Is early invasive management as ST elevation myocardial infarction warranted in de Winter’s sign?—a “peak” into the widow-maker
Introduction
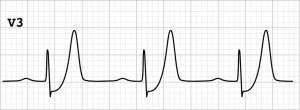
ST elevation in electrocardiographic (EKG) with symptoms consistent with acute coronary syndrome (ACS) has been an accurate indicator of complete coronary artery occlusion resulting in transmural ischemia which warrants primary percutaneous coronary intervention (PPCI) in a timely fashion; with a door-to-balloon time of 90 minutes, in a PCI available facility, and the use of thrombolytics if closest available PCI facility is more than 120 minutes away (1). The criteria for non-ST elevation in EKG to be considered ischemic is new horizontal or down sloping ST depressions ≥0.5 mm in at least two anatomically contiguous leads (2). The need for PPCI is based on risk stratification in non-ST-elevation myocardial infarction (NSTEMI), with a goal of 2 to 72 hours depending on presentation (2). de Winter in 2008 described a new EKG pattern with Nonpattern of acute proximal left anterior descending coronary artery (LAD) occlusion, that warrants immediate PPCI similar to ST-elevation myocardial infarction (STEMI). It typically presents as ST segment depression, upsloping, in general not concerning, in the precordial leads and tall, peaked T waves (3) (Figure 1). The prevalence of this sign noted in acute myocardial infarction was found to be 2% (3,4). This brought to attention of ST depression with peaked T waves should be identified and managed as STEMI to avoid mortality and morbidity.
There has been an influx of many case reports of de Winter’s sign being identified, followed by immediate cardiac catheterization revealing significant, acute occlusion of proximal LAD, treated with stents. Yet, there lacks proper guidelines from American Heart Association (AHA) (1) or European Society of Cardiology (ESC) (5) on the management of this particular EKG sign. LAD, dubbed the widow-maker, involvement increases the risk of patient’s mortality and morbidity with further delay in diagnosis, or management, if it is treated as NSTEMI. Rather, de Winter’s sign warrants early recognition and treatment as a “STEMI equivalent”.
Discussion
We will review the de Winter’s sign EKG characteristics, accuracy in diagnosis, typical patient presentation, and the outcomes of early intervention.
de Winter’s sign
de Winter’s sign was actually first described by Dressler in 1947 where he presented 27 cases of acute myocardial infarction where the initial EKG revealed tall T waves with one case presenting with de Winter’s sign pattern of EKG (6). de Winter described an EKG sign which was characterized by upsloping ST segment depression >1 mm at the J-point in the precordial leads, tall, prominent, symmetric T waves in the precordial leads with absence of ST elevation in the precordial leads, and ST segment elevation (0.5–1 mm) in aVR (1) (Table 1). Based on the analysis of database of PPCI, de Winter found 30 out of 1,532 (2%) patients with acute proximal LAD occlusion on cardiac catheterization presenting with this sign. Verouden’s retrospective analysis also found the prevalence to be at 2% (4).
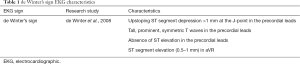
Full table
The electrophysiological mechanism of this EKG pattern presenting without ST elevation is still obscure. de Winter postulated endocardial conduction delay of an anatomical variant of Purkinje fibers. He also suggested an alternate explanation of ischemic ATP depletion leading to lac of activation of sarcolemmal ATP-sensitive potassium (KATP) channels, as demonstrated in animal models of acute ischemia (7). Another proposed mechanism is the involvement of a large area of transmural ischemia that no injury current was generated towards the precordial lead but only aVR (4). An alternate explanation suggests this EKG pattern is caused by subendocardial ischemia as the nidus for changes in subendocardial action potentials with no changes noted in the epicardial action potential. This EKG pattern resolves after revascularization (1).
Accuracy of the sign
de Winter’s sign has been shown to be highly accurate in diagnosing anterior MI caused by acute proximal LAD occlusion. The review by Morris took into consideration 3 retrospective cohort studies to define the accuracy of the de Winter’s sign by positive predictive value (PPV) (8) (Table 2). A small study with 21 patients with de Winter’s EKG pattern of which 20 patients had at least one lesion with angiographic stenosis of >70%. Based on this study, the PPV was 95.2% (95% confidence interval: 76.2–99.9%) (9). Verouden’s analysis of the 35 patients found to have de Winter’s sign had a PPV of 100% (95% confidence interval: 69.2–100.0%) with all of the patients having angiographic evidence of LAD occlusion (4). Misumida found de Winter’s sign corresponding with culprit lesion in the LAD in 6/330 NSTEMI patients with PPV of 100% (95% confidence interval: 51.7–100%) (10). de Winter’s sign has very high PPV for acute coronary occlusion, which will warrant urgent revascularization.
