Nocturnal supports for patients with central sleep apnea and heart failure: a systemic review and network meta-analysis of randomized controlled trials
Introduction
Nowadays, heart failure (HF) is increasingly common, resulting in death in elderly patients (1). A large number of novel regimens developed for HF are palliative rather than curative, so the problems of high morbidity and mortality still exist. The sleep disordered breathing (SDB) is increasingly recognized as a crucial comorbidity in patients with HF, the prevalence of SDB is as high as 50–60% in these patients (2-4). Patients with HF and sleep apnea have poor outcomes, and they have quite poor survival quality.
It is proved that obstructive sleep apnea (OSA) and central sleep apnea (CSA) are both closely associated with HF (5-7). There were some studies about that nocturnal supports could help HF people have quality life shown up (8,9). They raised and developed a theory to use the nocturnal supports to down the incidence of sleep apnea and hypopnea. As a kind of nocturnal supports, CPAP is regarded as a quite useful method to treat OSA, but in patients with CSA, the results of some studies showed that some patients with HF and CSA are quite insensitive to CPAP treatment (10,11).
There were some different kinds of nocturnal supports [adaptive servo ventilation (ASV), continuous positive airway pressure (CPAP), oxygen treatment] being studied in previous researches, however, few network meta-analysis integrated these studies to investigate what kind of nocturnal supports could better help people with HF and CSA. The previous meta-analysis only compared the ASV with other treatments (12). So, we try to conduct the study to guide clinical practice.
Methods
Search strategy
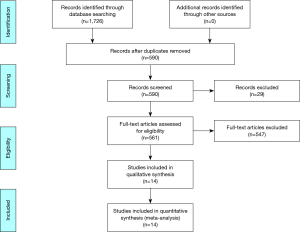
Two authors independently reviewed the identified abstracts and selected articles to full review. The third reviewer addressed the discrepancies. The reference lists of eligible studies and relevant papers were also manually searched and reviewed. The search terms were “central sleep apnea”, “heart failure”. The search date was until 2019/1/22. Finally, we found 1,726 articles, 590 of them existing after excluding duplications, then we excluded 29 articles through reading the title and abstract, and excluded 547 articles through reading the whole articles, finally, 14 RCTs (9,13-25) were included by reading the whole articles (Figure 1).
Inclusion and exclusion
Inclusions contain: (I) researched study about using nocturnal supports for treating patients with HF and CSA, (II) outcome: apnea and hypopnea index, (III) randomized controlled trial (RCTs), (IV) only be published by English.
Exclusions contain: (I) review, retrospective research, case report, (II) insufficient data in the articles.
Data elected
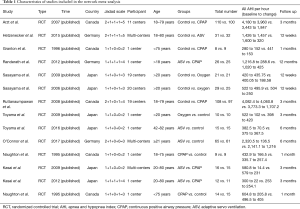
For each selected publication, the following baselines and study characteristics were extracted: first author, publication year, country, participant characteristics, age inclusion, total number of experiment and control group, follow up, and other baseline characteristics of these studies were concluded below (Table 1). Primary outcome measure was the incidence of apnea and hypopnea per hour.
Full table
Risk of bias assessment
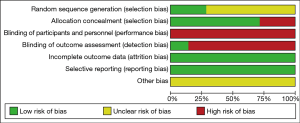
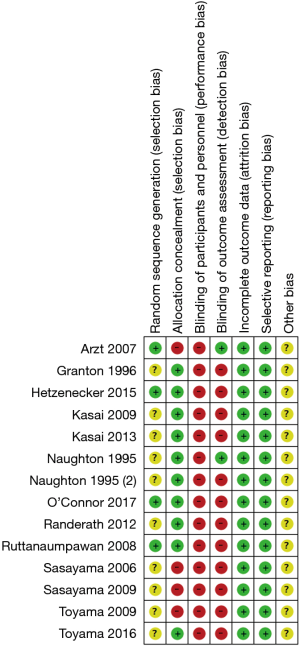
Risk of bias of trials included in this meta-analysis was assessed according to the recommendations of the Cochrane Handbook of Systematic Reviews of Interventions, in the following domains: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), and reporting bias (selective outcome reporting) (http://handbook.cochrane.org). Jadad scale was used to calculate the quality of every enrolled study.
Statistic analysis
We pooled data and used odd ratios (OR) for the dichotomy outcome: the incidence of apnea and hypopnea per hour. The Total numbers of patients occurring apnea and hypopnea per hour were multiplied by 2 to produce new total numbers, which were bigger than the apnea hypopnea index (AHI) multiplied by the number of HF patients in each group. All statistical analyses were carried out with Review Manager 5.3 (The Cochrane Collaboration) and Stata 15.1.
