
Sharp recanalization of the brachiocephalic vein occlusion through the external jugular vein in hemodialysis patients
Introduction
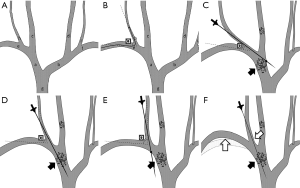
The left and right brachiocephalic veins are a pair of central venous structures formed by the union of the corresponding internal jugular vein (IJV) and the subclavian vein at the level of the sternoclavicular joint. The brachiocephalic veins merge to form the superior vena cava (SVC), the final passage of venous blood from the upper body (Figure 1). In patients treated with chronic hemodialysis, brachiocephalic vein occlusion is a common type of central venous occlusion (CVO), which can lead to ipsilateral limb swelling, altered vascular access function, and subsequent suboptimal hemodialysis (1). Brachiocephalic vein occlusion was traditionally treated with complex bypass surgery. In recent years, the majority of the cases are treated with traditional blunt angioplasty recanalization (2,3); however, when this fails, optional treatments include sharp transversal by a sharp device (4-6), radiofrequency recanalization (7) or outback reentry devices (8). IJV is one of the puncture sites most widely used for both hemodialysis catheter insertion and CVO angioplasty (9). When the IJV is obstructed, alternative vascular access, such as through the external jugular vein (EJV), may be considered (10,11). Compared with a brachial or femoral approach, the EJV holds the advantage of being adjacently located in a straight line to the brachiocephalic vein, which might enable using a straight sharp device during recanalization with better over-the-wire control. However, the utilization of EJV as access site when performing CVO sharp recanalization has seldom been reported. The present study aimed to describe the efficacy and safety of sharp recanalization for brachiocephalic vein occlusion through the EJV in hemodialysis population. To our knowledge, this is the first clinical observation among a cohort of hemodialysis patients utilizing this technique.
Methods
Study subjects
This study retrospectively enrolled consecutive chronic hemodialysis patients who received sharp recanalization of the brachiocephalic vein through EJV in West China Hospital from January 2017 to December 2018. The inclusion criteria were as follows: (I) on maintenance hemodialysis; (II) diagnosed with brachiocephalic vein occlusion and ipsilateral IJV occlusion; (III) occlusive brachiocephalic lesions were refractory to standard recanalization procedures; and (IV) received sharp recanalization of the brachiocephalic vein occlusion through the EJV. Patients with whom the brachiocephalic vein occlusion was sharply recanalized from the opposite side of the lesion through the SVC were excluded from the analysis.
Sharp recanalization technique
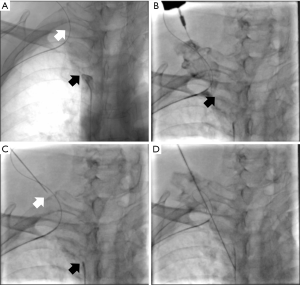
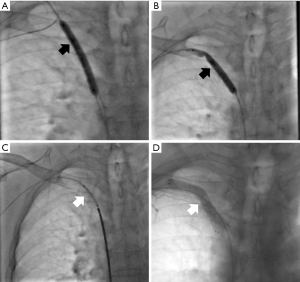
Recanalization was carried out by experienced interventional nephrologists under procedural sedation with fentanyl and midazolam. The brachial and common femoral veins were accessed under aseptic conditions, guided by ultrasound. Fluoroscopy was then performed to document the obstruction (Figure 2A). An attending interventional radiologist measured the length of occlusive segments using digital subtraction venography. If the occlusion could not be passed by blunt recanalization after multiple attempts from either end, then the patient then received sharp recanalization after informed consent was obtained. With the IJV occluded, venography was performed from the brachial approach to visualize the EJV and subclavian vein (Figure 2B). A guide wire was advanced from the brachial access into EJV by way of subclavian vein. The angle formed by the guide wire segments in the EJV and subclavian vein represents the E-S angle (Figure 1). When the operator determined that the E-S angle was suitable, sharp recanalization via the EJV was considered. The EJV was accessed, and a target was placed at the lower end of the obstructive lesion (Figure 2C). The needle of a 5-F Input Introducer Sheath (Medtronic, Minneapolis, MN, USA) (Figure 2D) was used to cross the occlusion, and the path of the needle was guided by multiple orthogonal fluoroscopic projections. Once the needle had crossed the lesion, venography was performed to rule out extravasation. The lesion was primarily dilated with a 6-mm balloon (Cordis, Milpitas, CA, USA) (Figure 3A). A guidewire was inserted into the EJV from the femoral approach and then snared from a brachial approach, establishing a femoral-brachial pull-through. The occlusive lesion was further sequentially dilated with balloons of various sizes (Cordis) (Figure 3B) with a covered fluency stent placed (Bard; Murray Hill, NJ, USA) (Figure 3C). The balloons and stents were sized based on the diameter measured by contrast venography.
