
Functional magnetic resonance imaging-based assessment of terlipressin vs. octreotide on renal function in cirrhotic patients with acute variceal bleeding (CHESS1903): study protocol of a multicenter randomized controlled trial
Introduction
Gastroesophageal variceal bleeding (GVB)/upper gastrointestinal bleeding
Gastroesophageal varices, the most relevant portal-system collaterals, and acute GVB are critical complications that result directly from portal hypertension in patients with liver cirrhosis (1-4). Gastroesophageal varices are present approximately in 50% of patients with cirrhosis. Their presence correlates with the severity of liver disease. Only 40% of Child-Pugh A patients have varices whilst 85% in Child-Pugh C patients (5). Due to remarkable improvements in diagnostic and therapeutic modalities such as vasoactive agents, endoscopic therapy and antibiotics, the overall prognosis has been improved during the past several decades (1,2,6,7). However, it is still associated with increased mortality which is still around 20% within 6 weeks (1-3). Acute GVB is also responsible for a variety of other complications in patients with cirrhosis including acute on chronic liver failure, hepatorenal syndrome, ascites liquid infection and hepatic encephalopathy (8). Therefore, timely and effective control of GVB is of crucial importance for the prognosis in patients with cirrhosis.
Hepatorenal syndrome
In the early stages of cirrhosis, when portal hypertension is moderate, increased cardiac output compensated for a modest reduction in the systemic vascular resistance, ensuring the arterial pressure and effective arterial blood volume to maintain within the normal limits (9,10). Patients with advanced cirrhosis have an intense overactivity of the endogenous vasoactive systems characterized by arterial hypotension and low peripheral vascular resistance (9,11,12). This cascade of events sets the stage for further renal vasoconstriction and renal sodium retention as the splanchnic and systemic vasodilatation worsens with the progression of cirrhosis. Severe renal vasoconstriction in consequence of marked arterial vasodilatation in splanchnic circulation triggers the reduction of glomerular filtration rate (GFR), and thus induces acute kidney injury (AKI)/hepato-renal syndrome (HRS) which may implicate in the increasing mortality in patients with cirrhosis (11,13,14).
Renal functional magnetic resonance imaging (fMRI)
Renal fMRI, a technique considered superior to the most common method used to estimate the GFR, allows for non-invasive, accurate measurements of renal structures and functions in both animals and humans. It has become increasingly prevalent in research and clinical applications. In recent years, renal fMRI has developed rapidly with progress in MRI hardware and emerging post-processing algorithms. Function related imaging markers could be acquired via renal fMRI, encompassing water molecular diffusion, perfusion, and oxygenation. The study will use phase-contrast MR angiography, intravoxel incoherent motion diffusion-weighted imaging (IVIM-DWI) and blood-oxygen-level-dependent (BOLD)-MRI to evaluate renal functional changes after using vasoactive medications in cirrhotic patients undergoing acute variceal bleeding (15-17).
Objective
The Baveno VI guideline recommended standardized, early, aggressive therapeutic strategies for acute GVB in patients with cirrhosis (18). The rationale for the use of vasoactive medications, including terlipressin and octreotide, is to produce splanchnic vasoconstriction and reduce portal blood flow and portal pressure (3,5,19), thereby underpinning the application of these vasoactive drugs in the management of cirrhotic patients with variceal bleeding. Also, terlipressin has been recommended as the international first-line pharmacological therapy for the treatment of HRS on the basis of its pathophysiological feature because terlipressin may improve renal hemodynamics (20,21) and therefore improve renal function in 40–50% patients (21-24). Thus, terlipressin may potentially enable HRS a reversible condition without the need of liver transplantation. However, there haven’t been any randomized controlled trial (RCT) comparing the renal function protection effect of terlipressin and octreotide in the treatment of cirrhotic patients undergoing acute variceal bleeding.