Results
The studies included in our meta-analysis were all RCTs, published from 1995 to 2017. The studies were conducted in Canada (13,14,18,19,22), Germany (16,17,23), and Japan (9,15,20,21,24,25). Table 1 presents the basic characteristics of included trials and demographic data of participants. Seven trials were multicenter studies and the Jadad Scales of all included studies ranged from 2 to 5.
In our study, we totally included 14 RCTs with 919 patients about nocturnal supports in treating patients with HF and CSA to explore which supports can decrease the apnea and hypopnea per hour. The qualities of the article evaluations are as followed (Figures 2,3).
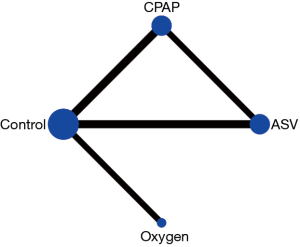
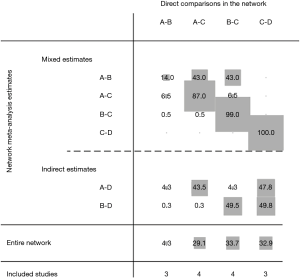
Network evidence of the comparisons between the different nocturnal supports is showed in Figure 4. Compared with the control group, all therapeutic regimens (ASV, oxygen therapy, CPAP) did not decrease the apnea hypopnea per hour in all patients with the OR (95% CI) value of 1.67 (95% CI, 0.49–5.74), 0.32 (95% CI, 0.04–2.55), 2.51 (95% CI, 0.36–17.74), respectively. In addition, there was no significant difference between these therapeutic regimens (Figures 5,6).
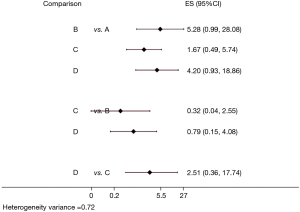
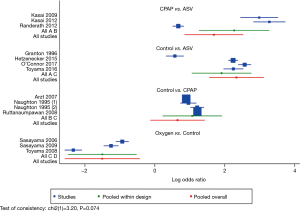
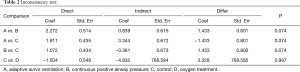
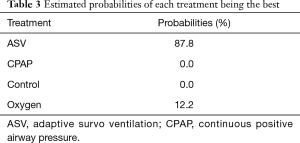
The inconsistency test showed that the comparison could be performed by consistency (P>0.05) (Table 2). In the rank of network meta-analysis, we found that ASV (87.8%) was the most effective nocturnal support to decrease the apnea and hypopnea index, followed by oxygen treatment (12.2%), control (0.0%), CPAP (0.0%) (Table 3).
Full table
Full table
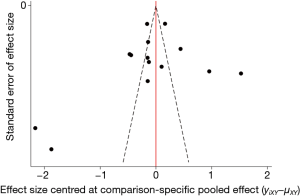
Potential publication bias of nocturnal supports used for treating patients with HF and CSA was performed and showed as funnel plot (Figure 7). Netweight of analysis was showed in Figure 8.
Discussion
In our study, ASV was the best choice treatment used in decreasing AHI in patients with HF and CSA. ASV could also improve cardiac function and quality of life (QOL). What’s more, the mode of ASV could be divided into flow-triggered ASV and volume-triggered ASV. Volume-triggered ASV was probably better in treating patients with central sleep apnea, because the volume-triggered ASV device applied a minimal difference of 3 cmH2O between minimal IPAP and EPAP, and could be better used in patients with coexisting OSA and CSR-CSA (20). The result of the SERVE-HF randomized trial was not included in our study,because it only contained the post-treatment AHI data in patients treated with ASV (26), for generating meta-analysis, we need the post-treatment AHI in both ASV and control group.
According to the previous researches about traditional CPAP mode used for treating patients with HF and central sleep apnea, there were some people un-responsive to CPAP treatment in these articles, which called them complex CPAP and insensitive CPAP (10,11). The results of our study demonstrated that the CPAP was less useful in treating these patients. However, some studies indicated that CPAP could increase transplant-free survival in patients whom CPAP sufficiently suppressed sleep-disordered breathing (SDB) than the control group, showing that CPAP were beneficial to long-term outcomes in the suppressing group (13). On the one hand, CPAP could alter intra-thoracic pressure, cardiac filling pressures, diastolic volumes, and afterload (27). On the other hand, CPAP induced significant reductions of apnea and arousal from sleep, associated with significant reductions of heart rate (28). In addition, from the results of previous study (29), CPAP was the preferred first-line therapy for symptomatic patients with hyperventilation-related CSA.