Follow-up and outcomes
The patients’ demographic information and clinical outcomes, including technical success, complications, and patency were recorded. The technical success was defined as successful sharp recanalization of brachiocephalic vein through EJV followed by balloon angioplasty and stent placement, with the restoration of antegrade flow by DSA (Figure 3D). Given that chronic hemodialysis patients are heparinized during each treatment session, we didn’t routinely prescribe anticoagulation therapy for this patient cohort. Follow-up tests include vascular ultrasonography in patients with increased venous pressure (>150 mmH2O) during hemodialysis, or CT angiography for patients with limb swelling or decreased subclavian vein blood flow by ultrasound. When imaging tests were not available, brachiocephalic vein patency was clinically defined as the absence of limb swelling/pain or fistula dysfunction. Follow-up information was collected from the outpatient medical record database, hemodialysis database, or by telephone calls. The study received approval from the institutional ethics committee and complied with the Declaration of Helsinki. Informed consent was obtained from all participants.
Statistical analysis
Continuous measurement data were expressed as the mean ± standard deviation. Categorical data were expressed as percentages. Calculations of mean values, standard deviations, and percentages were performed with Excel statistical spreadsheet software (Microsoft; Redmond, WA, USA).
Results
Patient characteristics
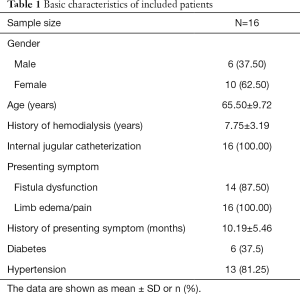
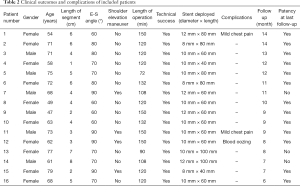
During the study period, we encountered 20 patients with right brachiocephalic vein occlusion that required sharp recanalization and was accompanied IJV occlusion. In 4 patients, venography indicated an E-S angle <45°, which was considered to be unsuitable for sharp recanalization through the EJV (as illustrated in Figure 1). Therefore, they were subjected to retrograde trans-septal needle sharp transversal through the SVC. A total of 16 patients who received sharp recanalization through the EJV were included in the final analysis. The mean age of the included patients was 65.50±9.72 years (range, 47–79 years), and 10 (62.50%) were female and 6 (37.50%) were male. The patients had received maintenance hemodialysis for an average of 7.75±3.19 years (range, 3–15 years). All of the patients had a history of previous IJV catheterizations. The patients had presented with arteriovenous fistula dysfunction and limb edema/pain for an average of 10.19±5.46 months (range, 1–22 months). None of the patients were on oral antiplatelet or anticoagulant drugs. Patient characteristics are summarized in Table 1.
Full table
Technical success
The obstructing segments had a mean length of 4.38±1.93 cm (range, 1 to 8 cm). The sharp recanalization procedure was successfully performed to restore the antegrade flow in all 16 patients, resulting in a technique success rate of 100% with a mean operation time of 122.63±22.01 minutes. Twelve patients (75%), whose E-S angles ranged between 60° and 80°, were successfully recanalized through the EJV on the first attempt. For the remaining 4 patients (25%), the puncture was difficult to perform due to the draining of the EJV into the subclavian vein at an almost right angle. This problem was resolved by elevating the patient’s ipsilateral shoulder to decrease the E-S angle, therefore aligning the course of the EJV with the medial part of the subclavian and brachiocephalic veins (Figure 1).
