
An adult patient with congenital pulmonary airway malformation and an esophageal cyst
Introduction
Congenital pulmonary airway malformation (CPAM), also referred to as congenital cystic adenomatoid malformation (CCAM), is a rare, non-hereditary abnormality resulting from the cessation of bronchial maturation and concomitant overgrowth of mesenchymal elements (1). CPAM produces an adenomatoid appearance during the sixth and seventh weeks of fetal development. Most CPAM cases are found in neonates or infants, but only a few patients remain asymptomatic until later life. Congenital esophageal cyst is a rare anomaly that occurs during early embryonic development and usually stays in the wall of esophagus or overlies upon the para-esophageal area in the mediastinum. We reported an adult male synchronous with an esophageal cyst and type III CPAM. The main part of the esophageal cyst was located in the lung and in contact with the esophagus simultaneously. To the best of our knowledge, there has been no report of a patient synchronously suffering from both of the above rare abnormities.
Case presentation
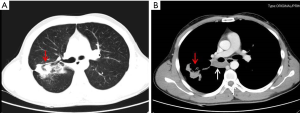
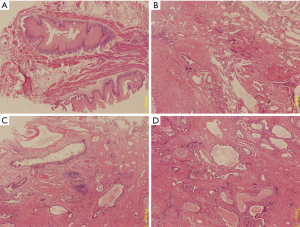
A 31-year-old adult male was admitted to our hospital with an acute episode of fever as high as 38.4 °C and a history of 15-year chronic cough and slight fever. There were no symptoms of dysphagia, dyspnea and hemoptysis previously. His past medical history was significant for pulmonary infection with several times anti-infection treatments administered to alleviate the repeated lung infections. In addition, empirical anti-tuberculous treatment had been implemented for about one year due to persistent lung infiltrates detected by chest X-ray. However, anti-infection and empirical anti-tuberculous treatments did not eliminate neither the symptoms nor the lesion. On admission, contrast-enhanced CT scans of the chest showed a mass involving the posterior segment of the right upper lobe (Figure 1A), and a cystic lesion with an obscure border to the neighboring bronchus and vessels which stayed on the posterior side of the mid-segment bronchus (Figure 1B). Thus, the infections of the right upper lobe and a bronchial cyst were initially considered. Preoperative right upper lung biopsy revealed chronic inflammation. To eliminate the symptoms and make an accurate diagnosis, the patient then received a right upper lobectomy and a complete excision of the cyst lesion via thoracotomy. Inside the resected right upper lobe, a 4.0 cm × 3.0 cm × 2.5 cm solid mass was found. Near the right hilum, there also existed a 3.5 cm × 2.0 cm × 2.0 cm cyst which was full of light yellow mucoid fluid. Microscopically, the cyst lesion was covered with stratified squamous epithelium, beneath which a double muscular layer existed which lacked of cartilage (Figure 2A). The resected solid mass was characterized by developmental abnormality of the lung including poor organized bronchi and blood vessels, and fibrous tissue and small blood vessels hyperplasia (Figure 2B). Multiple small cysts of different sizes were lined by cuboidal or low columnar epithelium. The walls of these small cysts were composed of hyperplastic fibrous tissues instead of smooth muscles (Figure 2C,D). According to the above typical histopathological features, the ultimate diagnosis was type III CPAM associated with an esophageal cyst. The patient had an uneventful post-operative course, was discharged home on the 7th post-operative day and remained uneventful during the 1-year follow-up observation without any complications.
Discussion
CPAM is categorized according to the Stocker et al. (2). Type I CPAM is characterized by single or multiple cysts more than 2 cm in diameter, which is lined by pseudostratified ciliated columnar epithelium and along with mucous cells. Type II CPAM consists of multiple terminal bronchiolar-like uniform cysts smaller than 2 cm in diameter, which is lined by cuboidal to columnar epithelium. Type III CPAM is defined as solid masses with multiple small cysts and consists almost entirely of bronchiolar elements lined by partly ciliated cuboidal epithelium. The new classification system was added type 0 and IV but is not widely applied because type 0 is very difficult to differentiate from bronchogenic cyst, and the similarities between type IV and cystic pleuropulmonary blastoma may result in misdiagnosis (3).
Adult CPAM patients are uncommon, especially for CPAM type III (4). In this report, the patient exhibited chest discomfort and repeated pulmonary infection until he was 16 years old, and the initial diagnosis was chronic pneumonia and tuberculosis. Most cases of CPAM are found in neonates or infants. Nevertheless, a minority of patients remain asymptomatic for years until a bout of recurrent chronic pneumonia resulting in fibrotic changes, cavity lesions or effusion presentations detected by radiology. These features can subsequently lead to misdiagnosis of chronic pneumonia and tuberculosis. According to the Stocker (2) classification, type III CPAM is more commonly reported in stillbirths and is thought to have a worse prognosis (5). In contrast to the poor prognosis of type III CPAM, our case grew up to be healthy and showed no impairment during exercise instead of progressive cardiac failure, and the development of fetal hydrops or intra-uterine demise. We speculate that the type III CPAM lesion in our case might have spontaneously regressed but had not disappeared completely, or fewer cells in embryonic life were affected to produce the relatively small lesion, which could also explain the relatively good prognosis. In addition, we may coincidently present an infrequent case in which a patient suffering from type III CPAM survived by means of conservative management other than surgical treatment during the pre-natal period.