Nocturnal oxygen treatment also showed superiority in decreasing AHI. The reasons why oxygen could reduce the CSA are multifactorial. Firstly, a rise of PaCO2 leads to a widening difference between the prevailing PaCO2 and the PaCO2 at the apneic threshold. When the difference between these 2 set points is wide, the occurrence of CSA will be suppressed because a large ventilator overshoot is necessary to reduce PaCO2 below the apneic threshold. Moreover, the suppression of the ventilator responses to hypercapnia. Last but not least, increasing the body stores of oxygen probably buffers oscillations in blood gases with each apnea (24).
Our study included all high quality RCTs, excluding studies designed by randomized cross-over trial and retrospective research, so our study is much more reliable to conduct clinical practice. In our study, the best treatment to down AHI could be ASV. AHI decreasing in chronic heart failure (CHF) patients is associated with significant improvements in left ventricular and right ventricular systolic function and reversing left ventricular reconstruction (r-LVR) (30), but the further mortality and morbidity should be discussed.
The American Academy Sleep Medicine (AASM) recommended against using of ASV to treat heart failure-associated CSA in patients with an ejection fraction ≤45% and moderate or severe CSA based on available data (12). In our network meta-analysis, most inclusion criteria of included studies matched to ejection fraction ≤45% however, four of them were different (17,20,21,23).
However, our study also exposes the disadvantages. Firstly, our study excluded the studies comparing with Bi-level ventilation mode because there were no RCTs about this mode of ventilation. Furthermore, the control and CPAP group showed the similar probability of the best choice of treatments, although some patients were insensitive to CPAP, many patients could get benefit from this treatment. Lastly, only 3 of the included studies compared ASV vs. CPAP, whereas all other included studies compared a specific support mode (ASV, CPAP or oxygen) with control.
Conclusions
All in all, we suggest that patients with HF and CSA use nocturnal support treatments to decrease the incidence of apnea and hypopnea, and ASV is probably the best choice of nocturnal support to decrease AHI in these patients, but the specific appropriate patients in ASV treating should be carefully identified according to previous guidelines and studies.
Acknowledgments
We acknowledge all the contributed Authors.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Rich MW, Nease RF. Cost-effectiveness analysis in clinical practice: the case of heart failure. Arch Intern Med 1999;159:1690-700. [Crossref] [PubMed]
- Javaheri S, Parker TJ, Liming JD, et al. Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation 1998;97:2154-9. [Crossref] [PubMed]
- Khayat RN, Jarjoura D, Patt B, et al. In-hospital testing for sleep-disordered breathing in hospitalized patients with decompensated heart failure: report of prevalence and patient characteristics. J Card Fail 2009;15:739-46. [Crossref] [PubMed]
- Oldenburg O, Lamp B, Faber L, et al. Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 2007;9:251-7. [Crossref] [PubMed]
- Corra U, Pistono M, Mezzani A, et al. Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence. Circulation 2006;113:44-50. [Crossref] [PubMed]
- Sin DD, Logan AG, Fitzgerald FS, et al. Effects of continuous positive airway pressure on cardiovascular outcomes in heart failure patients with and without Cheyne-Stokes respiration. Circulation 2000;102:61-6. [Crossref] [PubMed]
- Javaheri S, Shukla R, Zeigler H, et al. Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol 2007;49:2028-34. [Crossref] [PubMed]
- Yoshihisa A, Suzuki S, Miyata M, et al. 'A single night' beneficial effects of adaptive servo-ventilation on cardiac overload, sympathetic nervous activity, and myocardial damage in patients with chronic heart failure and sleep-disordered breathing. Circ J 2012;76:2153-8. [Crossref] [PubMed]
- Toyama T, Seki R, Kasama S, et al. Effectiveness of nocturnal home oxygen therapy to improve exercise capacity, cardiac function and cardiac sympathetic nerve activity in patients with chronic heart failure and central sleep apnea. Circ J 2009;73:299-304. [Crossref] [PubMed]
