
Microcirculation and mean arterial pressure: friends or foes?—reply
In their editorial Drs. Hamzaoui and Shi discuss the current uncertainties about the pathogenesis of persisting microcirculatory alterations in septic patients who have achieved macrohemodynamic targets of resuscitation. The question remains whether these alterations occur because of suboptimal targets or because of true incoherence between macro- and microcirculation which cannot be addressed by hemodynamic interventions. We would like to thank Drs. Hamzaoui and Shi for their detailed commentary on our recent publication on the impact of increased mean arterial pressure (MAP) on skin microcirculatory oxygenation in septic patients (1).
Our study included septic patients all of whom had achieved the MAP target of 65 mmHg mandated by the current guidelines (2). In 75% of these resuscitated patients an increase of MAP by 20 mmHg resulted in the improvement of skin microcirculatory oxygenation. MAP of 85 mmHg and higher is frequently seen in practice as individualization of blood pressure targets based upon the clinical impression of organ perfusion is a common occurrence. Even in clinical trials with clearly defined blood pressure targets clinicians tend to target higher MAP targets than guidelines recommend (3).
The perfusion pressures achieved by clinician guided resuscitation result in a subgroup of noradrenaline receiving patients who cannot be defined as being in septic shock as they can maintain MAP of 65 mmHg without vasopressor support. We feel that our study adds to previous research in describing the microcirculatory effects of ongoing vasopressor infusion in this group of patients. Our data show that an increase in tissue oxygenation can be achieved in most patients with increments of MAP regardless of their baseline pressure. Given this discrepancy of clinical practice with the guidelines, the addition of objective evaluation of microcirculatory perfusion and oxygenation could serve as a superior guide to the restoration of adequate oxygen delivery than commonly used macrohemodynamic variables.
Several studies on the effects of perfusion pressure manipulation on microcirculation including ours have identified a subgroup of patients with microcirculatory abnormalities unresponsive to macrohemodynamic interventions (4,5). This subgroup which constituted 25% of all the patients included in our study can be described as having incoherent macro- and microcirculation. Although this group can be identified by monitoring the microcirculation relevant management strategies in these patients are as yet unclear.
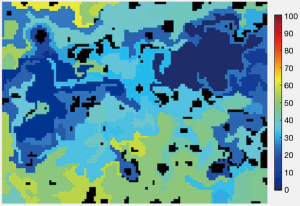
The expense and complexity of current methods of microcirculatory monitoring precludes their use for the selection of optimal macrohemodynamic targets in everyday practice. A major feature of microcirculation in septic patients is the increase of number unperfused and intermittently perfused capillaries leading to the coexistence of both hypoxic and well-oxygenated areas. The spatial resolution of the available methods except for intravital microscopy does not allow clinicians to assess this heterogeneity. Simple methods such as mottling and capillary refill time (CRT) have been adopted but either are qualitative or rely on assessment of a single site, such as the nailbed. If a good marker of microcirculatory perfusion is to be found it needs to obtain not only single site values for blood flow and oxygenation but also an index of their heterogeneity. The main advantage of hyperspectral imaging (HSI) is the ability to assess large areas of the skin. Heterogeneity of oxygenation can be identified and measurement focused on the worst perfused areas. We feel that HSI is a very promising technology because of ease of acquisition and automated analysis of images, as well as the ability to obtain perfusion, oxygenation and heterogeneity related values (Figure 1). We agree with Drs Hamzaoui and Shi that for the adoption of HSI for routine practice reference and target values of the obtained values need to be determined in larger studies.
Shock is defined as failure of circulation resulting in inadequate oxygen utilization by cells, and attempts at resuscitation should prioritize adequate oxygen delivery. While current guidelines provide guidance regarding macrohemodynamic management to achieve this goal, their application in practice shows that many patients benefit from an individualized approach. Before development of simple, objective methods of assessing tissue perfusion and oxygenation that take into account existing of heterogeneity individualized approach is difficult to achieve.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.03.101). The series “Hemodynamic Monitoring in Critically Ill Patients” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kazune S, Caica A, Luksevics E, et al. Impact of increased mean arterial pressure on skin microcirculatory oxygenation in vasopressor-requiring septic patients: an interventional study. Ann Intensive Care 2019;9:97. [Crossref] [PubMed]
- Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Medicine 2017;43:304-77. [Crossref] [PubMed]
- Asfar P, Meziani F, Hamel JF, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med 2014;370:1583-93. [Crossref] [PubMed]
- Thooft A, Favory R, Salgado DR, et al. Effects of changes in arterial pressure on organ perfusion during septic shock. Critical Care 2011;15:R222. [Crossref] [PubMed]
- Jhanji S, Stirling S, Patel N, et al. The effect of increasing doses of norepinephrine on tissue oxygenation and microvascular flow in patients with septic shock. Crit Care Med 2009;37:1961-6. [Crossref] [PubMed]