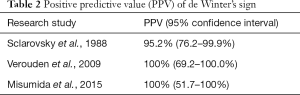
Full table
Patient characteristics
Verouden’s conducted a retrospective analysis of 1,890 patients who underwent PPCI for anterior MI, over a 10-year period (4). Both pre and post procedural EKGs were analyzed. The baseline characteristics of patients presenting with de Winter’s sign when compared to STEMI were found to be younger (mean age of 52 in de Winter’s presentation vs. 61 in STEMI, P=0.001), 33/35 patients being men (de Winter vs. STEMI P=0.002), and having hypercholesteremia (de Winter vs. STEMI P=0.001) (Table 3). Nineteen out of 35 patients were also smokers though it was statistically significant compared to STEMI patients. Another Retrospective study of 441 patients revealed a significant association of family history of coronary artery disease (CAD) in de Winter’s sign (P=0.004) with a prevalence of 3.4% (11).

Full table
The sign electrographically usually manifests approximately 90–100 minutes after symptom onset, with patients presenting with normal sinus rhythm in most cases, and a median heart rate of 75 beats/minute (4,11). Angiography provides evidence of the culprit lesion involving the LAD (1,4), with diffuse multi vessel disease also noted (11). About 50% patients in Verouden’s cohort had “wrap around” LAD artery. Despite after achieving adequate flow after PPCI, patient with de Winter’s sign had considerable loss of myocardium with impairment of LVF (4,11). Also, the time from EKG recording to reperfusion was also increased in the retrospective analysis of Xu et al. (11) (median of 182 minutes), due to lack of recognition, which further conveys the importance of prompt recognition of this sign.
Early cardiac catheterization associated with good outcomes
Ever since the original article, several cases of de Winter’s sign being detected and treated with early PPCI have been reported around the world. Sunbul et al. (12), Zhao et al. (13), Fernandez-Vega et al. (14), Yaranov et al. (15) all describe de Winter’s sign found in younger male patients, 31, 36, 40, and 50 years old respectively, all presenting with chest pain and cardiac catheterization revealing LAD occlusion either followed by immediate reperfusion therapy. The 40-year-old patient on presentation had hemodynamic collapse with initial rhythm being read as ventricular tachycardia and was resuscitated by ACLS protocol status post 3 shocks requiring intubation (14). Associated myocardium damage with loss of left ventricular systolic function was also noted despite prompt recognition and treatment (15). An instance of young female, 34-year-old, smoker with hypercholesterolemia, presenting with de Winter’s sign and getting prompt revascularization has also been reported (16). Thus, signifying that de Winter’s sign can manifest regardless of gender.
Further case reports of de Winter’s sign point towards smoking (16-19), hypercholesterolemia (16), and uncontrolled hypertension (17,19) being the common characteristics noted in these patients as described in the retrospective analysis of de Winter’s sign (4). The real-world scenario of failing to recognize the sign in an emergency room setting and with delay in diagnosis and revascularization has also been reported (20). The patient having significant LAD occlusion, further reiterates the importance of prompt recognition of this sign. The similarity in all these reports were the prompt recognition of the sign, early cardiac catheterization revealing complete or near-complete occlusion of the LAD, and successful resolution of the EKG changes after stenting with good patient outcomes.
Is thrombolysis indicated?
Thrombolysis in de Winter’s sign is controversial, as there is a lack of proper guidelines, and since the present guidelines advocate against thrombolytic therapy in NSTEMI. Xu et al. (11) cautions against the use of thrombolytics in the management of de Winter’s sign. In that retrospective analysis thrombolysis has poor outcomes with two patients failing thrombolysis and one patient having re-occlusion following successful thrombolysis. Thus, the analysis recommends PPCI rather than thrombolysis in manifestation of this sign. But the question looms about thrombolysis being an option in scenarios where immediate PPCI may not be available. Shergill et al. describes a case where a 34-year-old male smoker in India presenting with anginal symptoms and EKG compatible with de Winter’s sign being successfully thrombolysed with streptokinase with relief of symptoms and EKG returning to baseline (21). Thrombolysis was done because of the lack of availability of a cardiac catheterization lab at the facility and financial constraints of the patient. Patient made a successful recovery with mildly depressed LV systolic function in transthoracic echocardiogram and being discharged 5 days after thrombolysis. Thus, the jury is open in terms of thrombolysis in de Winter’s sign with need for more evidence to either favor or avoid thrombolysis in de Winter’s sign.
