
Diagnostic markers for community-acquired pneumonia
Introduction
Of infectious diseases worldwide, community-acquired pneumonia (CAP) is one of the most common and important causes of hospitalization and death (1-3). CAP is an infection of the lung parenchyma that is acquired in a community, not a hospital or a long-term care facility (4). CAP is defined as the presence of a lung infiltration shadow on chest radiography and any symptoms such as cough, sputum, fever, dyspnea, and chest pain (1). The diagnosis of CAP is sometimes difficult because viruses, fungi, and mycobacteria may cause the pneumonia, although the main causative pathogens are bacteria. In addition, there are many non-infectious diseases in the differential diagnosis of CAP, such as pulmonary edema, lung cancer, acute respiratory distress syndrome, and many interstitial lung diseases [cryptogenic organizing pneumonia (COP), eosinophilic pneumonia, drug-induced pneumonia, and vasculitis] (5).
We usually differentiate pneumonia from other non-infectious respiratory diseases by comprehensive evaluation including symptoms, laboratory examinations, and the properties of lung infiltrative shadows. However, some CAP patients, especially elderly patients, do not have cough, sputum, fever, and an elevated white blood cell count (6-8). Therefore, we usually perform blood tests for biomarkers to differentiate CAP from other non-infectious respiratory diseases. Currently, there are no biomarkers that could alone diagnose CAP, but the search for the ideal biomarker for pneumonia is ongoing, and multiple molecules are undergoing rigorous investigation (9). This article reviews some of the biomarkers for diagnosing CAP.
Inflammatory biomarkers in CAP
Biomarkers have been defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention” (10). An ideal diagnostic biomarker for CAP should be elevated only when bacterial infection has occurred and not in other infections, such as viral infections and fungal infections, to determine the need for antibiotic therapy. Furthermore, an ideal biomarker is expected to be simple to test, have the results available quickly, and not be expensive (11).
Overprescribing of antibiotics would lead to an increase in the probability of infection with antibiotic-resistant organisms (12,13). Therefore, it would be beneficial to have either rapid detection of the causative pathogens or the availability of biomarkers that would signify a bacterial infection that requires antibiotic therapy (14). Many biomarkers have been developed and used for diagnosing CAP so far (Table 1). However, some biomarkers cannot be examined in daily clinical practice. Therefore, we usually use some biomarkers such as the white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), procalcitonin (PCT), and so on. Of these biomarkers, less reliance has come to be placed on the WBC count and ESR because they have lower sensitivity and specificity compared with CRP and PCT (15). In addition, PCT is specific to bacterial infection, and there is more evidence to support its use for adjunctive diagnosis in CAP than for other biomarkers. The characteristics and usefulness of each biomarker in the diagnosis of CAP are reviewed below.
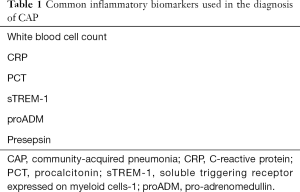
Full table
CRP
CRP is a 118-kDa pentameric protein synthesized in hepatic cells through induction by interleukin-6 (IL-6), IL-1β, and tumor necrosis factor-α (TNF-α) whenever infection or tissue inflammation occurs (16). CRP was first identified in pneumococcal pneumonia patients in 1930 (17). In healthy adults, the normal CRP concentration is usually less than 5 mg/L (18). The secretion of CRP starts within 4–6 hours, and its level doubles every 8 hours; it then reaches its maximum level within 36–50 hours. After the stimulation is removed, the CRP level falls relatively quickly, with a half-life of 19 hours (19).
Flanders et al. reported that a bedside CRP test was useful for predicting CAP in adults with acute cough (20). In 173 adult patients with acute cough, if the CRP cut-off level was ≥40 mg/L, the sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio for the diagnosis of pneumonia were 70%, 90%, 6.9, and 0.33, respectively. In addition, adding CRP to the clinical prediction rule of Heckerling (temperature >37.8 °C, pulse >100 beats per minute, rales, decreased breath sounds, and absence of asthma) could improve the area under the curve (AUC) (0.93) for diagnosing pneumonia compared to Heckerling’s score alone (AUC =0.88) (20).
Stolz et al. assessed the usefulness of CRP for predicting pneumonia in radiologically confirmed pneumonia patients (21). They showed that the specificity for predicting pneumonia was 91.2% when the CRP cut-off value was 100 mg/L (21).