- Morgenthaler TI, Kuzniar TJ, Wolfe LF, et al. The complex sleep apnea resolution study: a prospective randomized controlled trial of continuous positive airway pressure versus adaptive servoventilation therapy. Sleep 2014;37:927-34. [Crossref] [PubMed]
- Dellweg D, Kerl J, Hoehn E, et al. Randomized controlled trial of noninvasive positive pressure ventilation (NPPV) versus servoventilation in patients with CPAP-induced central sleep apnea (complex sleep apnea). Sleep 2013;36:1163-71. [Crossref] [PubMed]
- Aurora RN, Bista SR, Casey KR, et al. Updated Adaptive Servo-Ventilation Recommendations for the 2012 AASM Guideline: "The Treatment of Central Sleep Apnea Syndromes in Adults: Practice Parameters with an Evidence-Based Literature Review and Meta-Analyses J Clin Sleep Med 2016;12:757-61. [Crossref] [PubMed]
- Arzt M, Floras JS, Logan AG, et al. Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation 2007;115:3173-80. [Crossref] [PubMed]
- Granton JT, Naughton MT, Benard DC, et al. CPAP improves inspiratory muscle strength in patients with heart failure and central sleep apnea. Am J Respir Crit Care Med 1996;153:277-82. [Crossref] [PubMed]
- Toyama T, Hoshizaki H, Kasama S, et al. Adaptive servo-ventilation therapy improves cardiac sympathetic nerve activity, cardiac function, exercise capacity, and symptom in patients with chronic heart failure and Cheyne-Stokes respiration. J Nucl Cardiol 2017;24:1926-37. [Crossref] [PubMed]
- Hetzenecker A, Escourrou P, Kuna ST, et al. Treatment of sleep apnea in chronic heart failure patients with auto-servo ventilation improves sleep fragmentation: a randomized controlled trial. Sleep Med 2016;17:25-31. [Crossref] [PubMed]
- O'Connor CM, Whellan DJ, Fiuzat M, et al. Cardiovascular Outcomes With Minute Ventilation-Targeted Adaptive Servo-Ventilation Therapy in Heart Failure: The CAT-HF Trial. J Am Coll Cardiol 2017;69:1577-87. [Crossref] [PubMed]
- Naughton MT, Benard DC, Liu PP, et al. Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am J Respir Crit Care Med 1995;152:473-9. [Crossref] [PubMed]
- Naughton MT, Liu PP, Bernard DC, et al. Treatment of congestive heart failure and Cheyne-Stokes respiration during sleep by continuous positive airway pressure. Am J Respir Crit Care Med 1995;151:92-7. [Crossref] [PubMed]
- Kasai T, Usui Y, Yoshioka T, et al. Effect of flow-triggered adaptive servo-ventilation compared with continuous positive airway pressure in patients with chronic heart failure with coexisting obstructive sleep apnea and Cheyne-Stokes respiration. Circ Heart Fail 2010;3:140-8. [Crossref] [PubMed]
- Kasai T, Kasagi S, Maeno K, et al. Adaptive servo-ventilation in cardiac function and neurohormonal status in patients with heart failure and central sleep apnea nonresponsive to continuous positive airway pressure. JACC Heart Fail 2013;1:58-63. [Crossref] [PubMed]
- Ruttanaumpawan P, Logan AG, Floras JS, et al. Effect of continuous positive airway pressure on sleep structure in heart failure patients with central sleep apnea. Sleep 2009;32:91-8. [Crossref] [PubMed]
- Randerath WJ, Nothofer G, Priegnitz C, et al. Long-term auto-servoventilation or constant positive pressure in heart failure and coexisting central with obstructive sleep apnea. Chest 2012;142:440-7. [Crossref] [PubMed]
- Sasayama S, Izumi T, Matsuzapki M, et al. Improvement of quality of life with nocturnal oxygen therapy in heart failure patients with central sleep apnea. Circ J 2009;73:1255-62. [Crossref] [PubMed]
- Sasayama S, Izumi T, Seino Y, et al. Effects of nocturnal oxygen therapy on outcome measures in patients with chronic heart failure and cheyne-stokes respiration. Circ J 2006;70:1-7. [Crossref] [PubMed]
- Cowie MR, Woehrle H, Wegscheider K, et al. Adaptive Servo-Ventilation for Central Sleep Apnea in Systolic Heart Failure. N Engl J Med 2015;373:1095-105. [Crossref] [PubMed]
- Fewell JE, Abendschein DR, Carlson CJ, et al. Continuous positive-pressure ventilation decreases right and left ventricular end-diastolic volumes in the dog. Circ Res 1980;46:125-32. [Crossref] [PubMed]
- Hornyak M, Cejnar M, Elam M, et al. Sympathetic muscle nerve activity during sleep in man. Brain 1991;114:1281-95. [Crossref] [PubMed]
- Bradley TD, Logan AG, Kimoff RJ, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med 2005;353:2025-33. [Crossref] [PubMed]
- Kourouklis SP, Vagiakis E, Paraskevaidis IA, et al. Effective sleep apnoea treatment improves cardiac function in patients with chronic heart failure. Int J Cardiol 2013;168:157-62. [Crossref] [PubMed]