
How will next generation sequencing (NGS) improve the diagnosis of congenital hemolytic anemia?
Congenital hemolytic anemias are a group of very heterogeneous and rare disorders caused by alterations in structure, transport functions or metabolism of red blood cells (RBC).
Because the pathophysiology of some rare forms is poorly understood, these disorders represent a group of diseases that still lack easy-to-apply tools for diagnosis, clinical management, and patient stratification.
Moreover, epidemiological data in the international literature are generally still incomplete, and the estimated prevalence of some defects varies widely among countries.
The advent of next generation sequencing (NGS) technologies make these new approaches useful tools to investigate the genetic basis of these disorders and to identify new nosological entities. Moreover, the reduction in cost of these techniques allowed the development of targeted NGS-based panels of known genes and their market development.
From this perspective, an article recently published by Xue and colleagues (1) in Annals of Translational Medicine highlights the importance of NGS in the diagnosis of congenital hemolytic anemia. The study focused on ten Chinese patients affected by hereditary spherocytosis (HS) and compared the results with clinical features and laboratory examinations.
HS is considered to be the most common disorder associated with congenital hemolytic anemia, and reported to have a homogeneous worldwide distribution with an estimate prevalence of about 1:2,000 in individuals from Europe and North America (2,3). In Chinese population however, HS prevalence seems to be lower and calculated to be about 1 in 100,000 people (1).
The diagnosis of HS is currently based on clinical and family history, evaluation of biochemical markers of hemolysis, RBC morphology, and functional testing, including the osmotic fragility test and eosin-5-maleimide (EMA) binding test; the combination of acidified lysis glycerol test (AGLT50) and EMA binding test has been reported to have the better sensitivity and specificity in diagnosing HS (4). Other more specific tests, such as the new generation ektacytometer laser-assisted optical rotational cell analyzer (LoRRca) Osmoscan and SDS-PAGE analysis, are available only in specialized laboratories and, when included in the diagnostic workflow, may provide additional information on the specific membrane defect (5-7).
Despite the availability of a battery of diagnostic tests, none of the above mentioned methods can detect all cases of HS; moreover, the concomitance of different defects (for example the co-presence of a RBC membrane defect with a β-thalassemia trait or a RBC enzymopathy) (8-10) or blood cell contamination due to red cell transfusion in the more severe patients, may interfere with the interpretation of the results, therefore representing a possible cause of misdiagnosis (9).
The molecular basis of HS are complex, because it is caused by alterations in genes encoding for one or more of the major RBC cytoskeleton and transmembrane proteins: ankyrin-1 (ANK1), band-3 (SLC4A1), α-spectrin (SPTA1), β-spectrin (SPTB) and protein 4.2 (EPB42) (11,12), resulting in a wide clinical heterogeneity, ranging from asymptomatic patients with compensated anemia, to severely anemic, transfusion-dependent cases.
Molecular testing in HS has not been considered for a long time except in particular cases, due to the consistent number and size of involved genes; however, this approach is now moving increasingly towards customized multi-gene panels (i.e., targeted-NGS) and whole-exome sequencing (13-15) for diagnosis of RBC defects, making easier, cheaper and faster to sequence and analyze a large number of genes (1).
The genes involved in HS in fact, are now usually included in the targeted panels specifically designed for the diagnosis of hereditary hemolytic anemias (14-20).
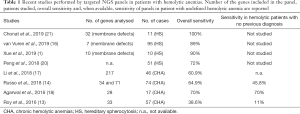
In the papers published in the last years, about 70–100% of patients with a previous diagnosis of HS were found to have a causative variants in the genes known to be associated with this disease (Table 1), suggesting that the use of targeted NGS has a high diagnostic efficiency in HS when used in combination with conventional diagnostic techniques; moreover, the molecular characterization of the defect allowed a definition of genotype-phenotype correlation (16,21), and in some cases the clarification of phenotypic variability sometime observed also inside the same family (19).
Xue and colleagues used the targeted capture and sequencing technique to confirm the diagnose in ten HS patients at molecular level. The authors detected pathogenetic variants in nine cases. Although the analyzed cohort is very limited to give information on the sensitivity of their approach, the detection rate obtained is comparable with previous reports; in particular, they found four mutations in SPTB, one in ANK1 and 1 in SLC4A1 gene, all at the heterozygous level and with dominant transmission in the affected families.
