Potential of the glasses-free three-dimensional display system in shortening the learning curve of video-assisted endoscopic surgery: a self-controlled ex-vivo study
Introduction
The video-assisted endoscopic approach, including both thoracoscopic and laparoscopic surgeries, has been rapidly developed and widely adopted for multiple surgical disciplines. However, there is one crucial dilemma facing nearly all surgeons who perform endoscopic surgery: the traditional two-dimensional (2D) display system lacks stereoscopic vision which consequently results in a heavier cognitive workload for surgeons. The most common alternative, the conventional three-dimensional (C-3D) display system requires endoscopic surgeons to adapt to side effects such as fatigue, dizziness, headaches, eyestrain, disorientation, and physical discomfort. Because of this, while most endoscopic surgeons acknowledge the advantages of depth perception with C-3D, they continue using the traditional 2D system.
A glasses-free 3D (GF-3D) display system has been designed with the intent of solving this issue. GF-3D has combined the merits of both 2D and C-3D; surgeons can perform video-assisted endoscopic surgery with a stereoscopic view in lieu of heavy and cumbersome 3D glasses. A stereoscopic image may offer advantages for training surgeons which remains a major concern in this field. One of the largest challenges in endoscopic surgical training is adapting to a flat 2D view. The lack of depth perception is a major sensory loss for surgeons.
In the presented study, junior thoracic surgeons were tested in routine and complex tasks with both a traditional high-definition 2D (HD-2D) display and the GF-3D display to determine whether there was any advantage in using the GF-3D system to acquire thoracoscopic skills.
Methods
Self-controlled study
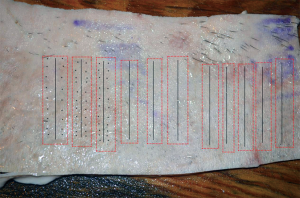
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University. A total of fifteen thoracic surgeons were invited to perform two endoscopic tasks three times each via a GF-3D or HD-2D display system. The fifteen surgeons were divided into two groups: the HD-2D group (n=7) and the GF-3D (n=8) group. The tasks consisted of one routine and one complex procedure. The routine procedure required surgeons to finish a thoracoscopic 5 cm continuous suture on porcine skin (Figure 1). The complex procedure requires surgeons to perform thoracoscopic continuous anastomosis of a transected porcine trachea (1). In both tasks, the participants used the same endoscopic instrumentation to complete the task. These participants had never performed these tasks before the experiment. Completion of the procedures on each display system was performed on separate mornings. Each surgeon was self-controlled to perform the same procedure at the same time every other day, to rule out potential differences in performance.
Establishment of the endoscopic skin continuous suture models
We used one patch of porcine skin attached with an adipose layer and muscle as the endoscopic skin continuous suture material. Each skin patch was bought from the food market and had similar sizes (about 10 cm × 15 cm). The adipose layer and muscle attached to the skin were preserved for further fixtures. An iron frame was applied as a thoracic simulator. Ten parallel lines were drawn vertically on the skin, and 10 dots were drawn on each side of the line. A 5-cm cut was made on the skin along the line. The distance between every dot and the distance between the line and dots were both 5 mm. The skin was placed into the iron frame vertically to imitate the actual surgery for flat suture.
Establishment of the endoscopic tracheal continuous anastomosis models
This model was described in our previous publication (1). We used transected porcine trachea from the throat to the carina as the tracheal continuous anastomosis material. Each trachea was bought from a food market and had a similar length (15 cm) and inside diameter (13 mm). The associated connective tissue along the trachea was removed preoperatively to clear the operative view. An iron frame was applied as the thoracic simulator. The trachea was placed in a position imitating the actual surgery of tracheal reconstruction. The porcine trachea was placed on the thoracic simulator table; the membranous trachea was placed downside. The throat was fixed to the distal end of the simulator table with two traction stitches on each side, while the carina was fixed to the proximal end.
Surgical preparation
For the HD-2D group, a 10-mm 30° thoracoscope (Stryker Corporation, MI, USA) was connected to a display system (Stryker Corporation). For the GF-3D group, a 10-mm 30° thoracoscope (AESCULAP, B. Braun Melsungen AG, Germany) was connected to a display system (AESCULAP, B. Braun Melsungen AG). Based on our previous experience with GF-3D, the AESCULAP 3D scope is the most compatible with our GF-3D display system. The GF-3D system used in this study had a 1,920×1,080 resolution, a 250 cd/m2 brightness, and a less than 4% degree of crosstalk. The specified principle and detailed requirements for projecting the GF-3D image have been previously reported (2). When surgeons focus on the screen, due to different visual angles of each eye, the left and the right eyes receive different pictures superimposed by different subpixels that generate binocular parallax leading to a 3D image (1,2).
