Acupuncture therapy for essential hypertension: a network meta-analysis
Introduction
Essential hypertension is a significant risk factor for cardiovascular disease and stroke, which are the most frequent causes of deaths in the world (1,2). Hypertension has caused a tremendous burden on the overall health of the people of China. A cohort study in 2016 has indicated that among the Chinese population aged between 35 and 79 years old, nearly one-third of cardiovascular deaths were related to a failure in hypertension control (3,4).
Anti-hypertension medication still serves as a major therapy choice for treating hypertension now. However, due to the adverse effects and drug resistance of the medication, there are more and more clinical physicians quickening their expansion to the field of traditional non-pharmaceutical therapy in the practice of hypertension treatment. Acupuncture, a traditional Chinese treatment, can lower blood pressure (BP) by putting needles into certain points on the body. The published study demonstrated that acupuncture could normalize decreased parasympathetic nerve activity (5). This result indicates that the potential mechanism whereby acupuncture can lower BP may be related to the nervous system. In the Web of Science, an international database, there were altogether 202 studies on the application of acupuncture in the treatment of hypertension published until the end of February 2018. The most influential one is the randomized control trial (RCT) published in Circulation (6). At the same time, there were some studies opposed to the application of acupuncture in the treatment of hypertension (7). Therefore, it is still controversial whether or not acupuncture therapy should be used in the clinical treatment of hypertension, hence comprehensive analysis and evaluation of the relevant evidence are still needed. We have systematically collected the evidence of acupuncture for the treatment of hypertension and conducted a pooled analysis to assess the safety and efficacy of acupuncture therapy in the treatment of primary hypertension.
Methods
Inclusion criteria
- Types of study: randomized controlled trials (RCTs) of acupuncture for hypertension;
- Types of patients: patients were diagnosed as having hypertension, and there were no limitations to gender, age, race, or the course of the disease;
- Types of interventions: acupuncture therapy (includes acupuncture, electroacupuncture, moxibustion, and needle warming therapy) with or without concomitant non-acupuncture hypertensive treatment, formed the treatment group, while non-acupuncture hypertensive treatment (life modification, medication), sham acupuncture, and no-treatment were employed in the control group;
- Types of outcomes: primary outcomes were major adverse cardiovascular events (MACE); post-treatment BP changes (BP changes = prior treatment BP value − post-treatment BP value). Secondary Outcomes were the response rate of the treatment (defined as 10 mmHg with a lowering down in SBP or 5 mmHg in DBP) and adverse effects.
Exclusion criteria
- Duplicated literatures;
- Studies only with abstracts and no specific data available;
- Studies neither in Chinese nor English;
- Mutual comparison between different acupuncture methods or different points;
- Studies that employed KPa as the unit of blood pressure and failure in the conversion of original data.
Search strategy
A systematic search was conducted on PubMed, Embase, CENTRAL, CBM, CNKI and Wan-fang Data Database from the inception to February 2018. The following keywords combined with Medical Subject Headings (MeSH) terms were used for searching: “acupuncture” “moxibustion” “electroacupuncture” “needle warming” “hypertension” “high blood pressure” “clinical study” “clinical trial” and “clinical research”. We did not apply any language restrictions. The detailed search strategy (search strategy for PubMed) is listed in Table S1.

Full table
Study selection and data extraction
EndNote X 8.0 software was used to process the management of the literature. Two reviewers (X Tan, Y Pan) screened all the trials for inclusion and conducted the data extraction. An electronic form was established using Excel for data extraction. The main extract content included research topic, author, year of publication, specific information of the treatment groups and control groups, and outcome index. In case of a dispute, adjudication would be done by the third person. In the case of any disagreement between the 2 reviewers, a final decision was made by the third reviewer (H Chen).
Assessment of the risk of bias
Two reviewers (W Su, S Gong) assessed the risk of bias of the included RCTs using the Cochrane Collaboration tool for assessing risk of bias (8). Each trial was scored as high, low, or unclear risk for the following seven domains: “random sequence generation (selection bias)” “allocation concealment (selection bias)” “blinding of participants and personnel (performance bias)” “blinding of outcome assessment (detection bias)” “incomplete outcome data (attrition bias)” “selective reporting (reporting bias)” and “any other bias”. Disagreements were resolved in consultation with the third reviewer (H Chen).