Given the wide spectrum of disorders associated with hemolytic anemias, NGS approaches offer a powerful diagnostic tool also for the cases who didn’t reach a definitive diagnosis with conventional methods, or for patients affected by ultra rare disorders. However, in these cases the diagnostic yield of targeted-NGS approach drastically drops down (Table 1), depending on the design of the platform, on the number of genes included in each panel (14,15), but possibly also on the kind of the patients studied; actually, a complete and detailed phenotyping and clinical classification of the patients is often mandatory to reach a definitive diagnosis in these cases.
Full table
The report of numerous variants of unknown significance (VUS) (22) to whom it is difficult to assign a certain pathogenetic significance may further reduce the sensitivity and specificity of results; in fact, not every mutation detected by DNA analysis should be classified as a disease-causing variant, even after in silico analysis by mutation prediction programs, until their pathogenic nature is confirmed with the functional analysis, such as protein quantification, Western Blot, RT-PCR analysis, or gene reporter assays. This may be particularly true for some variants that may have a mild effect on the phenotype accounting also for intrafamily variability as in the case reported by Xue and colleagues (1) (the same pathogenic variant identified in the affected mother and in the apparently healthy daughter).
The interpretation of NGS-derived data related to RBC membrane defects is also challenging because patients with inherited anemias can have multiple mutations with complex genotype-phenotype interactions (23), or may display low expression polymorphisms that modulate the phenotype [i.e., SPTA1LeLy (apics) or SPTA1Lepra (apics)] (21).
It would be desirable to have a common approach to standardize variability in current practice, including technical aspects, the number of genes analyzed, the diseases covered by the analysis, how to report variants and what specific functional tests are needed to validate a new pathogenetic mutation.
Although guidelines for variant reporting [e.g., American College of Medical Genetics and Genomics (ACMG)] (24) provide excellent advice on how to interpret the likely pathogenicity of genetic variants, no disease-specific guidance exists to assist in the clinical interpretation of NGS findings for individuals with rare inherited anemias (25). Given the rarity and the complexity of these disorders a shared scheme assessing specific external quality controls and interpretation of NGS could be of value.
As Xue and colleagues well underline in their study, one of the main causes of misdiagnosis in the past years could be also attributed to the lack of knowledge of these group of rare disorders by clinicians; the introduction of NGS techniques allowed in the past 2 years to double the number of diagnosed HS patients among Chinese population (1), further confirming the usefulness of this approach, and also its possible role in a more appropriate evaluation of rare disease prevalence among different populations.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xue J, He Q, Xie X, et al. Clinical utility of targeted gene enrichment and sequencing technique in the diagnosis of adult hereditary spherocytosis. Ann Transl Med 2019;7:527. [Crossref] [PubMed]
- Gallagher PG. Abnormalities of the erythrocyte membrane. Pediatr Clin North Am 2013;60:1349-62. [Crossref] [PubMed]
- Bianchi P, Mohandas N. Hereditary disorders of the red cell membrane and disorders of red cell metabolism in Postgraduate Haematology. Hoffbrand AV, Higgs DR, Keeling DM, et al. editors. 7th edition. John Wiley & Sons, Ltd., 2016.
- Bianchi P, Fermo E, Vercellati C, et al. Diagnostic power of laboratory tests for hereditary spherocytosis: a comparison study on 150 patients grouped according to the molecular and clinical characteristics. Haematologica 2012;97:516-23. [Crossref] [PubMed]
- Zaninoni A, Fermo E, Vercellati C, et al. Use of Laser Assisted Optical Rotational Cell Analyzer (LoRRca MaxSis) in the Diagnosis of RBC Membrane Disorders, Enzyme Defects, and Congenital Dyserythropoietic Anemias: A Monocentric Study on 202 Patients. Front Physiol 2018;9:451. [Crossref] [PubMed]
- Da Costa L, Suner L, Galimand J, et al. Society of Hematology and Pediatric Immunology (SHIP) group. French Society of Hematology (SFH). Diagnostic tool for red blood cell membrane disorders: Assessment of a new generation ektacytometer. Blood Cells Mol Dis 2016;56:9-22. [Crossref] [PubMed]
- Mariani M, Barcellini W, Vercellati C, et al. Clinical and hematologic features of 300 patients affected by hereditary spherocytosis grouped according to the type of the membrane protein defect. Haematologica 2008;93:1310-7. [Crossref] [PubMed]
- Zarza R, Moscardó M, Alvarez R, et al. Co-existence of hereditary spherocytosis and a new red cell pyruvate kinase variant: PK Mallorca. Haematologica 2000;85:227-32. [PubMed]
- Fermo E, Vercellati C, Marcello AP, et al. Hereditary Xerocytosis due to Mutations in PIEZO1 Gene Associated with Heterozygous Pyruvate Kinase Deficiency and Beta-Thalassemia Trait in Two Unrelated Families. Case Rep Hematol 2017;2017:2769570.