In addition, fMRI can noninvasively reflect the pathophysiological character and dynamically monitor renal parenchyma perfusion and blood oxygen, which makes it particularly valuable in the detection of microcirculation disorders (15). Nevertheless, there haven’t been any research focusing on the ability of fMRI to assess the renal function in cirrhotic patients with acute variceal bleeding. Thus, this research was conducted in order to assess the renal function-protective effect of terlipressin vs. octreotide based on serum creatinine as well as fMRI.
Methods
Study design
This is a multicenter, single-blinded, randomized controlled clinical trial. After screened for eligibility, the participants will be randomly allocated to terlipressin group and octreotide group, meanwhile the laboratory tests (including baseline serum creatinine and cystatin) will be finished and the baseline characteristic will be collected. After the pharmacological intervention, there will be a 90-day follow-up period. All tests and interventions will be performed at involved centers in China: (I) The First Hospital of Lanzhou University; (II) Zhongda Hospital, Medical School, Southeast University; (III) Nanfang Hospital of Southern Medical University; (IV) Guangdong Second Provincial General Hospital; (V) Xingtai People’s Hospital; (VI) The Third Hospital of Zhenjiang Affiliated Jiangsu University; (VII) Tianjin Second People’s Hospital; (VII) The Second Affiliated Hospital of Anhui Medical University; (IX) The Sixth People Hospital of Shenyang; (X) The Second Affiliated Hospital of Baotou Medical University.
Eligibility criteria
Participants involved in this research require compliance with all the inclusion criteria and non-compliance with any exclusion criteria. If the patient meets the below listed criteria and signs the informed consent, the patient is considered eligible for inclusion in this study.
Inclusion criteria
Eligible participants must meet the following criteria: (I) aged between 18–70 years, no restriction on gender; (II) clinically and/or pathologically diagnosed cirrhosis; (III) with a clinical history of GVB (melena, hematemesis, etc.); (IV) assessed as Child-Pugh class B or C; (V) voluntarily participate in the research, willingly to cooperate with the statistic collection process and sign the written informed consent.
Exclusion criteria
Those patients who meet any of the following criteria should be excluded: (I) pregnant or lactating woman; (II) diagnosed or suspected malignancy (hepatocellular carcinoma, cholangiocarcinoma, etc.); (III) with mental disease and unable to comply with MRI examination; (IV) with contraindications of terlipressin and octreotide; (V) with other conditions judged inadequate for participation by the investigators.
Recruitment
Recruitment is conducted from 10 centers in China via: (I) posters, which exhibits the brief information of this research; (II) websites and WeChat official account with multiple forms of dissemination; (III) advice of doctors both from in-patient and out-patient department. The recruitment will continue until the designed sample size is reached.
Patient and public involvement
The development of the research question, outcome measures and burden of intervention did not involve the patient’s eligibility. The final results of the study will be communicated by mail to every participant when published.
Allocation
Randomization will be 1:1 with stratification of Child-Pugh score, age (with 60 years being the dividing line) and gender and will be based on computer-generated secured lists. Eligible participants will be randomly allocated to either terlipressin group and octreotide group after the signed written informed consent is received. The randPack package of R software (R Project for Statistical Computing, Vienna, Austria) will be performed to conduct randomization. If the participant meets the inclusion criteria and agrees to join in the trial, a researcher independent from the intervention will record the participant’s personal information and get the randomized number and group assignment for this participant.
Intervention
Terlipressin
After randomization, participants will begin to receive terlipressin. Terlipressin should be administrated with an initial dose of 1–2 mg intravenously and slowly injected (over 1 minute) while monitoring the heart rate and blood pressure. The maintenance dose should be administrated every 4–6 hours. Each dose of terlipressin is 1 mg. The usual duration of therapy is 3–5 days.
Octreotide
After randomization, participants will begin to receive octreotide. Octreotide should be continuously and intravenously dripped at the speed of 0.025–0.05 mg/h and could be diluted with saline with the maximum duration of 5 days. The usual duration of therapy is 3–5 days.
Outcomes and assessments
Primary outcome
Renal function: number of participants with the improvement of renal function assessed by serum creatinine.
