Analysis of young ischemic stroke patients in northeast China
Introduction
Young stroke patients are often misdiagnosed at initial presentation (1); however, stroke in young adults results in devastating implications for the quality of life and ability to work, and creates a huge socio-economic burden (2-4). A previous study found that the highest incidence of stroke in China was in the north of the country (5). Knowledge of the etiology, stroke subgroups, and risk factors of stroke in young individuals could be beneficial for planning preventive strategies and improving quality of life. Previous studies have reported that the etiology and risk factors for young stroke patients vary by age, race, and region (6-8). However, these studies were small or methodologically heterogeneous (9) and limited prior research has specifically addressed stroke etiology in young patients in developing countries (10).
Due to the high expense, invasiveness, and radiation hazard of traditional vascular examination methods, few studies have focused on imaging features and cerebrovascular stenosis in young ischemic stroke (IS) patients (7,11-14). In recent years, the development of non-invasive examination methods, such as magnetic resonance angiography (MRA), transcranial Doppler (TCD), and carotid ultrasound, has helped better assessment of intracranial and extracranial vascular status. The present study analyzed the risk factors, etiologies, and the distribution of vascular stenosis in young IS patients. The prevalence of risk factors and differences in etiology between first-ever stroke and recurrent-stroke patients were also investigated.
Methods
We retrospectively analyzed the demographics and clinical data of young IS patients obtained from the stroke database of The First Hospital of Jilin University between January 1, 2013, and December 31, 2017. Patients meeting the following inclusion criteria were included in the present study: (I) aged 15–49 at stroke onset; (II) discharge diagnosis of IS; (III) underwent at least magnetic resonance imaging (MRI) or computed tomography (CT). Additional imaging studies, namely carotid artery ultrasonography, TCD or MRA, computed tomography angiography (CTA), and digital subtraction angiography (DSA), were also reviewed if conducted on those patients.
Patients were excluded from the present study if they had been diagnosed with transient ischemic attack (TIA), cerebral venous thrombosis, stroke attributable to direct head trauma or strangulation, ischemic lesion attributable to immediate complications originating from subarachnoidal hemorrhage, and any iatrogenic stroke as a consequence of angiographic imaging or major surgery (7). IS was defined as a focal neurological deficit of sudden onset that persisted beyond 24 hours or with evidence of acute brain ischemia on neuroimaging when symptoms lasted less than 24 hours. TIA was defined similarly but with symptoms lasting less than 24 hours and without corresponding imaging evidence of ischemic lesion (7). The study protocol was approved by the ethics committee of The First Hospital of Jilin University. The ethics committee provided a waiver for informed consent as patients were not contacted directly and the results of the study did not impact their care.
All patients underwent routine blood testing, chest radiography, and an electrocardiogram (ECG) at admission. Demographic data, medical history, and family history of stroke were extracted from the patient records. Risk factor variables included hypertension, dyslipidemia, diabetes, coronary artery disease, hyperhomocysteinemia, current cigarette smoking, and alcohol consumption (regular alcohol consumption in the 3 months preceding the stroke). Hypertension was defined as a medical history of hypertension or the use of antihypertensive drugs 2 weeks prior to enrolment in the study, a systolic blood pressure of ≥140 mmHg and/or a diastolic blood pressure of ≥90 mmHg (15). Diabetes mellitus was defined as a medical history of diabetes or the use of oral hypoglycemic medication or patients with a fasting glucose ≥7.0 mmol/L (126 mg/dL) or a two-hour postprandial serum glucose ≥11.1 mmol/L (200 mg/dL) (13). Dyslipidemia was defined as a history of hyperlipidemia, taking oral antidyslipidemic drugs, or the fulfillment of one of the following criteria: a total cholesterol level (TC) of ≥5.18 mmol/L, a low-density lipoprotein cholesterol (LDL-C) level of ≥3.37 mmol/L, a high-density lipoprotein cholesterol (HDL-C) level of <1.04 mmol/L, and triglyceride (TG) level of ≥1.70 mmol/L (16,17). Hyperhomocysteinemia was defined as total homocysteine level ≥10 µmol/L, as recommended by the American Heart Association and the American Stroke Association Council on stroke (18). Individuals were considered overweight or obese if they had a body mass index (BMI) of ≥26 kg/m2 (15). Stroke subtypes were classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria (19) as large-artery atherosclerosis (LAA), small-vessel disease (SVD), cardioembolism (CE), other determined etiology (ODE) and undetermined etiology (UDE). The study patients were first divided into different groups according to sex (male versus female) and age (15–44 versus 45–49 years). They were then grouped into first-ever stroke and recurrent stroke groups. If patients or their family members self-reported a previous history of stroke, which was supplemented by previous hospital records and brain imaging, they were categorized into the recurrent stroke group.