Conclusions
Current guidelines advocate towards immediate cardiac catheterization laboratory activation in cases of ST-segment elevation and presumed new left bundle-branch block revealed in EKG. But there exists ample evidence of patients presenting with anginal syndrome, ST-segment depression and peaked T waves, combined even in the absence of classic ST-segment elevation in the precordial leads of the 12-lead EKG, having significant LAD occlusion. de Winter’s sign is most often missed by the automated computerized EKG interpretations as well as physicians in the search for the classical ST-segment elevation. This calls for need for educating the physicians interpreting EKGs about de Winter’s sign to facilitate early detection and revascularization. Furthermore, incorporating this pattern into the algorithm of automated computerized EKG interpretation can also aid in diagnosis. Further research and definite guidelines by AHA on de Winter’s sign is a necessity, to address the need for early revascularization and to shed better light on indications of thrombolysis.
Thus, de Winter’s sign, although rare (~2%), should be promptly recognized, as it reveals underlying severe coronary artery pathology, frequently involving the LAD which is associated with a high rate of mortality. This systematic review emphasizes awareness and strong consideration of early activation of the cardiac catheterization lab with PPCI; which may yield better treatment outcomes. The evidence suggests that de Winter’s sign, presenting with upsloping ST segment depression, and prominent T waves in the precordial leads, should indeed be treated as STEMI equivalent, with timely recognition and early revascularization.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78-140. [Crossref] [PubMed]
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014;64:e1-76. [Crossref] [PubMed]
- de Winter RJ, Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion. N Engl J Med 2008;359:2071-3. [Crossref] [PubMed]
- Verouden NJ, Koch KT, Peters RJ, et al. Persistent precordial “hyperacute” T-waves signify proximal left anterior descending artery occlusion. Heart 2009;95:1701-6. [Crossref] [PubMed]
- Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2018;39:119-77. [Crossref] [PubMed]
- Dressler W, Roesler H. High T waves in the earliest stage of myocardial infarction. Am Heart J 1947;34:627-45. [Crossref] [PubMed]
- Li RA, Leppo M, Miki T, et al. Molecular basis of electrocardiographic ST-segment elevation. Circ Res 2000;87:837-9. [Crossref] [PubMed]
- Morris NP, Body R. The De Winter ECG pattern. Eur J Emerg Med 2017;24:236-42. [Crossref] [PubMed]
- Sclarovsky S, Rechavia E, Strasberg B, et al. Unstable angina: ST segment depression with positive versus negative T wave deflections - clinical course, ECG evolution, and angiographic correlation. Am Heart J 1988;116:933-41. [Crossref] [PubMed]
- Misumida N, Kobayashi A, Schweitzer P, et al. Prevalence and clinical significance of up-sloping ST-segment depression in patients with non-ST-segment elevation myocardial infarction. Cardiol Res 2015;6:306-10. [Crossref] [PubMed]
- Xu J, Wang A, Liu L, et al. The de winter electrocardiogram pattern is a transient electrocardiographic phenomenon that presents at the early stage of ST-segment elevation myocardial infarction. Clin Cardiol 2018;41:1177-84. [Crossref] [PubMed]
- Sunbul M, Erdogan O, Yesildag O, et al. De Winter sign in a patient with left main coronary artery occlusion. Postepy Kardiol Interwencyjnej 2015;11:239-40. [Crossref] [PubMed]
- Zhao YT, Huang YS. ECG Pattern Associated with Left Anterior Descending Coronary Artery Occlusion. N Engl J Med. 2018;378:e22. [Crossref] [PubMed]
- Fernandez-Vega A, Martínez-Losas P, Noriega FJ, et al. Winter Is Coming After a Cardiac Arrest. Circulation 2017;135:1977-8. [Crossref] [PubMed]
- Yaranov D, Kairouz V, Patel P, et al. “To Cath or not to Cath…” Rare electrocardiographic presentation of acute myocardial infarction. J Am Coll Cardiol 2018. [Crossref]
- Goktas MU, Sogut O, Yigit M, Kaplan O. A Novel Electrocardiographic Sign of an ST-Segment Elevation Myocardial Infarction-Equivalent: De Winter Syndrome. Cardiol Res 2017;8:165-8. [Crossref] [PubMed]
- Pranata R, Huang I, Damay V. Should de Winter T-Wave Electrocardiography Pattern Be Treated as ST-Segment Elevation Myocardial Infarction Equivalent with Consequent Reperfusion? A Dilemmatic Experience in Rural Area of Indonesia. Case Rep Cardiol 2018;2018:6868204.
- Martínez-Losas P, Fernández-Jiménez R. de Winter syndrome. CMAJ 2016;188:528. [Crossref] [PubMed]
- Goyal KK, Rajasekharan S, Muneer K, et al. de winter sign: A masquerading electrocardiogram in ST-elevation myocardial infarction. Heart India 2017;5:48-50. [Crossref]
- Sheng FQ, He MR, Zhang ML, et al. A STEMI equivalent of de Winter sign missed by an emergency physician. J Electrocardiol 2016;49:620-2. [Crossref]
- Shergill GS, Singh A, Meena NK. de Winters pattern: Spotted and successfully thrombolysed with streptokinase. Heart India 2017;5:157-9.