As described above, some studies have reported that CRP was useful for diagnosing CAP, but CRP is not a specific biomarker of bacterial infection because it can be increased in malignant diseases and collagen vascular diseases (22,23). In addition, CRP is apparently decreased by corticosteroid therapy (24). Therefore, it was stated that “testing for C-reactive protein is neither sufficiently sensitive to rule out nor sufficiently specific to rule in both an infiltrate on chest radiograph and bacterial etiology of lower respiratory infection” in BMJ in 2005 (25).
PCT
PCT is a 13-kDa, 116 amino acid precursor peptide of calcitonin and was first reported in the medical literature in 1975 (26). It is usually produced by the C-cells in the thyroid (27). The PCT level in healthy adults is very low (<0.1 ng/mL) (28). In 1993, Assicot first reported that PCT increased in septic patients in a study of burn pediatric patients (29). When bacterial infection occurs, lipopolysaccharide (LPS), IL-1β, IL-6, and TNF-α can promote CALC-I gene expression, and then release of PCT is increased from parenchymal tissues, such as the liver, kidney, lung, intestine, and muscle (30,31). PCT is released within 2–3 hours after bacterial infection, with a peak at 6 hours and a half-life of approximately 22–35 hours (32-34). PCT levels are attenuated by the interferon-γ released in response to viral infection; therefore, PCT levels are theoretically not increased in viral infections. PCT release is not affected by systemic steroids, unlike CRP (35). The characteristics of PCT and CRP are listed in Table 2.

Full table
Regarding the diagnosis of CAP, Müller et al. reported that the clinical signs and symptoms routinely used to diagnose CAP are of limited value (36). They also showed that PCT was the most useful biomarker for differentiating radiologically confirmed CAP (n=373) from other non-infectious lung diseases (n=44) among PCT, highly-sensitive CRP, leukocytes, and temperature. The AUC of PCT (0.88) was significantly higher than of highly-sensitive CRP (0.76, P<0.001), leukocytes (0.69, P<0.001), and temperature (0.55, P<0.001) (36).
COP is one of the interstitial lung diseases that is defined histopathologically by intra-alveolar buds of granulation tissue consisting of intermixed myofibroblasts, fibroblasts, and connective tissue (37,38). COP is sometimes similar in symptoms and radiologic findings to CAP; therefore, it can be difficult to differentiate CAP from COP in the early stages, and we often treat COP patients with antimicrobial agents. There are some studies assessing the utility of PCT for differentiating CAP from COP (39-41). Kolditz et al. showed that both PCT and CRP were significantly higher in CAP than in OP (median PCT 2.6 vs. 0.14 ng/mL, P<0.001; median CRP 266 vs. 140 mg/L, P=0.014). They also showed that the AUC value of PCT (0.90, 95% CI: 0.73–0.98) for diagnosis of OP was significantly higher than that of CRP (0.76, 95% CI: 0.57–0.90). Another study by Takeda et al. also reported that PCT and CRP levels were significantly higher in CAP than in COP patients (40). However, their studies included small numbers of OP patients (Kolditz’s study, n=15) or COP patients (Takeda’s study, n=16). Therefore, we investigated the usefulness of PCT for differentiating CAP from COP in 56 COP and 914 hospitalized CAP patients (41). The diagnostic accuracy was significantly higher for PCT (AUC 0.79) than for WBC (AUC 0.69, P=0.048) and CRP (AUC 0.60, P<0.001). When the cutoff value of PCT was 0.25 ng/mL, the sensitivity and specificity for discriminating CAP from COP were 83.9% and 61.1%, respectively (41).