This experiment was conducted in the operating room in order to simulate a real surgical environment, thus the temperature and light were constant for each repetition of the experiment. The experiment was conducted three times every other day. The surgeon stood in front of the simulator, and an assistant, the scope holder, stood at the surgeon’s side. For GF-3D, the surgeon wore a special wireless headband, while the assistant wore 3D glasses. During the procedure, the surgeon uses the GF-3D monitor (1). The distance between the GF-3D display system and the principal surgeon is adjusted before the start of the surgical procedure to obtain the sharpest 3D vision. The assistant uses the C-3D monitor (1).
The two procedures were both performed via three ports. For the introduction of the scope (30 degree), an observation port was placed in the middle, and the other two ports were placed beside the observation port. A continuous 17-mm 3-0 prolene (Covidien, Mansfield, MA, USA) suture was used, starting from the right-side dot on the skin and heading to the left-side dot, or from the posterior wall of the trachea and advancing to the anterior wall. The detailed tracheal continuous anastomosis procedure has been previously reported (1). The scope-holder was Yidong Wang from the operation room, who has been a scope-holder for more than 8 years (assisting 750 operations annually). In order to keep homogeneity across the operations, he assisted with every operation.
The 15 participants were timed while performing the procedure. The median time of the participants performing video-assisted thoracoscopic surgery (VATS) was 5 years, ranging from 2 to 10 years. The median operative volume of the participants performing VATS was 210 per year ranging from 120 to 350 per year. The numbers of stitches and distance between stitches were also recorded. In the comparison of operation completion, speed and accuracy of the procedure were determined by speed of suture (stitch/min) and distance deviation between stitches (mm). The speed of suture was calculated as the number of stitches divided by operative time. The ideal distance between stitches was established as 5 mm. The distance deviation of stitches was calculated as every distance between stitches minus 5 mm.
Statistical analysis
Data were processed with SPSS version 16.0. (SPSS, Chicago, IL, USA) and expressed as mean ± standard deviation (SD). Statistical significance was performed using Student’s t-test, the chi-square test, Fisher’s exact test, or one-way repeated measures analysis of variance (ANOVA). A two-sided P value less than 0.05 (P<0.05) was considered to be significant.
Results
All 15 volunteers finished thoracoscopic skin continuous suture and tracheal continuous anastomosis via HD-2D or the GF-3D display system. The median time of the participants performing VATS was 5 years ranging from 2 to 10 years. The median operative volume of the participants performing VATS was 210 per year ranging from 120 to 350 per year.
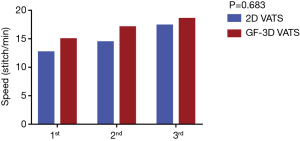
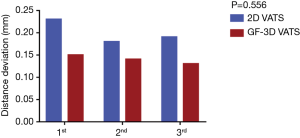
Skin continuous suture
The average time of skin continuous suture of HD-2D was 12.64±2.1, 14.43±2.59, and 17.36±1.49 cm/10 min, while the time of GF-3D was 14.94±1.29, 17.06±2.34, and 18.5±2.07 cm/10 min. There was no significant difference between the two groups in terms of the learning curve for speed (P=0.683) (Figure 2). The average distance deviation of the HD-2D stitches was 0.23±0.13, 0.18±0.75, and 0.19±0.08 mm, while the distance of GF-3D was 0.15±0.04, 0.14±0.04, and 0.13±0.04 mm. There was no significant difference between the two groups in terms of the learning curve for accuracy (P=0.556) (Figure 3).
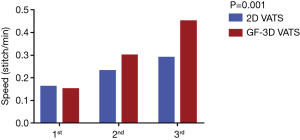
Tracheal continuous anastomosis
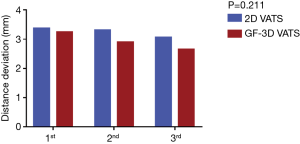
The average time of tracheal continuous anastomosis of HD-2D was 0.16±0.04, 0.23±0.07, and 0.29±0.08 stitch/min, while the time of GF-3D was 0.15±0.04, 0.30±0.06, and 0.45±0.08 stitch/min. There was a significant difference between the two groups in terms of the learning curve for speed (P=0.001) (Figure 4). The average distance deviation of stitches of HD-2D was 3.37±0.56, 3.31±0.60, and 3.06±0.38 mm, while the distance of GF-3D was 3.24±0.34, 2.89±0.26, and 2.64±0.27 mm. There was no significant difference between the two groups in terms of the learning curve for accuracy (P=0.211) (Figure 5).
Discussion
In this self-controlled study, 15 thoracic surgeons from three medical centers with similar experience in the field were divided into two groups to accomplish porcine skin and tracheal anastomosis via HD-2D or GF-3D display systems. The results showed that GF-3D had significant advantages in the learning curve for speed of tracheal continuous anastomosis compared to HD-2D. There was no significant difference between the two groups in terms of the learning curve for accuracy, and no significant difference was observed in the learning curve for speed and accuracy of skin continuous suture between the two groups.