Clinical outcomes and adverse events
As shown in Table 2, a total of 16 covered self-expanding stents, ranging from 8 to 12 mm in diameter and 40 to 120 mm in length, were deployed in 16 patients. No contrast extravasation was revealed in any of the patients by repeated contrast venography during graded dilation and at the end of the procedure. After the procedure, the patients’ limb swelling and pain were ameliorated. Postoperative ultrasonography suggested that the fistula flow rates among the patients ranged from 700 to 1,000 mL/min, providing satisfactory extracorporeal circuit flow for dialysis.
Full table
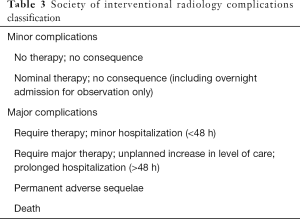
According to the Society of Interventional Radiology (SIR) classification (12) (Table 3), no major complications were recorded. Three minor complications (type B) were noted: 1 patient (a 62-year-old female) experienced blood oozing continuously from the EJV puncture site, which was stopped by application of sustained manual pressure and subsequent compression dressing for 12 hours; and 2 other patients (a 73-year-old male and a 54-year-old female) experienced mild chest pain that was attributed to vascular dilation and stenting, both of whom were relieved with oral non-steroid anti-inflammatory drugs (celecoxib 200 mg qd).
Full table
Follow-up
After surgery, the patients were followed up for a mean time of 10.00±2.53 months (range, 6–14 months). Because only 2 patients underwent follow-up vascular imaging tests, vascular patency was clinically defined as the absence of limb swelling/pain or fistula dysfunction. At the last follow-up, 13 brachiocephalic vein reconstructions (81.25%) were patent. No long-term procedure-related complications were recorded in this cohort.
Discussion
In nephrology practice, brachiocephalic vein occlusion is encountered as a central venous complication among hemodialysis patients on a daily basis (13,14). While the mainstream treatment of brachiocephalic vein occlusion is interventional angioplasty, other therapeutic options include surgical bypass, sharp recanalization, radiofrequency recanalization and outback reentry device. Sharp recanalization is a practical strategy to restore central vein patency when the occlusive lesion cannot be treated with blunt guidewire technique (15,16). According to the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines, the EJV can be as an alternative point of access in patients with occlusion of the IJV (9). Similar to the IJV, the location of the EJV, which is adjacent to central venous lesions, is advantageous and allows direct needle puncture or increased over-the-wire control of sharp devices.
We hypothesized that the EJV could serve as an alternative to an occluded IJV as an approach for angioplasty of CVO in selected patients. The present study aimed to reveal the efficacy and safety of sharp recanalization for brachiocephalic vein occlusion through the EJV in a cohort of consecutive hemodialysis patients. According to our observations, a 100% technical success rate was achieved for all 16 patients and no major complications were experienced. In the hands of an experienced practitioner, sharp recanalization through the EJV approach could offer an effective and safe treatment for right brachiocephalic vein occlusion. To our knowledge, this was the first study focused on the use of EJV as the vascular access for CVO angioplasty.
The EJV starts at the level of the mandible angle, runs vertically down the neck along the posterior border of the sternocleidomastoid muscle, and terminates at the subclavian vein (17). The EJV is tortuous and presents difficulty for cannulation. However, in patients with occlusion of central veins, the EJV may appear dilated, making it easier to puncture. At its distal end, the EJV usually turns medially and directs toward the midline to join the subclavian vein (18). The E-S angle determines whether the EJV is in alignment with the brachiocephalic vein, which makes sharp needle recanalization through the EJV possible.
