Retrograde transcatheter closure of ventricular septal perforation after acute myocardial infarction: a case report
Introduction
Ventricular septal perforation is a rare but a serious complication of acute myocardial infarction (AMI), and it has high mortality. Without effective treatment, the 1-month mortality rate exceeds 50%, and the 3-month survival rate does not exceed 10% (1). Both surgical procedures and transcatheter closure can effectively treat ventricular septal perforation. The short-term and long-term prognosis after surgery are similar, but interventional surgery is more convenient (2,3). The traditional approach used for interventional surgery is from the left femoral artery through the perforation of the interventricular septum to the right femoral vein. This approach is long and tortuous and requires the use of loach guidewires, which may cause myocardial damage due to their insufficient tension and difficult placement through the delivery sheath (4). In this case, we performed retrograde transcatheter closure of the ventricular septal perforation. A 26-mm occluder was successfully placed to close the ventricular septal muscular perforation. Left ventricular angiography showed only a small amount of residual shunting immediately after surgery. The approach used for the delivery system is as follows: right femoral vein-inferior vena cava-right atrium-right ventricle-ventricular septal perforation-left ventricle-descending aorta. The Lunderquist exchange guidewire was introduced to allow entry of the delivery sheath with sufficient tension. The procedure went smoothly, and the duration of the operation was 56 minutes, which is significantly shorter than the average operative time of 100 minutes in the past (4).
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-4014).
Case presentation
A 68-year-old woman was admitted to the hospital on September 23, 2019, due to chest pain for 3 hours and was diagnosed with AMI. She had a history of hypertension for 11 years; the highest blood pressure reading was 204/116 mmHg. She was on long-term treatment with amlodipine (5 mg, qd), benazepril (10 mg, qd), and atorvastatin (20 mg, qd). Her blood pressure was controlled at 140/80 mmHg.
Clinical findings
The patient’s blood pressure was 110/60 mmHg on admission. A III/6 systolic murmur was audible at the left sternal border in the 3–4 intercostal space. Electrocardiogram showed acute anterior myocardial infarction, and bedside ultrasound showed ventricular septal perforation. Her lab test showed a cardiac troponin T (cTnT) level of 17.9 µg/L and an N-terminal pro b-type natriuretic peptide (NT-proBNP) level of 1,492.5 µg/L.
Timeline
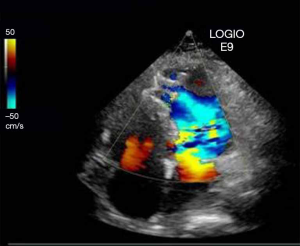
On September 23, 2019, the patient was admitted to the coronary care unit (CCU) due to chest pain for 3 hours and was diagnosed with AMI. The bedside cardiac ultrasound showed ventricular septum perforation (6 mm in diameter).
On September 30, 2019, she was in stable condition. Coronary angiography showed severe stenosis in the middle segment of the left anterior descending branch. A drug-eluting stent was implanted. Bedside color Doppler ultrasound showed interventricular septal perforation (8 mm in diameter).
On October 10, 2019, the patient complained of shortness of breath with even slight movements at the bedside, and bedside color Doppler ultrasound indicated a ventricular septal perforation with a diameter of 12 mm.
On October 17, 2019, the patient’s shortness of breath worsened, and a V/6 systolic murmur was audible at the left sternal border in the 3–4 intercostal space. Her blood pressure was 90/50 mmHg. An IABP was implanted after she was transferred to the intensive care unit.
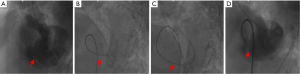
On October 18, 2019, we performed retrograde transcatheter closure of the ventricular septal perforation under local anesthesia. A 26-mm occluder was successfully placed to close the ventricular septal muscle perforation. Left ventricular angiography immediately after surgery showed only a small amount of residual shunting (Figure 1). The patient’s condition improved after surgery, and she was discharged.
Diagnostic assessment
After admission, the patient’s cTnT level gradually increased to a maximum of 29.7 µg/L on October 8, 2019, and her NT-proBNP level gradually increased to a maximum of 11,038.6 µg/L on October 17, 2019. Auscultation showed a gradually increasing grade of systolic rough murmurs in the left sternal border in the 3–4 intercostal space. Color Doppler ultrasound indicated gradual enlargement of the ventricular septal perforation. Based on the above-presented findings, the diagnosis was confirmed: (I) acute anterior septal myocardial infarction with ventricular septal perforation; and (II) hypertension grade; (III) the patient was at extremely high risk, and her prognosis was considered extremely poor.
Therapeutic intervention
After admission, aspirin (100 mg, qd), clopidogrel (75 mg/qd) and low molecular weight heparin (5,000 U, twice a day) were administered for anticoagulation according to guidelines, and the regimen was adjusted according to the patient’s blood pressure level. On October 18, 2019, we performed retrograde transcatheter closure of the ventricular septal perforation. A 26-mm occluder was successfully placed to close the ventricular septal muscle perforation. Left ventricular angiography showed only a small amount of residual shunting immediately after surgery. The delivery system used the following approach: right femoral vein-inferior vena cava-right atrium-right ventricle-ventricular septal perforation-left ventricle-descending aorta. The Lunderquist exchange guide wire was introduced with sufficient tension when entering the delivery sheath. The operation was successful. The operation time was 56 minutes, which was significantly shorter than the average operation time of 100 minutes in the past (Figure 2).