The cranial CT scans of all patients were examined to exclude cerebral hemorrhage. Infarct sites were determined using cranial MRI (T1-, T2-, and diffusion-weighted sequences). Carotid doppler ultrasonography, TCD, MRA, CTA, or DSA were used to define stenosis as narrowing of intra- or extracranial arteries by ≥50% (20).
All analyses were performed using SPSS 23.0 (IBM Corp., Armonk, NY, USA). Pearson’s Chi-squared test and Fisher’s exact test were used to compare categorical variables across groups and Student’s t-test was used to compare means. Numerical values with non-normal distribution are shown as the median (interquartile range, IQR) and a non-parametric test was used to compare differences between the two groups. Two-sided probability values (P) <0.05 were considered statistically significant.
Results
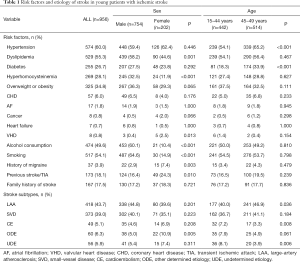
In total, 956 young IS patients from our database were enrolled in this study. There were 754 males (78.9% of total; male: female ratio 3.73:1). They were aged 15–49 years, with a median age (IQR) of 45 [40–47] years.
Overall, males had a significantly higher frequency of dyslipidemia and hyperhomocysteinemia than females (P=0.001 and P<0.001, respectively) (Table 1). Moreover, males were significantly more likely to be smokers and consume alcohol than females (P<0.001 for both). Conversely, females had a significantly higher frequency of valvular heart disease (P=0.013), history of migraine (P=0.003) and previous stroke or TIA (P=0.010) compared to males.
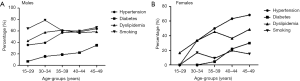
Full table
Patients were also divided into two groups according to their age; one group consisted of 442 patients aged 15–44 years (46.2%) and the second group consisted of 514 patients aged 45–49 years (53.8%) (Table 1). Comparisons of the two groups showed that hypertension and diabetes mellitus were more common in the 45–49 years age-group (P<0.001 for both) (Table 1, Figure 1).
Using the TOAST classification to identify stroke subtypes, the most common etiology of IS was LAA (43.7%), followed by SVD (39.0%). CE was uncommon (5.1%) (Table 1). Significant differences in etiology were observed between males and females (P=0.010) and the two age groups (P<0.001). The ODE stroke subtype was significantly higher in females than in males (P=0.005) whereas the UDE and CE stroke subtypes were significantly higher among the 15–44-year-old patients (P=0.006 and P=0.008, respectively) and the LAA subtype was significantly higher in the 45–49 years age-group (P=0.036).
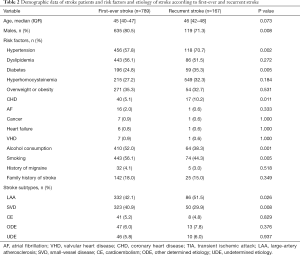
The proportion of males in the first-ever stroke group was significantly higher than that of the recurrent stroke group (P=0.008). The age of recurrent stroke patients was slightly higher than that of first-ever stroke patients (46 versus 45, P=0.073). Hypertension, diabetes, and coronary heart disease (CHD) were significantly higher in recurrent stroke patients than those in first-ever stroke patients (P=0.002, P=0.005, and P=0.011, respectively). However, recurrent stroke patients were significantly less likely to smoke (P=0.005) and consume alcohol (P=0.001) than first-ever stroke patients (Table 2). Recurrent stroke was more frequently caused by LAA (P=0.026) and less often by SVD (P=0.008) compared to etiologies observed in first-ever stroke patients.
Full table
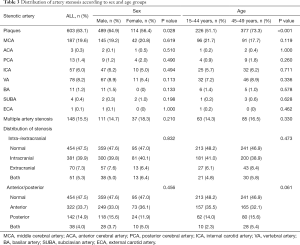
Carotid doppler ultrasound was performed on all patients, TCD examination in 778 (81.4%) patients, MRA examination in 406 (42.5%) patients, CTA examination in 61 (6.4%) patients, and DSA examination in 92 (9.6%) patients. Carotid doppler ultrasound reports showed that 603 patients (63.1%) had plaque, with significantly higher frequency in males (P=0.028) and 45–49-year-old patients (P<0.001).
