
The PD-1/PD-L1 pathway in advanced prostate cancer—have we milked this cow?
We would like to thank Dr. Fay and Dr. Antonarakis for their insightful comments on immunotherapy (IO) in advanced prostate cancer and specifically their commentary on the recently published KEYNOTE-028 study on the use of pembrolizumab in programmed cell death protein-1 ligand (PD-L1) positive metastatic castrate resistant prostate cancer (mCRPC) (1). As described by the authors, monotherapy with checkpoint inhibitors has not demonstrated the dramatic response rates in mCRPC that were shown in other cancer types such as melanoma and non-small cell lung cancer (NSCLC). In particular, our study demonstrated no complete responses (CR) while only 2 (1.5%) PD-L1 positive patients in KEYNOTE-199 had a CR, compared with rates of 5–6% in melanoma treated with pembrolizumab, and higher CR rates with combination IO (2-5). Interestingly, in NSCLC with tumour positive score (TPS) >50%, pembrolizumab monotherapy demonstrated impressive response rates of 39–44%, but the CR rates are low, reported as <1% (6,7). The use of objective response rates in mCRPC to evaluate clinical benefit from experimental therapy (including IO) may not be the most discriminating endpoint to estimate activity in early phase clinical trials (8).
Identification of the subset of patients who respond to checkpoint inhibitors with either tumor-based or circulating biomarkers has long been a goal of researchers in both the pre-clinical and clinical settings. In prostate cancer, responses to IO have been seen in patients with DNA mismatch-repair deficiency, although the frequency of this deficiency is low and estimated to be 3–8% including an acquired microsatellite-unstable phenotype (9,10). Other potential biomarkers for response include mutations in CDK12 or POLE/POLD1 and homologous repair deficiency (11-13). While there has been some success with biomarkers in IO e.g., head and neck squamous cell carcinoma (HNSCC) [combined positive score (CPS) >1%], cisplatin-ineligible bladder cancer (CPS >10%), NSCLC (TPS >50%) and microsatellite instability (MSI)-high disease, identification of biomarkers that sensitize to IO has been limited to very immune-responsive tumors. Markers such as PD-L1 positivity, tumor mutational burden, immune infiltrate or gut microbiome composition present many challenges regarding testing platforms and standardization, with wide variability between different IO agents and patients.
For CRPC, a mainly non-immunoreactive tumor, these efforts to identify a biomarker to IO, while laudable and needed, face many challenges. Therefore, the future of IO in prostate cancer will need to broaden efforts beyond the identification of predictive biomarkers, to explore IO resistance mechanisms and combination strategies to enhance antitumor immunity. Combining IO with non-IO agents has already proven successful in cancers such as small cell lung cancer, renal cell carcinoma and breast cancer (14-16). In prostate cancer, studies are underway examining combinations of IO with non-IO agents to potentiate anti-tumor T cell responses including chemotherapy, hormonal agents and PARP inhibitors (Table 1).
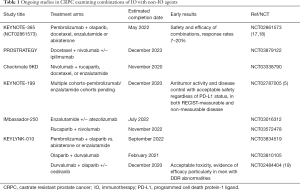
Full table
Numerous agents are in clinical trials to enhance the effects of IO by targeting the innate and adaptive immune systems. Blockade of T-cell receptors such as LAG-3 may upregulate PD-1 and CTLA-4 expression, while combination therapy with IO and anti-LAG-3 antibodies demonstrated activity in mouse models and is currently in phase I/II clinical trials (20,21). Other potential targets include TIM-3, an immune-inhibitory molecule found on T-cells which may be involved in IO resistance (22) and VISTA, an immunomodulatory protein increased on macrophages in IO-treated prostate cancer (23), antibodies to both of which are in early-phase trials in humans. Agonists to molecules such as TLR4, ICOS and CD27 have shown promise in pre-clinical work and phase I/II trials are ongoing (24-26).
