
Adjuvant EGFR TKIs in NSCLC harboring EGFR mutations: looking for a consensus way
Epidermal growth factor receptor (EGFR) sensitive mutations are routinely tested in advanced non-small cell lung cancer (NSCLC), with an incidence ranging from 10–15% in non-Asian to 30–50% in Asian patients (1). However, there is not a consensus on whether to test or not surgically resected NSCLCs for EGFR. Recently presented data show a positivity rate of 16% in completely resected NSCLC (2). In this journal Liang et al. reported a 2019 update of consensus on postoperative management of EGFR-mutant lung cancer of Society for Translational Medicine (3).
It is current standard of treatment for resected stage II-IIIA NSCLC patients, to receive adjuvant platinum-based chemotherapy (plus post-operative radiotherapy in pN2), when not received in neoadjuvant setting, with an overall 5% benefit in overall survival (OS) (4). The absolute overall 5-year survival ranged from 73% (IA) to 25% (IIIA), respectively, according to TNM staging (5). The survival advantage is obtained in all-comers NSCLCs, without considering the molecular profile of the resected tumors.
Following the usual clinical development shared by most anti-cancer drugs from advanced to early stage setting, EGFR tyrosine kinase inhibitors (EGFR TKIs) were rapidly moved to investigational adjuvant setting after the practice-changing results obtained in EGFR mutation positive aNSCLC (6-9). To date, six studies have complete results in this setting, with very heterogeneous inclusion criteria, treatment strategies and results (Tables 1,2). In particular, the negative phase III BR.19 (10) and RADIANT (11) trials were including patients unselected for EGFR status to receive EGFR TKI or placebo for 2 years after standard adjuvant treatment when needed. Three studies demonstrating prolonged disease free survival (DFS) with EGFR TKI treatment compared to standard chemotherapy—ADJUVANT (14), EVAN (15), EMERGING (17)—were limited to Chinese patients. In contrast, the non-randomized phase II SELECT trial, also showed positive results in DFS with 2-year erlotinib compared to placebo, following standard adjuvant treatment when needed according to disease stage (16).

Full table
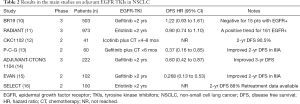
Full table
Looking at data from these trials, all with unavailable or negative OS results, many questions arise on the effective role of adjuvant EGFR TKIs in clinical practice, and no clear consensus has been reached, so far. The first concern is about the position of the EGFR TKI within the adjuvant treatment strategy, whether given alone or with chemotherapy (in association or after). This latter strategy was investigated in the phase II P-C-G trial, demonstrating an increase in DFS with the addition of gefitinib to carboplatin pemetrexed in resected stage IIIA-N2 NSCLC (13). In contrast, a Chinese trial of combined icotinib and platinum based adjuvant treatment in resected stage IB-IIIA NSCLC, failed to show DFS advantage (12).
Another issue to define which could be the optimal duration of adjuvant EGFR-TKI treatment. In the past trials the duration of treatment ranged from 4 months to 2 years, but randomized clinical trials in other diseases (e.g., GIST and breast cancer) have demonstrated a clinical advantage on DFS with the extended regimen (3 or 5 or 10 years) (19,20).
Indeed, a role in neoadjuvant setting may be considered as well, according to stage, as it is for chemotherapy, and preliminary data from phase II trials are available in this setting (21). Another related aspect is the disease stage to consider for adjuvant EGFR: the EVAN trial and the P-C-G trial only included resected stage IIIA patients, representing a population usually undergoing neoadjuvant treatment, while other trials were including also stage I disease, not routinely candidate for adjuvant approaches according to international guidelines (22).