There was no significant difference in distribution of stenosis between the different groups according to sex and age groups. Multiple artery stenosis was observed in 148 patients (15.5%) and middle cerebral artery (MCA) was the artery that was the most affected by stenosis in young patients with IS (19.6%), followed by the vertebral artery (8.2%), and internal carotid artery (ICA) (6.0%) (Table 3).
Full table
Discussion
This study showed that males were the most affected in young stroke patients of northeast China and that the proportion of conventional stroke risk factors in young patients was very high and were not well managed. The proportion of intracranial vascular stenosis observed was higher than that of previous studies. The most common etiology was LAA, followed by SVD; CE was less common.
The median age of patients in our study was 45 years, which was higher than that reported in young stroke studies in other countries (6,7,21); however, the high proportion of male patients in our study is consistent with what has previously been reported (7,22-26).
The current study provides a meaningful overview of the risk factors for young IS. Patients in our study had a high rate of conventional stroke risk factors, which is consistent with other studies (27,28). The most common risk factor in our study was hypertension. Hypertension in China is associated with high salt intake, obesity, smoking, alcohol consumption, and low education (29,30). In our study, dyslipidemia, hyperhomocysteinemia, smoking, and alcohol consumption were highly common in male patients. In fact, smoking and alcohol consumption surpassed hypertension as the most common risk factors for IS in young male patients, which has also been reported elsewhere (7,13,31-33). Estrogen has a protective effect on ischemia, which may explain the lower prevalence of IS in females (34). Females, however, showed a higher incidence of migraines and valvular heart disease, which was similar to previous studies (13,32,35).
A few studies have been done in young patients with recurrent stroke. In our study, recurrent stroke was associated with hypertension, diabetes, and CHD, which is similar to other studies (32,36). We also found that behavioral risk factors, that is smoking and alcohol consumption, were significantly lower in the recurrent stroke group; however, the proportions were still high (44.3% and 38.3%, respectively). These results suggest that secondary prevention has not been sufficiently conducted in patients who already experienced stroke once, as has been previously shown (32,36).
In terms of stroke etiology, the proportion of patients with LAA was higher than that with SVD, which is similar to findings of studies conducted in Korea (37) and the USA (26). In contrast, studies in Taiwan (24) and Finland (7) have shown that SVD was more common than LAA. However, the proportion of LAA and SVD in these studies was low, which was different from what we observed in our study. Furthermore, some studies in Europe found that most young strokes were caused by cardiac embolisms (7,38,39), which was uncommon in our study. These differences in stroke etiology might potentially be caused by a different distribution of risk factors or ethnic groups. In fact, in a recent study of ischemic stroke in young people of northern China showing results similar to ours, the authors indicated that the stroke etiology could be related to the higher prevalence of atherosclerosis in northern China (40).
Recent studies have shown that intracranial stenosis is common in young stroke, in particular at the MCA, which is highly vulnerable to stenosis (13). This is in line with our observations, where MCA stenosis was the most common subtype of symptomatic intracranial arterial stenosis in young adults. In previous studies, the incidence of intracranial stenosis or occlusion in young Asian stroke patients was 22–26%, and in a European study, it was 11.8%, which was lower than our study (12,41-43). Furthermore, anterior circulation stenosis of cerebral vessels was observed in a significant proportion of patients in our study, which is consistent with what was previously known (13).
For young stroke patients of northeast China, there are fewer studies on a larger sample and fewer studies on vascular conditions due to some technical limitations. Our study solves these problems. The vascular examination and imaging examination of the patients in our study were comprehensive, and the number of patients was relatively large. In addition, grouping patients into first-ever and recurrent stroke groups at admission also guided secondary prevention of stroke through a better understanding of its behavioral risk factors.
Our study had certain limitations. There were some missing data as this was a retrospective study and we, therefore, had to rely on patient reports previously stored in the computer database. Moreover, although our study sample size was relatively large, our patients originated from several provinces and cities of northeast China; therefore, a multi-center study is still needed to analyze regional characteristics.
Conclusions
LAA is the most common etiology in Chinese young stroke patients, especially in those with recurrent stroke. Our data highlight the need of screening of LAA and prevention and management of conventional stroke risk factors in young people of China. Secondary prevention and post-stroke education need to be more widely available.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (grant number 81971620).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the ethics committee of The First Hospital of Jilin University and all methods were performed in accordance with the relevant guidelines and regulations. The ethics committee provided a waiver for informed consent as patients were not contacted directly and the results of the study did not impact their care.