Minimally invasive surgery has shown clear advantages over open surgery in a large number of procedures and has been accepted as the primary approach for multiple techniques. Endoscopy training is important for a novice to become competent with surgical skills. Much attention has traditionally been paid to establishing dedicated training programs (3), training time requirements, or a minimum procedural volume during the training period (4-6). However, attention is rarely paid to display use. Hand-eye coordination is the greatest difficulty within a 2D scenario. For this reason, the learning curve of endoscopic surgery is prolonged (7). The use of a novel display device to overcome the obvious sensory loss for trainees and the lack of depth perception deserves further study.
The use of a 3D display in both clinical work and simulator training makes the whole process more efficient (7,8). Two recent meta-analyses showed that both 3D thoracoscopy (9) and laparoscopy (10) were the preferred surgical option when compared with 2D for surgical time and blood loss. Another prospective study showed that 3D vision shortens the duration of VATS lobectomy (3D 86.22 vs. 2D 107.70 min) (11). The GF-3D display system was designed to increase depth perception and improve accuracy (12) without the need for heavy and cumbersome 3D glasses. The reason we designed this experiment was to find out how much this system could influence our actual practice.
The skin suture task simulated a flat operation, such as lung fissure dissection or lysis of adhesions of pleura. The results here suggest that GF-3D may be less of an advantage for training if the operation can be performed easily or if stereoscopic operation is rarely performed. The tracheal anastomosis task simulated a complex operation, such as complex dissection or vessel or airway reconstruction. This result reveals that the GF-3D could be quite useful for learning complex surgical skills, especially when a stereoscopic operation is commonly performed. There was no significant difference in terms of the learning curve for accuracy of tracheal anastomosis. This may indicate that all the participants are more than qualified in performing this procedure, though they have never performed such operation on their own before.
There were several limitations in this study. First, we only investigated three performance times, and a junior surgeon might not have reached their actual plateau, yet we were still able to observe a significantly steep learning curve for complex tasks in the GF-3D group. Second, our participants could not be blinded to their condition. Third, we did not set-up a failure standard. Because the participants were all junior surgeons, and they were all qualified for these tasks given their daily practice. Last, we operated with ex vivo samples but not live mobile ones, which differs from real surgery on patients. Further studies are required to observe the efficacy in a clinical setting.
In summary, both HD-2D and GF-3D display systems are efficient for routine and complex endoscopic surgery. In vitro, surgeons can acquire new complex endoscopic skills faster via GF-3D than HD-2D. More comparative studies in a clinical setting are needed to further explore the feasibility, necessity, and economic aspects of the GF-3D display system.
Acknowledgments
Funding: This work was supported by the Science and Technology Planning Project of Guangdong Province, China (Grant No. 2014A020215037), and the National Natural Science Foundation of China (Grant No. 81703792).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are responsible for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University.
References
- Liu J, Li J, Liang H, et al. Is the glasses-free 3-dimensional display system more effective for complex video-assisted thoracic surgery? A self-controlled study ex vivo. Surg Innov 2019.1553350619853136. [PubMed]
- Liu J, Cui F, Li J, et al. Development and clinical applications of glasses-free three-dimensional (3D) display technology for thoracoscopic surgery. Ann Transl Med 2018;6:214. [Crossref] [PubMed]
- Verrier ED. Joint Council on Thoracic Surgical Education: an investment in our future. J Thorac Cardiovasc Surg 2011;141:318-21. [Crossref] [PubMed]
- Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 2012;1:47-50. [PubMed]
- Petersen RH, Hansen HJ. Learning thoracoscopic lobectomy. Eur J Cardiothorac Surg 2010;37:516-20. [Crossref] [PubMed]
- Ra YJ, Ahn HY, Kim MS. Learning curve of a young surgeon's video-assisted thoracic surgery lobectomy during his first year experience in newly established institution. Korean J Thorac Cardiovasc Surg 2012;45:166-70. [Crossref] [PubMed]
- Kong SH, Oh BM, Yoon H, et al. Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc 2010;24:1132-43. [Crossref] [PubMed]
- Sakata S, Watson MO, Grove PM, et al. The conflicting evidence of three-dimensional displays in laparoscopy: a review of systems old and new. Ann Surg 2016;263:234-9. [Crossref] [PubMed]
- Liang H, Liang W, Lei Z, et al. Three-dimensional versus two-dimensional video-assisted endoscopic surgery: a meta-analysis of clinical data. World J Surg 2018;42:3658-68. [Crossref] [PubMed]
- Fergo C, Burcharth J, Pommergaard HC, et al. Three-dimensional laparoscopy vs 2-dimensional laparoscopy with high-definition technology for abdominal surgery: a systematic review. Am J Surg 2017;213:159-70. [Crossref] [PubMed]
- Yang CL, Wang W, Mo LL, et al. Short-term outcome of three-dimensional versus two-dimensional video-assisted thoracic surgery for benign pulmonary diseases. Ann Thorac Surg 2016;101:1297-302. [Crossref] [PubMed]
- Ng CSH, He JX, Rocco G. Innovations and technologies in thoracic surgery. Eur J Cardiothorac Surg 2017;52:203-5. [Crossref] [PubMed]