Regarding the correlation with causative pathogens of CAP and PCT, the PCT levels of classic bacterial pneumonia patients (n=27, median 1.41 µg/L) were reported to be higher than those of atypical pneumonia patients (n=9, median 0.05) (42). In this study, only one atypical patient (11.1%) had PCT levels ≥0.5 µg/L, whereas 21 of 27 bacterial pneumonia patients (77.8%) had PCT levels ≥0.5 µg/L (42). Thereafter, Krüger et al. compared the PCT levels among 5 groups (typical bacterial pathogens, atypical pathogens, virus, mixed infection, and unknown etiology) in 1,337 CAP patients (43). They reported that the PCT levels of typical bacterial pathogens were significantly higher than those of atypical pathogens (P<0.01) and viruses (P<0.01) (43). We also reported that the PCT levels of bacterial pneumonia patients (median 1.85 ng/mL) were significantly higher than those of atypical pneumonia patients, excluding Legionella pneumonia (median 0.41 ng/mL) (44). In addition, we showed that the CRP values were not significantly different between bacterial and atypical pneumonia patients (44). Self et al. showed that the median PCT values (ng/mL) of viral, atypical bacterial, typical bacterial, mycobacterial/fungal, and unknown etiology patients were 0.09, 0.20, 2.5, 0.19, and 0.14, respectively, and the PCT values of typical bacterial etiology patients were significantly higher than those of viral etiology patients (P<0.01) (45). However, of the 169 patients with typical bacterial pneumonia, 39 (23.1%) had PCT <0.25 ng/mL, and 21 (12.4%) had PCT <0.1 ng/mL (45). Naturally, we cannot detect the etiologic pathogens based on the PCT levels and should treat with antibiotic agents if we suspect clinically that the patients have bacterial pneumonia, because there are some bacterial pneumonia patients who have PCT levels less than 0.25 ng/mL. However, based on the previous reports, we may be able to guess the etiologic pathogen group, such as bacterial pathogens or atypical pathogens and viruses.
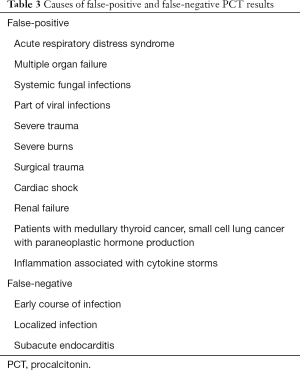
As we stated above, there are many reports regarding the usefulness of PCT for differentiating CAP from other respiratory diseases and bacterial from atypical or viral pneumonia. However, there are some limitations of PCT use because of false-positive and false-negative results; the false-positive and false-negative situations are listed in Table 3. Specifically, the PCT values could be less than 0.25 ng/mL because of measurement soon after symptom onset. Therefore, it is important to measure PCT serially within 6–24 hours, as stated by PCT-guided algorithms (46).
Full table
Soluble triggering receptor expressed on myeloid cells-1 (sTREM-1)
Triggering receptor expressed on myeloid cell 1 (TREM-1) is a glycoprotein member of the immunoglobulin family (47) that was first identified on both human and murine myeloid cells, especially neutrophils, mature monocytes, and macrophages (48). TREM-1 is highly increased in skin, biological fluids, and tissues when bacterial and fungal infections occur, but it is not increased in non-infectious inflammatory conditions (49). TREM-1 exists in both a membranous and a soluble form (sTREM-1), and sTREM-1 is released and can be measured in several body fluids (48).
Richeldi et al. reported that TREM-1 expression at the surface of alveolar neutrophils and macrophages was increased in bacterial pneumonia compared with in non-infectious interstitial lung diseases, although the expression of TREM-1 in peripheral blood neutrophils was similar in these patients (50). In addition, Gibot et al. showed that alveolar sTREM-1 concentrations were highly predictive of lung infection and performed better than any other clinical or biological findings in both CAP patients who required mechanical ventilation (n=38) and ventilator-associated pneumonia patients (n=46) (51). The area under the receiver-operating characteristic curve of sTREM-1 for differentiating the presence from the absence of pneumonia was 0.93 (95% CI: 0.92 to 0.95) (51). When the cutoff value of sTREM-1 was 5 pg/mL, the sensitivity and specificity were 98% and 90%, respectively (51). Huh et al. also reported that sTREM-1 concentrations in bronchoalveolar lavage (BAL) fluid of patients with bilateral lung infiltrates were significantly higher in bacterial or fungal pneumonia patients (n=29, 521.2±94.7 pg/mL) than in viral or atypical pneumonia patients (n=14, 92.9±20.0 pg/mL, P<0.05) and non-infectious disease patients (n=37, 92.8±10.7 pg/mL, P<0.05) (52). On multiple logistic regression analysis, they showed that the sTREM-1 level (cutoff value ≥184 pg/mL) in BAL fluid is an independent predictor of bacterial or fungal pneumonia, with an odds ratio of 59.742 (52).