- Vercellati C, Marcello AP, Fermo E, et al. A case of hereditary spherocytosis misdiagnosed as pyruvate kinase deficient hemolytic anemia. Clin Lab 2013;59:421-24. [Crossref] [PubMed]
- Lux SE. Anatomy of the red cell membrane skeleton: Unanswered questions. Blood 2016;127:187-99. [Crossref] [PubMed]
- Perrotta S, Gallagher PG, Mohandas N. Hereditary spherocytosis. Lancet 2008;372:1411-26. [Crossref] [PubMed]
- Roy NB, Wilson EA, Henderson S, et al. A novel 33-Gene targeted esequencing panel provides accurate, clinical-grade diagnosis and improves atient management for rare inherited anaemias. Br J Haematol 2016;175:318-30. [Crossref] [PubMed]
- Russo R, Andolfo I, Manna F, et al. Multi-gene panel testing improves diagnosis and management of patients with hereditary anemias. Am J Hematol 2018;93:672-82. [Crossref] [PubMed]
- Wang R, Yang S, Xu M, et al. Exome sequencing confirms molecular diagnoses in 38 Chinese families with hereditary spherocytosis. Sci China Life Sci 2018;61:947-53. [Crossref] [PubMed]
- van Vuren A, van der Zwaag B, Huisjes R, et al. The Complexity of Genotype-Phenotype Correlations in Hereditary Spherocytosis: A Cohort of 95 Patients: Genotype-Phenotype Correlation in Hereditary Spherocytosis. Hemasphere 2019;3:e276. [Crossref] [PubMed]
- Li Y, Peng GX, Gao QY, et al. Using target next-generation sequencing assay in diagnosing of 46 patients with suspected congenital anemias. Zhonghua Xue Ye Xue Za Zhi 2018;39:414-9. [PubMed]
- Agarwal AM, Nussenzveig RH, Reading NS, et al. Clinical utility of next-generation sequencing in the diagnosis of hereditary haemolytic anaemias. Br J Haematol 2016;174:806-14. [Crossref] [PubMed]
- Fermo E, Vercellati C, Marcello AP, et al. Diagnosis of rare congenital hemolytic anemias enabled by next generation sequencing panel. EmaSphere 2018;2:148-9.
- Peng GX, Yang WR, Zhao X, et al. The characteristic of hereditary spherocytosis related gene mutation in 37 Chinese hereditary spherocytisis patients. Zhonghua Xue Ye Xue Za Zhi 2018;39:898-903. [PubMed]
- Chonat S, Risinger M, Sakthivel H, et al. The Spectrum of SPTA1-Associated Hereditary Spherocytosis. Front Physiol 2019;10:815. [Crossref] [PubMed]
- Trujillano D, Oprea GE, Schmitz Y, et al. A comprehensive global genotype-phenotype database for rare diseases. Mol Genet Genomic Med 2016;5:66-75. [Crossref] [PubMed]
- Gallagher PG, Maksimova Y, Lezon-Geyda K, et al. Aberrant splicing contributes to severe α-spectrin-linked congenital hemolytic anemia. J Clin Invest 2019;129:2878-87. [Crossref] [PubMed]
- Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015;17:405-24. [Crossref] [PubMed]
- Roy N, Proven M, Roberts I, et al. Towards an External Quality Assessment for Next Generation Sequencing in the Diagnosis of Rare Inherited Anaemias. Blood 2018;132:4936. [Crossref]