Among the 20 patients we encountered, 4 had E-S angles of less than 45°. Therefore, the direction of the needle that was advanced through the EJV was too close to the transverse plane to enter the brachiocephalic vein; subsequently, these patients underwent another recanalization strategy. In another 4 patients whose E-S angles were almost 90°, the direction of the puncture needle was too close to the sagittal plane to enter the brachiocephalic vein. In these cases, the patient’s shoulder was then elevated to successfully align the course of the EJV with the brachiocephalic vein during sharp recanalization. For the remaining 12 patients who were successfully recanalized on the first attempt, we determined that E-S angles between 60° and 80° were best suited for sharp recanalization through the EJV.
Practitioners need to be aware that sharp recanalization through the EJV carries all the risks associated with needle revascularization, including extravasation and injury of the adjacent structures (19). For long-segment CVO, the lesion usually involves more than 1 segment of central veins. The obstruction, not surprisingly, could be curved at the junctions between different vessels, which make sharp recanalization more risky, especially when an atypical site like EJV is accessed. Additionally, the “shoulder elevation” maneuver carried out to assist with the puncture requires a more sophisticated collaboration between the interventionist and the assistant for the shoulder to be properly fixed. Strict eligibility screening (E-S angle, length of lesion) and skillful surgery are essential in applying this technique and minimizing the potential risk of adverse events.
Three minor complications were recorded in this study. One patient suffered from blood oozing from an EJV puncture site, which was successfully managed by compression dressing. Because the EJV is superficially located and not supported by subcutaneous tissue above it, procedures involving the EJV should be performed with care to avoid excessive hemorrhaging. Some researchers have advised against the direct puncture of the vein, instead suggesting that a small track should be created approximately 1 cm laterally away from the vein to avoid severe bleeding (18). Because the EJV can undergo ligation without neurologic significance, the risk carried by EJV cannulation itself is, fortunately, much lower than that for the IJV (17). Since the patients enrolled in this study received heparin anticoagulation during hemodialysis, the heparin dosage and time interval between dialysis and surgery might have influenced the risk of bleeding; however, this was beyond the scope of our current investigation. Future studies are called for to identify the potential risk factors of bleeding episodes during EJV puncture. Two other patients in our study exhibited mild chest pain and were prescribed oral celecoxib. Mild chest pain is usually attributed to balloon dilatation and stent deployment; it frequently occurs in patients who receive angioplastic procedures and, in most cases, can be managed with conservative treatment (16).
Our results should be interpreted within the context of the study’s limitations. First, due to the limited patient volume requiring sharp recanalization through an atypical access site, this was a pilot research with a small sample size. Our observation is to be further verified by studies involving more patients. The lack of a control group and the single-center retrospective nature of this study also limited its strength of evidence. Second, as previously mentioned, most of the patients in our cohort did not receive follow-up imaging tests for vascular patency. The estimation of the patent rate was therefore based on clinical assessments. Third, the patients were followed up for an average of only 10 months, and long-term outcomes need to be reported in the future. It is also important to note that even though we aimed to enroll patients with either left or right brachiocephalic vein occlusion, all of the cases in our study were right sided. The applicability of our findings warrants verification in left brachiocephalic vein occlusions.
In conclusion, sharp recanalization performed by experienced practitioners through the EJV could be an effective and safe procedure for treating right brachiocephalic vein occlusion in hemodialysis patients. The angle formed by the EJV and subclavian vein might provide helpful information for patient selection. Prospective controlled clinical trials with larger patient volume are needed to justify the results of this investigation and to provide additional data on the advantages and disadvantages of different sharp recanalization strategies.
Acknowledgments
We gratefully thank Ms. Sammi Lee for the help to prepare the figures.