Studies are currently examining IO in combination with radiation, with the rationale that radiation may increase antigen release, leading to antigen presentation and immune activation to augment IO response, and also may facilitate the elusive abscopal effect. Pembrolizumab in combination with stereotactic body radiation therapy (SBRT) with or without a TLR9 agonist, which promotes T cell activation and homing, is being studied in patients with castrate-sensitive oligometastatic prostate cancer (NCT03007732). Stereotactic ablative radiotherapy to multiple disease sites in combination with Sipuleucel T in mCRPC is currently in a phase II trial, with results expected early next year (NCT01818986). Numerous oncolytic viruses are in pre-clinical and clinical testing in prostate cancer, using vectors such as adenoviruses or herpes simplex viruses that are modified to preferentially target cancer cells and elicit anti-tumor immunity (27). Therefore these viruses could potentially be combined with IO to further enhance efficacy of both treatments through further immune activation. PROSTVAC is a poxviral-based vaccine which targets PSA as its tumor antigen, and is currently in early-phase trials in combination with nivolumab (NCT02933255), nivolumab/ipilimumab (NCT03532217) and other IO agents (NCT03315871), although PROSTVAC as a single agent has not proven effective in mCRPC (28).
In conclusion, IO remains a therapy with much potential in advanced prostate cancer, but trials to define its clinical benefit are ongoing. Given the tolerable toxicity profile of checkpoint inhibitor monotherapy, combination treatment is a rationale option to improve survival outcomes. While biomarkers for IO response are an attractive prospect in terms of patient selection and personalization of IO treatment, they have proven elusive in many cancers. Combination therapy with IO agents and chemotherapy, hormonal therapy, targeted treatment or even oncolytic virus-based therapy may provide improvements in efficacy by enhancing adaptive immunity, altering the tumor immune microenvironment to promote anti-cancer immune responses through T cell activation and tumor-antigen generation. Beyond identifying a small subset of patients whose tumors are inherently IO-sensitive, manipulating the immune system to turn cold or non-immunogenic tumors such as CRPC into immunoresponsive cancers could prove to be an alternative strategy. This could enable the promise of IO to produce long term durable responses and extend overall survival in mCRPC to be realized.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hansen AR, Massard C, Ott PA, et al. Pembrolizumab for advanced prostate adenocarcinoma: findings of the KEYNOTE-028 study. Ann Oncol 2018;29:1807-13. [Crossref] [PubMed]
- Robert C, Schachter J, Long GV, et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med 2015;372:2521-32. [Crossref] [PubMed]
- Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall Survival with Combined Nivolumab and Ipilimumab in Advanced Melanoma. N Engl J Med 2017;377:1345-56. [Crossref] [PubMed]
- Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N Engl J Med 2018;378:1277-90. [Crossref] [PubMed]
- de Bono JS, Goh JC, Ojamaa K, et al. KEYNOTE-199: Pembrolizumab (pembro) for docetaxel-refractory metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol 2018;36:abstr 5007.
- Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Mok TSK, Wu YL, Kudaba I, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 2019;393:1819-30. [Crossref] [PubMed]
- Scher HI, Morris MJ, Stadler WM, et al. Trial Design and Objectives for Castration-Resistant Prostate Cancer: Updated Recommendations From the Prostate Cancer Clinical Trials Working Group 3. J Clin Oncol 2016;34:1402-18. [Crossref] [PubMed]
- Abida W, Cheng ML, Armenia J, et al. Analysis of the Prevalence of Microsatellite Instability in Prostate Cancer and Response to Immune Checkpoint Blockade. JAMA Oncol 2018. [Epub ahead of print]. [PubMed]
- Nava Rodrigues D, Rescigno P, Liu D, et al. Immunogenomic analyses associate immunological alterations with mismatch repair defects in prostate cancer. J Clin Invest 2018;128:4441-53. [Crossref] [PubMed]
- Antonarakis ES. Cyclin-Dependent Kinase 12, Immunity, and Prostate Cancer. N Engl J Med 2018;379:1087-9. [Crossref] [PubMed]
- Lee L, Ali S, Genega E, et al. Aggressive-Variant Microsatellite-Stable POLE Mutant Prostate Cancer With High Mutation Burden and Durable Response to Immune Checkpoint Inhibitor Therapy. JCO Precis Oncol 2018:1-8.