References
- Kuruvilla A, Bhattacharya P, Rajamani K, et al. Factors associated with misdiagnosis of acute stroke in young adults. J Stroke Cerebrovasc Dis 2011;20:523-7. [Crossref] [PubMed]
- Naess H, Nyland H. Poststroke fatigue and depression are related to mortality in young adults: a cohort study. BMJ open 2013;3. [Crossref] [PubMed]
- Naess H, Waje-Andreassen U, Thomassen L, et al. Health-related quality of life among young adults with ischemic stroke on long-term follow-up. Stroke 2006;37:1232-6. [Crossref] [PubMed]
- Giang KW, Bjorck L, Nielsen S, et al. Twenty-year trends in long-term mortality risk in 17,149 survivors of ischemic stroke less than 55 years of age. Stroke 2013;44:3338-43. [Crossref] [PubMed]
- Wang W, Jiang B, Sun H, et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017;135:759-71. [Crossref] [PubMed]
- Putaala J, Yesilot N, Waje-Andreassen U, et al. Demographic and geographic vascular risk factor differences in European young adults with ischemic stroke: the 15 cities young stroke study. Stroke 2012;43:2624-30. [Crossref] [PubMed]
- Putaala J, Metso AJ, Metso TM, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki young stroke registry. Stroke 2009;40:1195-203. [Crossref] [PubMed]
- Pezzini A, Grassi M, Lodigiani C, et al. Predictors of long-term recurrent vascular events after ischemic stroke at young age: the Italian Project on Stroke in Young Adults. Circulation 2014;129:1668-76. [Crossref] [PubMed]
- von Sarnowski B, Putaala J, Grittner U, et al. Lifestyle risk factors for ischemic stroke and transient ischemic attack in young adults in the Stroke in Young Fabry Patients study. Stroke 2013;44:119-25. [Crossref] [PubMed]
- Singhal AB, Biller J, Elkind MS, et al. Recognition and management of stroke in young adults and adolescents. Neurology 2013;81:1089-97. [Crossref] [PubMed]
- Siddiq F, Chaudhry SA, Vazquez G, et al. Intracranial stenosis in young patients: unique characteristics and risk factors. Neuroepidemiology 2012;38:148-53. [Crossref] [PubMed]
- von Sarnowski B, Schminke U, Tatlisumak T, et al. Prevalence of stenoses and occlusions of brain-supplying arteries in young stroke patients. Neurology 2013;80:1287-94. [Crossref] [PubMed]
- Ojha R, Huang D, An H, et al. Distribution of ischemic infarction and stenosis of intra- and extracranial arteries in young Chinese patients with ischemic stroke. BMC Cardiovasc Disord 2015;15:158. [Crossref] [PubMed]
- Fromm A, Waje-Andreassen U, Thomassen L, et al. Comparison between Ischemic Stroke Patients <50 Years and ≥50 Years Admitted to a Single Centre: The Bergen Stroke Study. Stroke Res Treat 2011;2011:183256. [Crossref] [PubMed]
- Chen HX, Wang LJ, Yang Y, et al. The prevalence of intracranial stenosis in patients at low and moderate risk of stroke. Ther Adv Neurol Disord 2019;12:1756286419869532. [Crossref] [PubMed]
- Zhang FL, Xing YQ, Wu YH, et al. The prevalence, awareness, treatment, and control of dyslipidemia in northeast China: a population-based cross-sectional survey. Lipids Health Dis 2017;16:61. [Crossref] [PubMed]
- Wang Y, Cui L, Ji X, et al. The China National Stroke Registry for patients with acute cerebrovascular events: design, rationale, and baseline patient characteristics. Int J Stroke 2011;6:355-61. [Crossref] [PubMed]
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke 2006;37:577-617. [Crossref] [PubMed]
- Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35-41. [Crossref] [PubMed]
- Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Circulation 2011;124:e54-130. [PubMed]
- Putaala J, Curtze S, Hiltunen S, et al. Causes of death and predictors of 5-year mortality in young adults after first-ever ischemic stroke: the Helsinki Young Stroke Registry. Stroke 2009;40:2698-703. [Crossref] [PubMed]