Funding: This study was supported by National Natural Science Foundation of China (81700588) and The 1•3•5 Project for Disciplines of Excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (2020HXFH014). The funding sources had no involvement in this study.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-3015
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-3015). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study received approval from the institutional ethics committee and complied with the Declaration of Helsinki. Informed consent was obtained from all participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Malik AK, Bhalla N, Goel A, et al. Percutaneous reconstruction of chronic total occlusion of brachiocephalic vein using transseptal needle in dialysis-dependent patient. Cardiovasc Interv Ther 2016;31:136-9. [Crossref] [PubMed]
- Agarwal AK. Central vein stenosis. Am J Kidney Dis 2013;61:1001-15. [Crossref] [PubMed]
- Toda N, Asada S, Komiya T. Brachiocephalic Vein Occlusion from a Tunneled Hemodialysis Catheter. Intern Med 2019;58:3339-40. [Crossref] [PubMed]
- McDevitt JL, Srinivasa RN, Gemmete JJ, et al. Approach, Technical Success, Complications, and Stent Patency of Sharp Recanalization for the Treatment of Chronic Venous Occlusive Disease: Experience in 123 Patients. Cardiovasc Intervent Radiol 2019;42:205-12. [Crossref] [PubMed]
- Honnef D, Wingen M, Günther RW, et al. Sharp central venous recanalization by means of a TIPS needle. Cardiovasc Intervent Radiol 2005;28:673-6. [Crossref] [PubMed]
- Athreya S, Scott P, Annamalai G, et al. Sharp recanalization of central venous occlusions: a useful technique for haemodialysis line insertion. Br J Radiol 2009;82:105-8. [Crossref] [PubMed]
- Sivananthan G, MacArthur DH, Daly KP, et al. Safety and efficacy of radiofrequency wire recanalization of chronic central venous occlusions. J Vasc Access 2015;16:309-14.
- Brountzos EN, Preza O, Kelekis A, et al. Recanalization of dialysis catheter-related subclavian vein occlusion using a re-entry device: report of two patients. Cardiovasc Intervent Radiol 2011;34:207-11. [Crossref] [PubMed]
- Navuluri R, Regalado S. The KDOQI 2006 Vascular Access Update and Fistula First Program Synopsis. Semin Intervent Radiol 2009;26:122-4. [Crossref] [PubMed]
- Wang P, Wang Y, Qiao Y, et al. A Retrospective Study of Preferable Alternative Route to Right Internal Jugular Vein for Placing Tunneled Dialysis Catheters: Right External Jugular Vein versus Left Internal Jugular Vein. PLoS One 2016;11:e0146411. [Crossref] [PubMed]
- Beigi AA, Sharifi A, Gaheri H, et al. Placement of long-term hemodialysis catheter (permcath) in patients with end-stage renal disease through external jugular vein. Adv Biomed Res 2014;3:252. [Crossref] [PubMed]
- Sacks D, McClenny TE, Cardella JF, et al. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol 2003;14:S199-202. [Crossref] [PubMed]
- Letachowicz K, Kołodziej M, Międzybrodzki K, et al. Tunneled-cuffed catheter implanted into the accessory hemiazygos vein because of occlusion of the left innominate vein. Hemodial Int 2012;16:310-4. [Crossref] [PubMed]
- Koh K, Koh YX, Choke ET, et al. Alternative Strategies for Central Venous Stenosis and Occlusion in Patients Requiring Haemodialysis Access. Ann Acad Med Singapore 2017;46:39-41. [PubMed]
- Zhao Y, Yang L, Mai H, et al. Long-segment central venous occlusion in a hemodialysis patient treated by segmented sharp recanalization strategy: A case report. Medicine (Baltimore) 2019;98:e15208. [Crossref] [PubMed]
- Cohen EI, Beck C, Garcia J, et al. Success Rate and Complications of Sharp Recanalization for Treatment of Central Venous Occlusions. Cardiovasc Intervent Radiol 2018;41:73-9. [Crossref] [PubMed]
- Bechmann S, Kashyap V. Anatomy, Head and Neck, External Jugular Veins. StatPearls. Treasure Island (FL): StatPearls Publishing LLC., 2019.
- Gouda ZE, Emara MM, Elbarbary HS, et al. Studying alternative approaches for placement of cuffed hemodialysis catheters in hemodialysis patients with bilateral internal jugular vein occlusion. J Vasc Access 2019;20:250-9.
- Yang L, Yang L, Zhao Y, et al. The feasibility and safety of sharp recanalization for superior vena cava occlusion in hemodialysis patients: A retrospective cohort study. Hemodial Int 2020;24:52-60. [Crossref] [PubMed]