Esophageal cysts involving the right upper lobe bronchus have been reported by Song et al. (6). The esophageal cyst of our case stayed on the posterior side of the mid-segment bronchus and was mainly ectopic in the right lung, resulting in the differential diagnosis between an esophageal cyst and a bronchogenic cyst remains a challenge for radiologists before surgery. In our case, the CT scans were somewhat misleading. Pathologic examination is the most appropriate manner to establish an accurate diagnosis. In the cyst lesion of our patient, the pathological investigations of the stratified squamous epithelium and the two layers of smooth muscle wall without cartilage and glands are consistent with an esophageal cyst. Contrastingly, the most specific microscopic features of a bronchogenic cyst are the wall which is composed of glands, hyaline cartilages, elastic tissues and a single layer of muscle.
The incidence of malignant transformation of CPAM is reportedly between 1% and 3% (7). Associated malignancies with CPAM include rhabdomyosarcoma, pulmonary blastoma and bronchioloalveolar carcinoma. According to the available literature, there have been no previous reports on the relationship of type III CPAM with malignancy. We speculate that the extremely poor prognosis of type III CPAM contributes to the negligible risk for malignant transformation. Types I, II and IV were reported to have a relationship with malignancy. Also, there is overlap between type IV CPAM and type I PPB on pathology. Potential misdiagnosis is with PPB for type IV CPAM and pathologic analysis of the specimen is reliable. A few cases of malignant transformation have also been reported in patients with esophageal cyst and surgical treatment is recommended even in asymptomatic patients (6).
Complete resection is associated with excellent outcome for CPAM and esophageal cyst. Surgery remains the cornerstone treatment for symptomatic patients (8). However, the management of asymptomatic CPAM and esophageal cyst is controversial. Some authors (9,10) supported early surgical treatment for asymptomatic patients as they present better short-term surgical outcomes than symptomatic children, and the long-term natural history of CPAM and esophageal cyst is not well defined. However, those against surgery (10) argue that surgical risk is unreasonable in the large majority of children with small CPAM who remain totally asymptomatic into adulthood. Therefore, elective surgery should be based on multiple factors and a case-by-case decision.
Acknowledgments
Funding: This study was supported by grants from Chengdu City Science and Technology Project of China (No. 0040205301E42) and the National Key Research Project of China (No. 2017YFC0113502).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Shanmugam G, MacArthur K, Pollock JC. Congenital lung malformations--antenatal and postnatal evaluation and management. Eur J Cardiothorac Surg 2005;27:45-52. [Crossref] [PubMed]
- Stocker JT, Madewell JE, Drake RM. Congenital cystic adenomatoid malformation of the lung. Classification and morphologic spectrum. Hum Pathol 1977;8:155-71. [Crossref] [PubMed]
- Feng A, Cai H, Sun Q, et al. Congenital cystic adenomatoid malformation of lung in adults: 2 rare cases report and review of the literature. Diagn Pathol 2012;7:37. [Crossref] [PubMed]
- McDonough RJ, Niven AS, Havenstrite KA. Congenital pulmonary airway malformation: a case report and review of the literature. Respir Care 2012;57:302-6. [PubMed]
- Hasegawa M, Sakai F, Arimura K, et al. EGFR mutation of adenocarcinoma in congenital cystic adenomatoid malformation/congenital pulmonary airway malformation: a case report. Jpn J Clin Oncol 2014;44:278-81. [Crossref] [PubMed]
- Song Z, Peng F, Lin L. Isolated oesophageal cyst connected with the bronchus. West Indian Med J 2007;56:385-7. [PubMed]
- Singh R, Davenport M. The argument for operative approach to asymptomatic lung lesions. Semin Pediatr Surg 2015;24:187-95. [Crossref] [PubMed]
- Kim YT, Kim JS, Park JD, et al. Treatment of congenital cystic adenomatoid malformation-does resection in the early postnatal period increase surgical risk? Eur J Cardiothorac Surg 2005;27:658-61. [Crossref] [PubMed]
- Conforti A, Aloi I, Trucchi A, et al. Asymptomatic congenital cystic adenomatoid malformation of the lung: is it time to operate? J Thorac Cardiovasc Surg 2009;138:826-30. [Crossref] [PubMed]
- Fitzgerald DA. Congenital cyst adenomatoid malformations: resect some and observe all? Paediatr Respir Rev 2007;8:67-76. [Crossref] [PubMed]