However, all these studies indicated the usefulness of sTREM-1 in BAL fluid for diagnosing pneumonia, and there were few reports showing the usefulness of serum sTREM-1 for diagnosing pneumonia patients. Indeed, Müller et al. showed that the sTREM-1 levels in plasma and serum of CAP patients at admission were not significantly different according to pneumonia severity [mild vs. severe (median, interquartile range), 93.3 (44.1–165.2) vs. 79.1 (45.8–154.1), P=0.31] (53). Another study by Esposito et al. found that plasma sTREM-1 levels had a poor ability to differentiate bacterial from viral CAP in 433 hospitalized pediatric patients (AUC 0.50, 95% CI: 0.45–0.56) (54).
Basically, we do not routinely perform BAL examinations for CAP patients, especially in mild to moderate cases, because it is a relatively invasive procedure. Therefore, we think that sTREM-1 is not a useful biomarker for diagnosing pneumonia.
Pro-adrenomedullin (proADM)
ADM is produced by physiologic stress and has vasodilatory activity, bactericidal activity, and anti-inflammatory properties. Hirata reported that ADM levels increased according to disease severity in adult sepsis patients (55). However, ADM is rapidly cleared from the circulation due to its rapid binding to receptors and its half-life of 22 minutes (56). Therefore, midregional-proADM (MR-proADM), a precursor of ADM, is used in daily clinical practice because of its stability (57).
Krüger et al. showed that MR-proADM was the best predictor for 28-day and 180-day mortality among WBC, CRP, PCT, copeptin, CT-proET-1, MR-proANP, and MR-proADM in 728 CAP patients (58). In addition, Bello et al. showed that MR-proADM was the only biomarker able to predict short and long-term mortality among MR-proADM, WBC, CRP, and PCT in 228 hospitalized CAP patients (59). However, in their study, MR-proADM levels were almost similar between bacterial [median (interquartile range), 0.909 nmol/L (0.669–1.506 nmol/L)] and viral or atypical pneumonia patients [median (interquartile range), 0.875 nmol/L (0.606–1.155 nmol/L)] (59). Therefore, we think that MR-proADM is not useful for differentiating bacterial from viral pneumonia to determine whether we need to treat by antibiotics.
Presepsin
Presepsin is a 13-kDa protein and a fragment of monocyte LPS receptor CD14 that is released in the blood circulation during the process of bacterial phagocytosis. Yaegashi et al. reported that presepsin levels in sepsis patients were significantly higher than those of SIRS patients and healthy controls (60). Furthermore, Endo et al. reported that presepsin had similar diagnostic accuracy to PCT for differentiating bacterial and nonbacterial infectious diseases in a multicenter, prospective study in Japan (AUC of presepsin was 0.908, and that of PCT was 0.825) (61).
In 72 ICU patients admitted for acute respiratory failure, Klouche et al. reported that presepsin was useful for differentiating severe CAP from non-infectious respiratory failure (AUC 0.85) (62). When the cutoff value of presepsin was 588 pg/mL, the sensitivity and specificity for the diagnosis of pneumonia were 81% and 80%, respectively (62). In another study by Qi et al., presepsin levels in active pulmonary tuberculosis patients were reported to be slightly increased compared with those of healthy controls [median (interquartile range) pg/mL, 218.0 (146.0–368.0) vs. 128.0 (101.5–176.5)] (63). However, they also showed that presepsin was useful for discriminating bacterial CAP from active pulmonary tuberculosis (AUC 0.841) (63). Recently, Halıcı et al. reported that presepsin was useful for diagnosing pneumonia in chronic obstructive pulmonary disease patients with acute exacerbations (AUC 0.70) (64). However, the diagnostic accuracy of presepsin was not higher than of PCT (AUC 0.72) and CRP (AUC 0.75) (64).
There are only a few studies that have evaluated the usefulness of presepsin for diagnosing pneumonia. Therefore, whether presepsin is useful as a diagnostic biomarker in pneumonia patients in routine clinical practice is controversial, and further studies are needed.
Conclusions
Biomarkers are useful for differentiating CAP from other non-infectious respiratory diseases, but we should not rely only on biomarkers; they should be used adjunctively. The search for biomarkers that have higher sensitivity and specificity than the existing biomarkers for diagnosing CAP and could suggest the causative microorganisms continues, and it is hoped that they will be identified.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Zhi-De Hu, Bing Gu) for the series “Advances in laboratory tests for infectious diseases” published in Annals of Translational Medicine. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm.2020.02.182). The series “Advances in Laboratory Tests for Infectious Diseases” was commissioned by the editorial office without any funding or sponsorship. TI has received honoraria from MSD K. AI has no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mandell LA, Wunderrink RG, Anzueto A, et al. Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/ American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44:S27-72. [Crossref] [PubMed]
- Anevlavis S, Bouros D. Community-acquired bacterial pneumonia. Expert Opin Pharmacother 2010;11:361-74. [Crossref] [PubMed]
- The Committee for the Japanese Respiratory Society in the management of pneumonia in adults guidelines 2017. The JRS Guidelines for the management of pneumonia in adults 2017. Tokyo: The Japanese Respiratory Society, 2017.