Secondary outcomes
- Renal perfusion: number of participants with the improvement of renal perfusion assessed by fMRI measurement (IVIM).
- Renal blood oxygenation: number of participants with the improvement of renal bold oxygenation assessed by fMRI measurement (BOLD).
- Failure to control bleeding: the occurrence rate of failure to control bleeding.
- Intra-hospital rebleeding: the occurrence rate of intra-hospital rebleeding.
- Intra-hospital mortality: the occurrence of intra-hospital mortality.
- Adverse events (AE): the occurrence rate of AE.
- Overall survival: the number of participants still be alive within the 90-day follow-up.
Assessments
Time nodes of involving measurements to be performed during hospitalization area outlined in Table 1. The following assessments will be conducted and relevant statistic will be collected in participants allocated to each group.
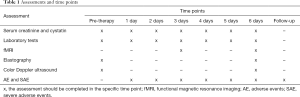
Full table
- General information collection: age, gender, height, weight and ethnic.
- History-taking: past medical history, disease history (with the exact time of the occurrence of GVB, and other complications of cirrhosis including ascites, spontaneous bacterial peritonitis, hepatic encephalopathy, hepatorenal syndrome, etc.), pharmacohistory.
- Clinical diagnosis and etiology of cirrhosis.
- Laboratory test: blood routine examination (red blood cell, white blood cell, haemoglobin, platelet count, etc.), coagulation function (prothrombin time, activated partial thromboplastin time, etc.), liver function (total bilirubin, direct and indirect bilirubin, glutamine transferase, alanine aminotransferase, aspartate aminotransferase, albumin), renal function (serum creatinine and cystatin), blood ammonia and assess Child-Pugh score.
- Record of intake and output volume.
- Color Doppler ultrasound: spleen diameter, portal vein diameter, portal vein velocity, splenic vein velocity, cardiac output, etc.
- Elastography: liver stiffness, spleen stiffness.
- fMRI measurement.
- Examination of neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule 1 (KIM-1), interleukin 18 (IL-18) and liver fatty acid-binding protein (L-FABP), and differentiation from tubular necrosis.
- Record of esophagogastroduodenoscopy results and intervention if available.
- Record of AE and severe adverse events (SAE) of any cause.
Upon occurrence of first variceal bleeding during hospitalization and 90-day follow-up, the following data will be additionally recorded: (I) time of rebleeding since enrollment; (II) cause of rebleeding; (III) intervention and outcome of rebleeding.
Upon death of participants during hospitalization and 90-day follow-up, the following data will be additionally recorded: (I) time of death since enrollment; (II) cause of death.
Sample size estimation
Due to lack of research studies directly comparable to ours, pragmatic considerations have guided the decision to terminate recruitment once a sample of at least 60 volunteers has completed the 90-day follow-up. Because terlipressin is a stronger splanchnic arterial vasoconstrictor than octreotide, it was hypothesized that a certain reduction of serum creatinine could occur in 60% of patients treated with terlipressin and in 30% of those treated with octreotide. Using a 2-tailed test, 30 patients were required in each group for a P value <0.05 with a type I (α) error of 5% and type II (1-β) error of 20%.
Ethics and dissemination
Ethical approval was obtained from all participating centers. Any modifications in protocol will be done under the premise of adequate communication and approval. All interventions and assessments included in this trial will be in full compliance with Good Clinical Practice (GCP).
Before the allocation, all participant candidates will be fully informed about the purpose, process and possible consequences of the trial. Before any treatment, the participants will be informed about the interventions they will undergo and the interventions will not be applied before a written informed consent signed by the participants themselves is provided.
Safety
AE
AE refer to the unintended signs (e.g., abnormal laboratory examination result), symptoms (e.g., nausea, diarrhea) and disease (e.g., GVB) occurring during the trial which may deteriorate the living condition of patients. These AE may not certainly involve with the accepted examination and will be assessed in terms of severity and causality whilst the incidence will also be recorded. The 3-point grading categories will be applied as followed:
- Grade I: mild, without symptoms or with only mild symptoms and do not require treatment.