In addition, it is essential to keep in mind that the adjuvant setting concerns disease free patients, whose long-term quality of life (QoL) may be negatively affected by a long-term treatment with EGFR TKIs compared to the time-limited adjuvant chemotherapy. The financial impact of such a long-term treatment, though the exact duration has not reached a consensus, should be also considered. The principal endpoint of all clinical trials in selected EGFR positive NSCLC patients was DFS, and the results of all these trials showed clearly that EGFR TKI can prolong DFS without improving the cure rates, so far all the aspects (optimal duration, which drug, safety profile and QoL) must be considered in this subset of patients. As far as it regards the choice of EGFR TKI for adjuvant treatment, it is important to note that the available data are related to first generation drugs erlotinib, gefitinib and icotinib. No specific information on TKI retreatment is known from the remaining studies save for SELECT trial. In the latter trial, patients received the same EGFR TKI at disease relapse, with a median on-treatment time of 13.1 months (16). These drugs are not corresponding to the current standard of treatment in first-line for EGFR mutant patients, that is the third generation TKI osimertinib. Complicating matters, the actual indication for osimertinib after previous EGFR TKI is conditional on the detection of T790M resistant mutation (23). To the current knowledge, limited information is available, deriving from the SELECT trial, were 60% of relapsing patients underwent rebiopsy, with confirmed EGFR mutation: T790M mutation was identified only in 5% (1 out of 20) of cases (16).
In conclusion, several phase II/randomized trials have been carried out in patients with EGFR positive resected NSCLC: they shared small sample size, included only common EGFR mutations and treatment duration was within 2 years. Overall, no clear indications can be derived from the available studies, where the OS results are negative or immature and only DFS advantage has been obtained (24). Interestingly, disease relapse mainly occurs after the completion of EGFR TKI, suggesting that the use of adjuvant EGFR TKIs may only anticipate the first-line treatment in EGFR mutant NSCLC patients. In this view, the final OS results from the randomized phase III ADAURA trial, evaluating the efficacy of 3-year third generation osimertinib compared to placebo in completely resected stage IB-IIIA EGFR mutant NSCLC patients, are awaited (18).
Acknowledgments
Funding: This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5x1000 funds.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.04.35). Dr. Passaro reports personal fees from Roche, personal fees from BMS, personal fees from MSD, personal fees from Lilly, personal fees from Dako, personal fees from Astra Zeneca, from null, outside the submitted work; Dr. de Marinis reports personal fees from Roche, personal fees from BMS, personal fees from MSD, personal fees from Lilly, personal fees from Dako, personal fees from Astra Zeneca, personal fees from Novartis, personal fees from Takeda, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shigematsu H, Lin L, Takahashi T, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst 2005;97:339-46. [Crossref] [PubMed]
- Oxnard G, Mandrekar S, Hillman S, et al. P1.16-47 Adjuvant Targeted Therapy Following Standard Adjuvant Therapy for Resected NSCLC: An Initial Report from ALCHEMIST (Alliance A151216). J Thorac Oncol 2018;13:S646-7. [Crossref]
- Liang W, Cai K, Chen C, et al. Society for Translational Medicine consensus on postoperative management of EGFR-mutant lung cancer (2019 edition). Transl Lung Cancer Res 2019;8:1163-73. [Crossref] [PubMed]
- Pignon JP, Tribodet H, Scagliotti GV, et al. Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE Collaborative Group. J Clin Oncol 2008;26:3552-9. [Crossref] [PubMed]