- Watkins RR, Lemonovich TL. Diagnosis and management of community-acquired pneumonia in adults. Am Fam Physician 2011;83:1299-306. [PubMed]
- Musher DM, Thorner AR. Community-acquired pneumonia. N Engl J Med 2014;371:1619-28. [Crossref] [PubMed]
- Esposito AL. Community-acquired bacteremic pneumococcal pneumonia. Effect of age on manifestations and outcome. Arch Intern Med 1984;144:945-8. [Crossref] [PubMed]
- Metlay JP, Schulz R, Li YH, et al. Influence of age on symptoms at presentation in patients with community-acquired pneumonia. Arch Intern Med 1997;157:1453-9. [Crossref] [PubMed]
- Janssens JP, Krause KH. Pneumonia in the very old. Lancet Infect Dis 2004;4:112-24. [Crossref] [PubMed]
- Morley D, Torres A, Cillóniz C, et al. Predictors of treatment failure and clinical stability in patients with community acquired pneumonia. Ann Transl Med 2017;5:443. [Crossref] [PubMed]
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther 2001;69:89-95. [Crossref] [PubMed]
- Karakioulaki M, Stolz D. Biomarkers in Pneumonia-Beyond Procalcitonin. Int J Mol Sci 2019;20:2004. [Crossref] [PubMed]
- Malhotra-Kumar S, Lammens C, Coenen S, et al. Effect of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet 2007;369:482-90. [Crossref] [PubMed]
- Hillier S, Roberts Z, Dunstan F, et al. Prior antibiotics and risk of antibiotic-resistant community-acquired urinary tract infection: a case-control study. J Antimicrob Chemother 2007;60:92-9. [Crossref] [PubMed]
- Sungurlu S, Balk RA. The role of biomarkers in the diagnosis and management of pneumonia. Clin Chest Med 2018;39:691-701. [Crossref] [PubMed]
- Shaddock EJ. How and when to use common biomarkers in community-acquired pneumonia. Pneumonia 2016;8:17. [Crossref] [PubMed]
- Mortensen RF. C-reactive protein, inflammation, and innate immunity. Immunol Res 2001;24:163-76. [Crossref] [PubMed]
- Tillett WS, Francis T. Serological reactions in pneumonia with a non-protein somatic fraction of pneumococcus. J Exp Med 1930;52:561-71. [Crossref] [PubMed]
- Du Clos TW. C-reactive protein as a regulator of autoimmunity and inflammation. Arthritis Rheum 2003;48:1475-7. [Crossref] [PubMed]
- Póvoa P. C-reactive protein: a valuable marker of sepsis. Intensive Care Med 2002;28:235-43. [Crossref] [PubMed]
- Flanders SA, Stein J, Shochat G, et al. Performance of a bedside C-reactive protein test in the diagnosis of community-acquired pneumonia in adults with acute cough. Am J Med 2004;116:529-35. [Crossref] [PubMed]
- Stolz D, Christ-Crain M, Gencay MM, et al. Diagnostic value of signs, symptoms and laboratory values in lower respiratory tract infection. Swiss Med Wkly 2006;136:434-40. [PubMed]
- Nozoe T, Matsumata T, Kitamura M, et al. Significance of preoperative elevation of serum C-reactive protein as an indicator for prognosis in colorectal cancer. Am J Surg 1998;176:335-8. [Crossref] [PubMed]
- Otterness IG. The value of C-reactive protein measurement in rheumatoid arthritis. Semin Arthritis Rheum 1994;24:91-104. [Crossref] [PubMed]
- Youssef J, Novosad SA, Winthrop KL. Infection risk and safety of corticosteroid use. Rheum Dis Clin North Am. 2016;42:157-76. [Crossref] [PubMed]
- van der Meer V, Neven AK, van den Broek PJ, et al. Diagnostic value of C reactive protein in infections of the lower respiratory tract: systematic review. BMJ 2005;331:26. [Crossref] [PubMed]
- Moya F, Nieto A. R-Candela JL. Calcitonin biosynthesis: evidence for a precursor. Eur J Biochem 1975;55:407-13. [Crossref] [PubMed]
- Russwurm S, Oberhoffer M, Zipfel PF, et al. Procalcitonin--a novel biochemical marker for the mediator-directed therapy of sepsis. Mol Med Today 1999;5:286-7. [Crossref] [PubMed]