- Grade II: moderate, consistent with minimum, partial and/or non-invasive treatment indications and with age-related work restrictions on daily life.
- Grade III: severe or medically significant, consistent with hospitalization and/or extended hospitalization indications, disabled and/or with restrictions on self-care ability in daily life.
The causality categories applied will be certain, probably/likely, possible, unlikely, conditional/unclassified and unassessable/unclassifiable.
SAE
AE will be judged as SAE if compliance with any of the following criteria:
- Life-threatening, referring to the condition that participants are in danger of death when AE occur rather than the condition that participants will be in danger of death if AE progress.
- Deadly, if the outcome of an event is “death” then it could be reported and recorded as SAE.
- Resulting in hospitalization or extended hospitalization, the reason leads to this condition should be explicit. It should be AE rather than selective operation or other medical reason.
- Resulting in permanent or significant disability or dysfunction.
- Resulting in malformation if giving birth to a child.
- Other significant medical events.
Data management
For imaging data, the electronic form images will be collected. Other raw data will be recorded in the written form case report form first and saved electronically afterwards. All electronic data will be kept by a member of the study team without direct clinical contact with any of the centers. All written form data will be stored in cabinets with lock permitting access for only investigators. All data will be kept for 25 years after publication and destroyed after then.
Statistical analyses
Statistical analyses were performed with the Statistical Package for Social Sciences version 13.0 (SPSS, Chicago, IL, USA). Statistical significance was established at P<0.05. All P values were two-tailed. Methods for the sample-size calculation are described in the supporting methods. Data are presented as mean ± standard deviation (SD) or number of patients and percentage values. Categorical and continuous variables were compared with the chi-square test and Student’s t-test, respectively. The primary end point for the trial is the renal function. The secondary end point for the trial are (I) renal perfusion; (II) renal blood oxygenation; (III) failure to control bleeding; (IV) intra-hospital rebleeding; (V) intra-hospital mortality; (VI) AE; (VII) overall survival. As mentioned above, primary and secondary study objectives will be analyzed by using a generalized linear mixed model (GLMM), which can take into account the longitudinal structure of the data as well as missing data. The stratification attribute HRS will be included as a covariate in the model and a closed-testing procedure will be used. The multivariate logistic regression analyses were performed to detect independent predictive factors for 90-day treatment failure.
Discussion
Vasoactive drugs including terlipressin and octreotide play a role in the control of variceal bleeding by reducing the portal blood flow and portal pressure (25,26). The results from previous studies indicated that the use of vasoactive drugs was associated with significantly lower risk of mortality and transfusion requirement, and an improved control rate of bleeding up to 75–90% patients (27). Several previous randomized trials and meta-analyses suggested that terlipressin is the only pharmacological agents that provides a survival benefit compared to placebo in patients with cirrhosis (27-29). Nevertheless, many other studies have compared the hemostatic effect of different types of vasoactive drugs and found no difference in mortality rate (30), which is consistent with those of previous researches that analyzed the clinical efficacies of combined therapy of vasoactive drugs and endoscopic procedure (31,32). On the basis of the convincing evidence provided by a large-scale multicenter randomized trial (31), control of bleeding without rescue treatment (89.7%, 88.1%), rebleeding (3.3%, 3.4%) and mortality (8.0%, 8.8%) had no significant difference between terlipressin and octreotide. Thus, in the present multicenter randomized trial, we hypothesized that the application of terlipressin and octreotide in each group may have the similar efficacy in the treatment of acute variceal bleeding. In the meantime, this hypothesis further underpinned the assessment of renal function as a precondition.