- Varona JF, Guerra JM, Bermejo F, et al. Causes of ischemic stroke in young adults, and evolution of the etiological diagnosis over the long term. Eur Neurol 2007;57:212-8. [Crossref] [PubMed]
- Leys D, Bandu L, Henon H, et al. Clinical outcome in 287 consecutive young adults (15 to 45 years) with ischemic stroke. Neurology 2002;59:26-33. [Crossref] [PubMed]
- Lee TH, Hsu WC, Chen CJ, et al. Etiologic study of young ischemic stroke in Taiwan. Stroke 2002;33:1950-5. [Crossref] [PubMed]
- Naess H, Nyland HI, Thomassen L, et al. Incidence and short-term outcome of cerebral infarction in young adults in western Norway. Stroke 2002;33:2105-8. [Crossref] [PubMed]
- Adams HP Jr, Kappelle LJ, Biller J, et al. Ischemic stroke in young adults. Experience in 329 patients enrolled in the Iowa Registry of stroke in young adults. Arch Neurol. 1995;52:491-5. [Crossref] [PubMed]
- Rolfs A, Fazekas F, Grittner U, et al. Acute cerebrovascular disease in the young: the Stroke in Young Fabry Patients study. Stroke 2013;44:340-9. [Crossref] [PubMed]
- Ji R, Schwamm LH, Pervez MA, et al. Ischemic stroke and transient ischemic attack in young adults: risk factors, diagnostic yield, neuroimaging, and thrombolysis. JAMA Neurol 2013;70:51-7. [Crossref] [PubMed]
- Du S, Batis C, Wang H, et al. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr 2014;99:334-43. [Crossref] [PubMed]
- Dong G, Sun Z, Zheng L, et al. Prevalence, awareness, treatment, and control of hypertension in rural adults from Liaoning Province, northeast China. Hypertens Res 2007;30:951-8. [Crossref] [PubMed]
- Gungor L, Polat M, Ozberk MB, et al. Which Ischemic Stroke Subtype Is Associated with Hyperhomocysteinemia? J Stroke Cerebrovasc Dis 2018;27:1921-9. [Crossref] [PubMed]
- Schneider S, Kornejeva A, Vibo R, et al. Risk Factors and Etiology of Young Ischemic Stroke Patients in Estonia. Stroke Res Treat 2017;2017:8075697. [Crossref] [PubMed]
- Bi Q, Wang L, Li X, et al. Risk factors and treatment of stroke in Chinese young adults. Neurol Res 2010;32:366-70. [Crossref] [PubMed]
- Krause DN, Duckles SP, Pelligrino DA. Influence of sex steroid hormones on cerebrovascular function. J Appl Physiol (1985) 2006;101:1252-61. [Crossref] [PubMed]
- Ferro JM, Massaro AR, Mas JL. Aetiological diagnosis of ischaemic stroke in young adults. Lancet Neurol 2010;9:1085-96. [Crossref] [PubMed]
- Lekoubou A, Nkoke C, Dzudie A, et al. Recurrent Stroke and Early Mortality in an Urban Medical Unit in Cameroon. J Stroke Cerebrovasc Dis 2017;26:1689-94. [Crossref] [PubMed]
- Kwon SU, Kim JS, Lee JH, et al. Ischemic stroke in Korean young adults. Acta Neurol Scand 2000;101:19-24. [Crossref] [PubMed]
- Nedeltchev K, der Maur TA, Georgiadis D, et al. Ischaemic stroke in young adults: predictors of outcome and recurrence. J Neurol Neurosurg Psychiatry 2005;76:191-5. [Crossref] [PubMed]
- Palm F, Urbanek C, Wolf J, et al. Etiology, risk factors and sex differences in ischemic stroke in the Ludwigshafen Stroke Study, a population-based stroke registry. Cerebrovasc Dis 2012;33:69-75. [Crossref] [PubMed]
- Li F, Yang L, Yang R, et al. Ischemic Stroke in Young Adults of Northern China: Characteristics and Risk Factors for Recurrence. Eur Neurol 2017;77:115-22. [Crossref] [PubMed]
- Kim YD, Choi HY, Cho HJ, et al. Increasing frequency and burden of cerebral artery atherosclerosis in Korean stroke patients. Yonsei Med J 2010;51:318-25. [Crossref] [PubMed]
- Bang OY, Saver JL, Liebeskind DS, et al. Impact of metabolic syndrome on distribution of cervicocephalic atherosclerosis: data from a diverse race-ethnic group. J Neurol Sci 2009;284:40-5. [Crossref] [PubMed]
- Bang OY, Saver JL, Liebeskind DS, et al. Age-distinct predictors of symptomatic cervicocephalic atherosclerosis. Cerebrovasc Dis 2009;27:13-21. [Crossref] [PubMed]