen LN. Abdominal wall reconstruction for large incisional hernia restores expiratory lung function. Surgery 2017;161:517-24. [Crossref] [PubMed]
- Azar FK, Crawford TC, Poruk KE, et al. Ventral hernia repair in patients with abdominal loss of domain: an observational study of one institution’s experience. Hernia 2017;21:245-52. [Crossref] [PubMed]
- Jensen KK, Brondum TL, Harling H, et al. Enhanced recovery after giant ventral hernia repair. Hernia 2016;20:249-56. [Crossref] [PubMed]
- Slater NJ, van Goor H, Bleichrodt RP. Large and complex ventral hernia repair using “components separation technique” without mesh results in a high recurrence rate. Am J Surg 2015;209:170-9. [Crossref] [PubMed]
- Patel NG, Ratanshi I, Buchel EW. The best of abdominal wall reconstruction. Plast Reconstr Surg 2018;141:113e-36e. [Crossref] [PubMed]
- Bittner R, Bain K, Bansal VK, et al. Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—Part A. Surg Endosc 2019;33:3069-139. [Crossref] [PubMed]
- Kirkpatrick AW, Nickerson D, Roberts DJ, et al. Intra-abdominal hypertension and abdominal compartment syndrome after abdominal wall reconstruction: quaternary syndromes? Scand J Surg 2017;106:97-106. [Crossref] [PubMed]
- Eriksson A, Rosenberg J, Bisgaard T. Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia 2014;18:31-8. [Crossref] [PubMed]
- de Vries Reilingh TS, van Goor H, Charbon JA, et al. Repair of giant midline abdominal wall hernias: ‘‘components separation technique’’ versus prosthetic repair. World J Surg 2007;31:756-63. [Crossref] [PubMed]
- Song YH, Huang WJ, Yan YT, et al. Application of double circular suturing technique (DCST) in the repair of large abdominal wall defects after resection of abdominal wall tumor. Ann Transl Med 2020;8:367. [Crossref] [PubMed]
- Liang MK, Holihan JL, Itani K, et al. Ventral hernia management. Ann Surg 2017;265:80-9. [Crossref] [PubMed]
- Yang S, Chen J, Shen YM, et al. Retrospective research on initiative content reduction technique for obesity patients with huge abdominal incisional hernia. Int J Abdom Wall Hernia Surg 2018;1:19.
- Chandra R, Jacobson RA, Poirier J, et al. Successful non-operative management of intraabdominal hypertension and abdominal compartment syndrome after complex ventral hernia repair: a case series. Am J Surg 2018;216:819-23. [Crossref] [PubMed]
- Oprea V, Matei O, Gheorghescu D, et al. Progressive preoperative pneumoperitoneum (PPP) as an adjunct for surgery of hernias with loss of domain. Chirurgia (Bucur) 2014;109:664-9. [PubMed]
- López Sanclemente MC, Robres J, López Cano M, et al. Progressive preoperative pneumoperitoneum in patients with giant hernias of the abdominal wall. Cir Esp 2013;91:444-9. [Crossref] [PubMed]
- de Vries Reilingh TS, van Goor H, Rosman C, et al. “Components separation technique” for the repair of large abdominal wall hernias. J Am Coll Surg 2003;196:32-7. [Crossref] [PubMed]
- Ko JH, Wang EC, Salvay DM, et al. Abdominal wall reconstruction: lessons learned from 200 “components separation” procedures. Arch Surg 2009;144:1047-55. [Crossref] [PubMed]
- Ewart CJ, Lankford AB, Gamboa MG. Successful closure of abdominal wall hernias using the components separation technique. Ann Plast Surg 2003;50:269-73; discussion 273-4. [Crossref] [PubMed]
- de Vries Reilingh TS, Bodegom ME, Van Goor H, et al. Autologous tissue repair of large abdominal wall defects. Brit J Surg 2007;94:791-803. [Crossref] [PubMed]
- Fong HC, Tan BK, Chow PKH, et al. The Use of Bilayered Fascia Lata With an Interpositional Omental Flap for Autologous Repair of Contaminated Abdominal Fascial Defects. Ann Plast Surg 2017;79:486-9. [Crossref] [PubMed]
- Yang S, Shen Y, Zou Z, et al. Retrospective study of initiative content reduction on prevention of postoperative intra-abdominal hypertension in herniorrhaphy of obese patients with giant ventral hernia. Int J Clin Exp Med 2018;11:8164-9.
- Kanters AE, Krpata DM, Blatnik JA, et al. Modified hernia grading scale to stratify surgical site occurrence after open ventral hernia repairs. J Am Coll Surg 2012;215:787-93. [Crossref] [PubMed]
- Hodgkinson JD, Maeda Y, Leo CA, et al. Complex abdominal wall reconstruction in the setting of active infection and contamination: a systematic review of hernia and fistula recurrence rates. Colorectal Dis 2017;19:319-30. [Crossref] [PubMed]