Furthermore, to the best of our knowledge, improvement in renal function was associated with a significant increase in arterial pressure, confirming the major relationship between circulatory and renal function in patients with HRS (33-35). A recently published study investigated the effectiveness of terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of HRS (36). The result exhibited that the reduction of serum creatinine of terlipressin group was statistically higher than midodrine/octreotide group with a P value of 0.035. In addition, mean arterial pressure was significantly higher in terlipressin group over midodrine/octreotide group at the time nodes of three days after treatment and mid-point of the treatment period with P value of 0.02 and less than 0.001 respectively. The greater effect of terlipressin treatment on increasing mean arterial pressure may explain the higher efficacy of terlipressin plus albumin over midodrine and octreotide plus albumin in improving renal function. Therefore, we reasonably assumed that terlipressin may have higher effectiveness than octreotide in protecting renal function when administrated to patients with acute variceal bleeding.
Still, this study has several limitations. First, the major cause of cirrhosis of the target population of this study is hepatitis B virus infection while the major etiology source of cirrhosis is alcohol and hepatitis C in American and European countries. Differences in etiology may bring problems in applicability. Second, the period of follow-up in this study is set to be about 90 days, which may not be enough to thoroughly unfold the long-term effect of pharmacological agents.
Acknowledgments
The study was supported by the grant from Wu Jieping Medical Foundation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This trial protocol has been approved by the Ethics Committee from all participating centers. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ibrahim M, Mostafa I, Devière J. New developments in managing variceal bleeding. Gastroenterology 2018;154:1964-9. [Crossref] [PubMed]
- Sauerbruch T, Mengel M, Dollinger M, et al. Prevention of rebleeding from esophageal varices in patients with cirrhosis receiving small-diameter stents versus hemodynamically controlled medical therapy. Gastroenterology 2015;149:660-8.e1. [Crossref] [PubMed]
- Ibrahim M, El-Mikkawy A, Abdel Hamid M, et al. Early application of haemostatic powder added to standard management for oesophagogastric variceal bleeding: a randomised trial. Gut 2019;68:844-53. [Crossref] [PubMed]
- Qi X, Berzigotti A, Cardenas A, et al. Emerging non-invasive approaches for diagnosis and monitoring of portal hypertension. Lancet Gastroenterol Hepatol 2018;3:708-19. [Crossref] [PubMed]
- Garcia-Tsao G, Sanyal AJ, Grace ND, et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007;46:922-38. [Crossref] [PubMed]
- Qi X, An W, Liu F, et al. Virtual hepatic venous pressure gradient with CT angiography (CHESS 1601): a prospective multicenter study for the noninvasive diagnosis of portal hypertension. Radiology 2019;290:370-7. [Crossref] [PubMed]
- Liu F, Ning Z, Liu Y, et al. Development and validation of a radiomics signature for clinically significant portal hypertension in cirrhosis (CHESS1701): a prospective multicenter study. EBioMedicine 2018;36:151-8. [Crossref] [PubMed]
- Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426-37.e1-9.
- Schrier RW, Arroyo V, Bernardi M, et al. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 1988;8:1151-7. [Crossref] [PubMed]
- Arroyo V, Ginès P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club. Hepatology 1996;23:164-76. [Crossref] [PubMed]
- Wong F. Recent advances in our understanding of hepatorenal syndrome. Nat Rev Gastroenterol Hepatol 2012;9:382-91. [Crossref] [PubMed]
- Møller S, Hobolth L, Winkler C, et al. Determinants of the hyperdynamic circulation and central hypovolaemia in cirrhosis. Gut 2011;60:1254-9. [Crossref] [PubMed]
- Salerno F, Gerbes A, Ginès P, et al. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut 2007;56:1310-8. [PubMed]
- Angeli P, Merkel C. Pathogenesis and management of hepatorenal syndrome in patients with cirrhosis. J Hepatol 2008;48 Suppl 1:S93-103. [Crossref] [PubMed]