- Boussekey N, Leroy O, Georges H, et al. Diagnostic and prognostic values of admission procalcitonin levels in community-acquired pneumonia in an intensive care unit. Infection 2005;33:257-63. [Crossref] [PubMed]
- Assicot M, Gendrel D, Carsin H, et al. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993;341:515-8. [Crossref] [PubMed]
- Müller B, White JC, Nylén ES, et al. Ubiquitous expression of the calcitonin-i gene in multiple tissues in response to sepsis. J Clin Endocrinol Metab 2001;86:396-404. [PubMed]
- Linscheid P, Seboek D, Nylen ES, et al. In vitro and in vivo calcitonin I gene expression in parenchymal cells: a novel product of human adipose tissue. Endocrinology 2003;144:5578-84. [Crossref] [PubMed]
- Dandona P, Nix D, Wilson MF, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab 1994;79:1605-8. [PubMed]
- Brunkhorst FM, Heinz U, Forycki ZF. Kinetics of procalcitonin in iatrogenic sepsis. Intensive Care Med 1998;24:888-9. [Crossref] [PubMed]
- Reinhart K, Karzai W, Meisner M. Procalcitonin as a marker of the systemic inflammatory response to infection. Intensive Care Med 2000;26:1193-200. [Crossref] [PubMed]
- de Kruif MD, Lemaire LC, Giebelen IA, et al. The influence of corticosteroids on the release of novel biomarkers in human endotoxemia. Intensive Care Med 2008;34:518-22. [Crossref] [PubMed]
- Müller B, Harbarth S, Stolz D, et al. Diagnostic and prognostic accuracy of clinical and laboratory parameters in community-acquired pneumonia. BMC Infect Dis 2007;7:10. [Crossref] [PubMed]
- Cordier JF. Cryptogenic organising pneumonia. Eur Respir J 2006;28:422-46. [Crossref] [PubMed]
- Cottin V, Cordier JF. Cryptogenic organizing pneumonia. Semin Respir Crit Care Med 2012;33:462-75. [Crossref] [PubMed]
- Kolditz M, Halank M, Schulte-Hubbert B, et al. Procalcitonin improves the differentiation between infectious and cryptogenic/secondary organizing pneumonia. J Infect 2012;64:122-4. [Crossref] [PubMed]
- Takeda S, Nagata N, Miyazaki H, et al. Clinical utility of procalcitonin for differentiating between cryptogenic organizing pneumonia and community-acquired pneumonia. Int J Clin Med 2015;6:372-6. [Crossref]
- Ito A, Ishida T, Tachibana H, et al. Utility of procalcitonin for differentiating cryptogenic organising pneumonia from community-acquired pneumonia. Clin Chem Lab Med 2019;57:1632-7. [Crossref] [PubMed]
- Hedlund J, Hansson LO. Procalcitonin and C-reactive protein levels in community-acquired pneumonia: correlation with etiology and prognosis. Infection 2000;28:68-73. [Crossref] [PubMed]
- Krüger S, Ewig S, Papassotiriou J, et al. CAPNETZ Study Group. Inflammatory parameters predict etiologic patterns but do not allow for individual prediction of etiology in patients with CAP: results from the German competence network CAPNETZ. Respir Res 2009;10:65. [Crossref] [PubMed]
- Ito A, Ishida T, Tachibana H, et al. Serial procalcitonin levels for predicting prognosis in community-acquired pneumonia. Respirology 2016;21:1459-64. [Crossref] [PubMed]
- Self WH, Balk RA, Grijalva CG, et al. Procalcitonin as a marker of etiology in adults hospitalized with community-acquired pneumonia. Clin Infect Dis 2017;65:183-90. [Crossref] [PubMed]
- Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med 2011;9:107. [Crossref] [PubMed]
- Salluh JIF, Souza-Dantas VC, Póvoa P. The current status of biomarkers for the diagnosis of nosocomial pneumonias. Curr Opin Crit Care 2017;23:391-7. [Crossref] [PubMed]
