
Rare paradoxical adverse event in Crohn’s disease: a case report
Introduction
Biological agent therapy has been reported to cause several paradoxical adverse events (PAEs) during treatment of immune-mediated inflammatory disorders. PAEs are defined as pathological conditions during biological agent therapy that is usually effective in treatment (1). Herein, we report a rare case of PAEs occurring in a patient with Crohn’s disease.
Case presentation
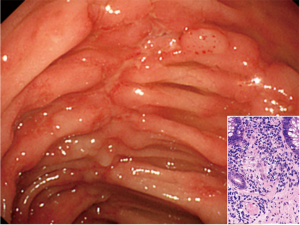
An 18-year-old male adolescent was referred to our hospital for diarrhea, fever (temperature >38 °C), stomatitis, and perianal abscess for 4 months. He had no allergies, no significant medical history, and was not on any medication. Colonoscopy revealed multiple erosions in the terminal ileum and extensive longitudinal ulcers in the colon (Figure 1). Therefore, several biopsies were obtained that showed poorly formed non-caseating granulomas without a well-demarcated septum (Figure 1 insert). He was diagnosed with ileocolitis-type Crohn’s disease. A combination of an elemental diet and oral prednisolone (starting dose of 0.6 mg/kg/day, subsequently tapered) resulted in remission, but the disease relapsed because of poor patient compliance. Furthermore, he received therapy involving an anti-tumor necrosis factor-α (TNF-α) blocker (infliximab, 5 mg/kg during weeks 0, 2, and 6; subsequently, once every 8 weeks), which resulted in remission for 2 years. However, after the remission, he was lost to follow-up.
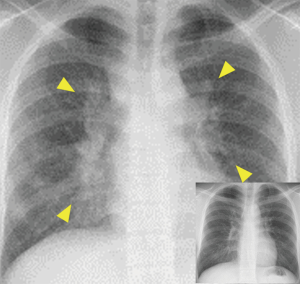
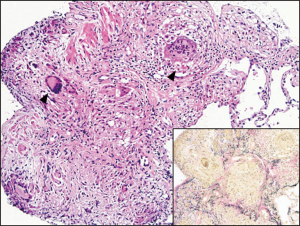
Eleven months later, he presented with fever, stomatitis, and cough with respiratory distress that had lasted for 3 months. His peripheral blood white blood cell count and C-reactive protein level were slightly elevated at 10,100/µL (neutrophils: 72.5%) and 2.29 mg/mL (reference: <0.20), respectively. Several tests inspecting infection as tuberculosis and sarcoidosis were negative. Additionally, serum TNF-α level was abnormally elevated at 117.4 pg/mL (reference: <2.8). The serum angiotensin-converting enzyme (ACE), soluble interleukin-2 receptor (sIL-2R), and lysozyme levels were elevated at 70.2 U/L (reference range, 7.0–25.0 U/L), 10,048 U/mL (122–496 U/L), and 35.8 µg/mL (5.0–10.0 µg/mL), respectively. Furthermore, a chest radiograph revealed bilateral hilar lymphadenopathy (Figure 2, yellow triangle), and bronchoalveolar lavage showed a high lymphocyte level: 40.8% (reference <15%) and CD4/8 value: 3.9 (reference <3.5). Transbronchial lung biopsy identified multiple non-caseating granulomas fused to each other with connective tissue septa, leading to a diagnosis of sarcoidosis (Figure 3, black triangles, giant cells; insert: Elastica van Gieson staining).
Cessation of TNF-α blocker administration was sufficient to induce remission.
Discussion
Cases of sarcoidosis and granulomatosis-like diseases that occur during or after treatment with immune checkpoint inhibitors, highly active antiretroviral therapy, interferons, and TNF-α blocker have been reported (2), although cases of Crohn’s disease are still scarce. The mechanism of the reaction remains unclear, however, in our case, the paradoxical increase in TNF-α activity may have triggered the disease because TMF-α plays an important role in the formation and maintenance of sarcoid granuloma (3). The prognosis of sarcoidosis as a PAE seems favorable, and in most cases, cessation of TNF-α blocker administration is sufficient to induce remission (Figure 2 insert, 8 months later). In cases treated with biological agents, including TNF-α blocker, a careful follow-up and differential diagnoses of PAEs are necessary even after treatment cessation. For the diagnosis of sarcoidosis, there are no specific or sensitive symptoms or physical findings. However, the specificity and sensitivity of elevated serum ACE and sIL-2R level, respectively, were reported to be high (4,5), which are useful for differential diagnosis. Furthermore, bilateral hilar lymphadenopathy on chest radiography is also a characteristic finding. Thereafter, non-caseating granulomas on histology should be proved, and if the disease is in the lungs, elevated lymphocyte on bronchoalveolar lavage is also supplementary (6). We should consider lung infections or metastatic Crohn’s disease (7), which have more severe pathology when compared with our case. Only case report and case series are present in literature, which can be considered a limitation, however, our case suggests that laboratory, radiography, and histological findings are useful for the differentiation and management of sarcoidosis as PAE.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Toussirot É, Aubin F. Paradoxical reactions under TNF-alpha blocking agents and other biological agents given for chronic immune-mediated diseases: an analytical and comprehensive overview. RMD Open 2016;2:e000239. [Crossref] [PubMed]
- Chopra A, Nautiyal A, Kalkanis A, Judson MA. Drug-Induced Sarcoidosis-Like Reactions. Chest 2018;154:664-77. [Crossref] [PubMed]
- Marzouk K, Saleh S, Kannass M, et al. Interferon-induced granulomatous lung disease. Curr Opin Pulm Med 2004;10:435-40. [Crossref] [PubMed]
- Ungprasert P, Carmona EM, Crowson CS, et al. Diagnostic Utility of Angiotensin-Converting Enzyme in Sarcoidosis: A Population-Based Study. Lung 2016;194:91-5. [Crossref] [PubMed]
- Thi Hong Nguyen C, Kambe N, et al. Serum soluble interleukin-2 receptor level is more sensitive than angiotensin-converting enzyme or lysozyme for diagnosis of sarcoidosis and may be a marker of multiple organ involvement. J Dermatol 2017;44:789-97. [Crossref] [PubMed]
- Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 1999;160:736-55. [PubMed]
- Gill KR, Mahadevan U. Infliximab for the treatment of metastatic hepatic and pulmonary Crohn's disease. Inflamm Bowel Dis 2005;11:210-2. [Crossref] [PubMed]