- Zhou JY, Wang YC, Zeng CH, et al. Renal functional MRI and its application. J Magn Reson Imaging 2018;48:863-81. [Crossref] [PubMed]
- Chang D, Wang YC, Xu TT, et al. Noninvasive identification of renal hypoxia in experimental myocardial infarctions of different sizes by using BOLD MR imaging in a mouse model. Radiology 2018;286:129-39. [Crossref] [PubMed]
- Wang YC, Tang A, Chang D, et al. Significant perturbation in renal functional magnetic resonance imaging parameters and contrast retention for iodixanol compared with iopromide: an experimental study using blood-oxygen-level-dependent/diffusion-weighted magnetic resonance imaging and computed tomography in rats. Invest Radiol 2014;49:699-706. [Crossref] [PubMed]
- de Franchis R, Baveno VI. Faculty. Expanding consensus in portal hypertension: report of the Baveno VI consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol 2015;63:743-52. [Crossref] [PubMed]
- Wells M, Chande N, Adams P, et al. Meta-analysis: vasoactive medications for the management of acute variceal bleeds. Aliment Pharmacol Ther 2012;35:1267-78. [Crossref] [PubMed]
- Ginès P, Guevara M, Arroyo V, et al. Hepatorenal syndrome. Lancet 2003;362:1819-27. [Crossref] [PubMed]
- Sanyal AJ, Boyer T, Garcia-Tsao G, et al. A randomized, prospective, double-blind, placebo-controlled trial of terlipressin for type 1 hepatorenal syndrome. Gastroenterology 2008;134:1360-8. [Crossref] [PubMed]
- Ginès P, Schrier RW. Renal failure in cirrhosis. N Engl J Med 2009;361:1279-90. [Crossref] [PubMed]
- Martín-Llahí M, Pépin MN, Guevara M, et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: a randomized study. Gastroenterology 2008;134:1352-9. [Crossref] [PubMed]
- Gluud LL, Christensen K, Christensen E, et al. Systematic review of randomized trials on vasoconstrictor drugs for hepatorenal syndrome. Hepatology 2010;51:576-84. [Crossref] [PubMed]
- de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol 2005;43:167-76. [Crossref] [PubMed]
- Fernández J, Ruiz del Arbol L, Gómez C, et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology 2006;131:1049-56. [Crossref] [PubMed]
- D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology 1995;22:332-54. [Crossref] [PubMed]
- Söderlund C, Magnusson I, Törngren S, et al. Terlipressin (triglycyl-lysine vasopressin) controls acute bleeding oesophageal varices. A double-blind, randomized, placebo-controlled trial. Scand J Gastroenterol 1990;25:622-30. [Crossref] [PubMed]
- Levacher S, Letoumelin P, Pateron D, et al. Early administration of terlipressin plus glyceryl trinitrate to control active upper gastrointestinal bleeding in cirrhotic patients. Lancet 1995;346:865-8. [Crossref] [PubMed]
- Villanueva C, Piqueras M, Aracil C, et al. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol 2006;45:560-7. [Crossref] [PubMed]
- Seo YS, Park SY, Kim MY, et al. Lack of difference among terlipressin, somatostatin, and octreotide in the control of acute gastroesophageal variceal hemorrhage. Hepatology 2014;60:954-63. [Crossref] [PubMed]
- Abid S, Jafri W, Hamid S, et al. Terlipressin vs. octreotide in bleeding esophageal varices as an adjuvant therapy with endoscopic band ligation: a randomized double-blind placebo-controlled trial. Am J Gastroenterol 2009;104:617-23. [Crossref] [PubMed]
- Boyer TD, Sanyal AJ, Garcia-Tsao G, et al. Predictors of response to terlipressin plus albumin in hepatorenal syndrome (HRS) type 1: relationship of serum creatinine to hemodynamics. J Hepatol 2011;55:315-21. [Crossref] [PubMed]
- Nazar A, Pereira GH, Guevara M, et al. Predictors of response to therapy with terlipressin and albumin in patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 2010;51:219-26. [Crossref] [PubMed]
- Velez JC, Nietert PJ. Therapeutic response to vasoconstrictors in hepatorenal syndrome parallels increase in mean arterial pressure: a pooled analysis of clinical trials. Am J Kidney Dis 2011;58:928-38. [Crossref] [PubMed]
- Cavallin M, Kamath PS, Merli M, et al. Terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: a randomized trial. Hepatology 2015;62:567-74. [Crossref] [PubMed]