- Lim E, Harris G, Patel A, et al. Preoperative versus postoperative chemotherapy in patients with resectable non-small cell lung cancer: systematic review and indirect comparison meta-analysis of randomized trials. J Thorac Oncol 2009;4:1380-8. [Crossref] [PubMed]
- Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. [Crossref] [PubMed]
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. [Crossref] [PubMed]
- Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. [Crossref] [PubMed]
- Ramalingam SS, Vansteenkiste J, Planchard D, et al. Overall Survival with Osimertinib in Untreated, EGFR-Mutated Advanced NSCLC. N Engl J Med 2020;382:41-50. [Crossref] [PubMed]
- Goss GD, O'Callaghan C, Lorimer I, et al. Gefitinib versus placebo in completely resected non-small-cell lung cancer: results of the NCIC CTG BR19 study. J Clin Oncol 2013;31:3320-6. [Crossref] [PubMed]
- Kelly K, Altorki NK, Eberhardt WE, et al. Adjuvant Erlotinib Versus Placebo in Patients With Stage IB-IIIA Non-Small-Cell Lung Cancer (RADIANT): A Randomized, Double-Blind, Phase III Trial. J Clin Oncol 2015;33:4007-14. [Crossref] [PubMed]
- Feng S, Wang Y, Cai K, et al. Randomized Adjuvant Chemotherapy of EGFR-Mutated Non-Small Cell Lung Cancer Patients with or without Icotinib Consolidation Therapy. PLoS One 2015;10:e0140794. [Crossref] [PubMed]
- Li N, Ou W, Ye X, et al. Pemetrexed-carboplatin adjuvant chemotherapy with or without gefitinib in resected stage IIIA-N2 non-small cell lung cancer harbouring EGFR mutations: a randomized, phase II study. Ann Surg Oncol 2014;21:2091-6. [Crossref] [PubMed]
- Zhong WZ, Wang Q, Mao WM, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1-N2) EGFR-mutant NSCLC (ADJUVANT/CTONG1104): a randomised, open-label, phase 3 study. Lancet Oncol 2018;19:139-48. [Crossref] [PubMed]
- Yue D, Xu S, Wang Q, et al. Erlotinib versus vinorelbine plus cisplatin as adjuvant therapy in Chinese patients with stage IIIA EGFR mutation-positive non-small-cell lung cancer (EVAN): a randomised, open-label, phase 2 trial. Lancet Respir Med 2018;6:863-73. [Crossref] [PubMed]
- Pennell NA, Neal JW, Chaft JE, et al. SELECT: A Phase II Trial of Adjuvant Erlotinib in Patients With Resected Epidermal Growth Factor Receptor-Mutant Non-Small-Cell Lung Cancer. J Clin Oncol 2019;37:97-104. [Crossref] [PubMed]
- Zhong WZ, Chen KN, Chen C, et al. Erlotinib Versus Gemcitabine Plus Cisplatin as Neoadjuvant Treatment of Stage IIIA-N2 EGFR-Mutant Non-Small-Cell Lung Cancer (EMERGING-CTONG 1103): A Randomized Phase II Study. J Clin Oncol 2019;37:2235-45. [Crossref] [PubMed]
- Wu YL, Herbst RS, Mann H, et al. ADAURA: Phase III, Double-blind, Randomized Study of Osimertinib Versus Placebo in EGFR Mutation-positive Early-stage NSCLC After Complete Surgical Resection. Clin Lung Cancer 2018;19:e533-6. [Crossref] [PubMed]
- Laurent M, Brahmi M, Dufresne A, et al. Adjuvant therapy with imatinib in gastrointestinal stromal tumors (GISTs)-review and perspectives. Transl Gastroenterol Hepatol 2019;4:24. [Crossref] [PubMed]
- Rossi L, McCartney A, De Santo I, et al. The optimal duration of adjuvant endocrine therapy in early luminal breast cancer: A concise review. Cancer Treat Rev 2019;74:29-34. [Crossref] [PubMed]
- Schaake EE, Kappers I, Codrington HE, et al. Tumor response and toxicity of neoadjuvant erlotinib in patients with early-stage non-small-cell lung cancer. J Clin Oncol 2012;30:2731-8. [Crossref] [PubMed]
- Postmus PE, Kerr KM, Oudkerk M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28:iv1-iv21. [Crossref]
- Mok TS, Wu YL, Ahn MJ, et al. Osimertinib or Platinum-Pemetrexed in EGFR T790M-Positive Lung Cancer. N Engl J Med 2017;376:629-40. [Crossref] [PubMed]
- Raphael J, Vincent M, Boldt G, et al. Adjuvant Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors (TKIs) in Resected Non-Small Cell Lung Cancer (NSCLC): A Systematic Review and Meta-analysis. Am J Clin Oncol 2019;42:440-5. [Crossref] [PubMed]