- Lemarié J, Gibot S. Soluble triggering receptor expressed on myeloid cells-1: diagnosis or prognosis? Crit Care Clin 2020;36:41-54. [Crossref] [PubMed]
- Bouchon A, Facchetti F, Weigand MA, et al. TREM-1 amplifies inflammation and is a crucial mediator of septic shock. Nature 2001;410:1103-7. [Crossref] [PubMed]
- Richeldi L, Mariani M, Losi M, et al. Triggering receptor expressed on myeloid cells: role in the diagnosis of lung infections. Eur Respir J 2004;24:247-50. [Crossref] [PubMed]
- Gibot S, Cravoisy A, Levy B, et al. Soluble triggering receptor expressed on myeloid cells and the diagnosis of pneumonia. N Engl J Med 2004;350:451-8. [Crossref] [PubMed]
- Huh JW, Lim CM, Koh Y, et al. Diagnostic utility of the soluble triggering receptor expressed on myeloid cells-1 in bronchoalveolar lavage fluid from patients with bilateral lung infiltrates. Crit Care 2008;12:R6. [Crossref] [PubMed]
- Müller B, Gencay MM, Gibot S, et al. Circulating levels of soluble triggering receptor expressed on myeloid cells (sTREM)-1 in community-acquired pneumonia. Crit Care Med 2007;35:990-1. [Crossref] [PubMed]
- Esposito S, Di Gangi M, Cardinale F, et al. Ita-CAP Study Group. Sensitivity and specificity of soluble triggering receptor expressed on myeloid cells-1, midregional proatrial natriuretic peptide and midregional proadrenomedullin for distinguishing etiology and to assess severity in community-acquired pneumonia. PLoS One 2016;11:e0163262. [Crossref] [PubMed]
- Hirata Y, Mitaka C, Sato K, et al. Increased circulating adrenomedullin, a novel vasodilatory peptide, in sepsis. J Clin Endocrinol Metab 1996;81:1449-53. [PubMed]
- Morgenthaler NG, Struck J, Alonso C, et al. Measurement of midregional proadrenomedullin in plasma with an immunoluminometric assay. Clin Chem 2005;51:1823-9. [Crossref] [PubMed]
- Struck J, Tao C, Morgenthaler NG, et al. Identification of an adrenomedullin precursor fragment in plasma of sepsis patients. Peptides 2004;25:1369-72. [Crossref] [PubMed]
- Krüger S, Ewig S, Giersdorf S, et al. German Competence Network for the Study of Community Acquired Pneumonia (CAPNETZ) Study Group. Cardiovascular and inflammatory biomarkers to predict short- and long-term survival in community-acquired pneumonia: Results from the German Competence Network, CAPNETZ. Am J Respir Crit Care Med 2010;182:1426-34. [Crossref] [PubMed]
- Bello S, Lasierra AB, Mincholé E, et al. Prognostic power of proadrenomedullin in community-acquired pneumonia is independent of aetiology. Eur Respir J 2012;39:1144-55. [Crossref] [PubMed]
- Yaegashi Y, Shirakawa K, Sato N, et al. Evaluation of a newly identified soluble CD14 subtype as a marker for sepsis. Evaluation of a newly identified soluble CD14 subtype as a marker for sepsis. J Infect Chemother 2005;11:234-8. [Crossref] [PubMed]
- Endo S, Suzuki Y, Takahashi G, et al. Usefulness of presepsin in the diagnosis of sepsis in a multicenter prospective study. J Infect Chemother 2012;18:891-7. [Crossref] [PubMed]
- Klouche K, Cristol JP, Devin J, et al. Diagnostic and prognostic value of soluble CD14 subtype (Presepsin) for sepsis and community-acquired pneumonia in ICU patients. Ann Intensive Care 2016;6:59. [Crossref] [PubMed]
- Qi ZJ, Yu H, Zhang J, et al. Presepsin as a novel diagnostic biomarker for differentiating active pulmonary tuberculosis from bacterial community acquired pneumonia. Clin Chim Acta 2018;478:152-6. [Crossref] [PubMed]
- Halıcı A, Hür İ, Abatay K, et al. The role of presepsin in the diagnosis of chronic obstructive pulmonary disease acute exacerbation with pneumonia. Biomark Med 2020;14:31-41. [Crossref] [PubMed]