Follow-up
On January 18, 2020, the patient returned to the hospital for a follow-up examination. She had no complaints. Echocardiography indicated that the occluder was well positioned and secure, and a residual shunt (2 mm in diameter) at the upper edge of the occluder was noted (Figure 3). The electrocardiogram showed old anterior wall myocardial infarction. Both the cTnT and NT-proBNP levels were within normal limits, and the patient’s blood pressure was 124/68 mmHg. She was instructed to continue using aspirin (100 mg, once a day), clopidogrel (75 mg/once a day), benazepril (10 mg, once a day) and atorvastatin (40 mg, once a day). No major adverse cardiovascular events (MACEs) were reported during the follow-up period.
Discussion
Ventricular septal rupture (VSR) is a rare and catastrophic mechanical complication after AMI, with an incidence of approximately 0.3% to 0.5% (5,6). Surgery has a definite effect on some patients, but postoperative mortality is still high (7). To date, transcatheter device closure has become an effective method for the treatment of VSR due to its minimal invasiveness and safety (8). The key to the success of the operation is to create a delivery system. The traditional delivery system used in interventional surgery enters at the left femoral artery and progresses through the interventricular septum perforation to the right femoral vein. This approach is long and tortuous and requires the use of loach guidewires, which may cause myocardial damage due to their insufficient tension and difficulty of placement through the delivery sheath (4,9). In this patient, we attempted to use the retrograde transcatheter closure technique, that is, we used the loach guidewire inserted from the right ventricle to the descending aorta through the ventricular septal perforation. The delivery system took the following approach: right femoral vein-inferior vena cava-right atrium-right ventricle-ventricular septal perforation-left ventricle-descending aorta. The Lunderquist exchange guidewire was introduced to allow entry into the delivery sheath with sufficient tension. The procedure went smoothly, and the duration of the operation was 56 minutes, which is significantly shorter than the average operation time of 100 minutes in the past. This technique is beneficial for restoring hemodynamic stability as quickly as possible. In summary, retrograde transcatheter closure is a feasible procedure for closing interventricular septal perforations. This procedure simplifies the previous steps involved in capturing the guidewire and creating the delivery system. It reduces the risk of the guidewire entering the tricuspid tendon, enhances the tension of the guidewire, and reduces the risk and operation time. The procedure is simpler and safer than previous methods, and its application is easier to extend.
Patient perspective
The patient complained of shortness of breath and chest tightness after admission. Upon examination, the physician found that the perforation of the interventricular septum had gradually increased. After the patient’s condition deteriorated, the physician placed an IABP in a timely manner and then performed retrograde transcatheter closure of the ventricular septal perforation. The patient’s symptoms were noticeably relieved immediately after surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-4014
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-4014). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Goldsweig AM, Wang Y, Forrest JK, et al. Ventricular septal rupture complicating acute myocardial infarction: Incidence, treatment, and outcomes among medicare beneficiaries 1999-2014. Catheter Cardiovasc Interv 2018;92:1104-15. [Crossref] [PubMed]
- Takahashi H, Arif R, Almashhoor A, et al. Long-term results after surgical treatment of postinfarction ventricular septal rupture. Eur J Cardiothorac Surg 2015;47:720-4. [Crossref] [PubMed]
- Yam N, Au TW, Cheng LC. Post-infarction ventricular septal defect: surgical outcomes in the last decade. Asian Cardiovasc Thorac Ann 2013;21:539-45. [Crossref] [PubMed]
- Sabiniewicz R, Huczek Z, Zbroński K, et al. Percutaneous Closure of Post-Infarction Ventricular Septal Defects-An Over Decade-long Experience. J Interv Cardiol 2017;30:63-71. [Crossref] [PubMed]
- Jones BM, Kapadia SR, Smedira NG, et al. Ventricular septal rupture complicating acute myocardial infarction: a contemporary review. Eur Heart J 2014;35:2060-8. [Crossref] [PubMed]
- Ng R, Yeghiazarians Y. Post myocardial infarction cardiogenic shock: a review of current therapies. J Intensive Care Med 2013;28:151-65. [Crossref] [PubMed]
- Wilson WM1, Horlick EM. Management of post-myocardial infarction ventricular septal rupture. EuroIntervention 2016;12 Suppl X:X18-X23.
- Zhong W, Liu Z, Fan W, et al. Cardiac MRI-guided interventional occlusion of ventricular septal rupture in a patient with cobalt alloy stent. Ann Transl Med 2019;7:395. [Crossref] [PubMed]
- Tai S, Tang JJ, Tang L, et al. Management and outcome of ventricular septal rupture complicating acute myocardial infarction: what is new in the era of percutaneous intervention? Cardiology 2018;141:226-32. [Crossref] [PubMed]