- Wu YM, Cieślik M, Lonigro RJ, et al. Inactivation of CDK12 Delineates a Distinct Immunogenic Class of Advanced Prostate Cancer. Cell 2018;173:1770-82.e14. [Crossref] [PubMed]
- Horn L, Mansfield AS, Szczesna A, et al. First-Line Atezolizumab plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer. N Engl J Med 2018;379:2220-9. [Crossref] [PubMed]
- Schmid P, Adams S, Rugo HS, et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N Engl J Med 2018;379:2108-21. [Crossref] [PubMed]
- Rini BI, Plimack ER, Stus V, et al. Pembrolizumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N Engl J Med 2019;380:1116-27. [Crossref] [PubMed]
- Yu EY, Massard C, Retz M, et al. Keynote-365 cohort a: Pembrolizumab (pembro) plus olaparib in docetaxel-pretreated patients (pts) with metastatic castrate-resistant prostate cancer (mCRPC). J Clin Oncol 2019;37:abstr 145.
- Fong PC, Retz M, Drakaki A, et al. Keynote-365 cohort C: Pembrolizumab (pembro) plus enzalutamide (enza) in abiraterone (abi)-pretreated patients (pts) with metastatic castrate resistant prostate cancer (mCRPC). J Clin Oncol 2019;37:abstr 171.
- 28. Karzai F, VanderWeele D, Madan RA, et al. Activity of durvalumab plus olaparib in metastatic castration-resistant prostate cancer in men with and without DNA damage repair mutations. J Immunother Cancer 2018;6:141.
- Huang RY, Francois A, McGray AR, et al. Compensatory upregulation of PD-1, LAG-3, and CTLA-4 limits the efficacy of single-agent checkpoint blockade in metastatic ovarian cancer. Oncoimmunology 2016;6:e1249561. [Crossref] [PubMed]
- Andrews LP, Marciscano AE, Drake CG, et al. LAG3 (CD223) as a cancer immunotherapy target. Immunol Rev 2017;276:80-96. [Crossref] [PubMed]
- Koyama S, Akbay EA, Li YY, et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat Commun 2016;7:10501. [Crossref] [PubMed]
- Gao J, Ward JF, Pettaway CA, et al. VISTA is an inhibitory immune checkpoint that is increased after ipilimumab therapy in patients with prostate cancer. Nat Med 2017;23:551-5. [Crossref] [PubMed]
- Shetab Boushehri MA, Lamprecht A. TLR4-Based Immunotherapeutics in Cancer: A Review of the Achievements and Shortcomings. Mol Pharm 2018;15:4777-800. [Crossref] [PubMed]
- Fan X, Quezada SA, Sepulveda MA, et al. Engagement of the ICOS pathway markedly enhances efficacy of CTLA-4 blockade in cancer immunotherapy. J Exp Med 2014;211:715-25. [Crossref] [PubMed]
- He LZ, Thomas LJ, Testa J, et al. Combination therapies augment the anti-tumor activity of agonist CD27 mAb in human CD27 transgenic mouse models. J Immunother Cancer 2013;1:76. [Crossref]
- Lee P, Gujar S. Potentiating prostate cancer immunotherapy with oncolytic viruses. Nat Rev Urol 2018;15:235-50. [Crossref] [PubMed]
- Gulley JL, Borre M, Vogelzang NJ, et al. Phase III Trial of PROSTVAC in Asymptomatic or Minimally Symptomatic Metastatic Castration-Resistant Prostate Cancer. J Clin Oncol 2019;37:1051-61. [Crossref] [PubMed]