Data synthesis and statistical analysis
As the length of the course of treatment is a clinically relevant factor for the antihypertensive effect, we synthesized the effects based on different course lengths. According to clinical settings, we divided the course treatment lengths into categories, immediacy (within 1 day), short-term (one day to 4 weeks), and long-term (over 4 weeks). All analysis was conducted using Stata 15.0 software (Stata Corporation, College Station, TX, USA) (9,10). For the continuous outcomes, weighted mean difference (WMD) was calculated to pool the effects and odds ratios (OR) for the dichotomous outcomes. First, a pair-wise meta-analysis was conducted using the DerSimonian and Laird method. Second, a network meta-analysis was processed using the mvmeta package of Stata software. The REML Wald test was used to assess the evidence of inconsistency (11). Funnel plots were conducted to assess the small sample size. Results were reported with 95% confidence intervals (CIs), A P<0.05 was considered a significant statistical effect.
Results
Literature searching
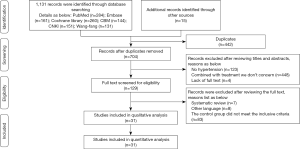
In total, 1,146 pieces of literature were included via the original search, and 442 pieces were excluded due to duplication. After screening for title and abstract, 575 pieces of literature that failed the inclusion criteria were deleted, and after reading the whole text, 98 pieces of studies were removed. Finally, 12 studies (6,12-22) published before and 19 ones (23-41) after 2010 were included (Figure 1).
Characteristics of the included studies
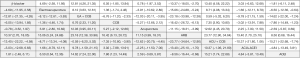
Among the 31 pieces of literature, there were 5 pieces of literature in English (6,20,28,30,34), and 26 in Chinese. The earliest publication was in 2001 (16), and the latest was in 2018 (34). Four studies (27,37,39,41) were three-arm trials, and 27 were two-arm trials. Altogether, 2,649 patients were included in the 31 studies. The outcomes of the included studies were mainly the post-treatment BP value, the response rate of the treatment, and the adverse effects. The characteristics of the included studies are shown in Table 1.
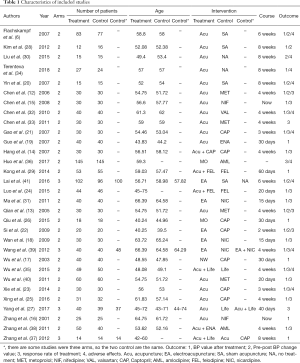
Full table
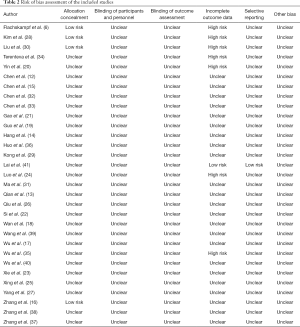
Assessment of the risk of bias
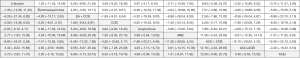
Based on the risk of bias tool, most of the included studies were rated as high risk. Only 4 studies (6,16,28,30) described the detail method of allocation concealment. None of the included studies mentioned the method of blinding. As the protocol of the trials are lacking, it is difficult to assess the attrition bias and the reporting bias (Table 2).
Full table
Results of the network meta-analysis
MACE
None of the included studies evaluated MACE as a primary outcome. Therefore, the pooled-analysis for MACE was not conducted in this review.
Pre-post treatment BP change value (immediacy)
Two studies (15,16) with 110 cases of participants reported an immediate pre-post treatment BP change value. As shown in Figure 2, acupuncture seemed to have a better effect on SBP reduction than CCB at 3, 6, and 60 mins after treatment, while there was no significant difference between acupuncture and CCB at 9, 12, 15, and 30 mins. What is more, CCB may gain much more SBP reduction than acupuncture at 120 mins after treatment (Figure 2A).
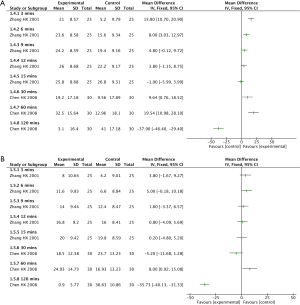
These two studies also reported a DBP reduction in acupuncture and CCB. The results showed that there was no significant difference between acupuncture and CCB at 3, 6, 9, 12, 15, 30, and 60 mins after treatment, while CCB may have a better effect on DBP reduction at 120 mins after treatment (Figure 2B).
Pre-post treatment BP change value (short-term)
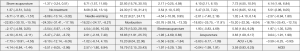
Fifteen studies (12-14,18,21-25,31,32,35,38-40) involving 1,142 cases of participants reported pre-post treatment BP change value after 11 types of short-term treatment (Figure 3). One study (35) which focused on two types of treatments did not form a connected loop with the other therapies. The study reported that acupuncture combined with life modification might gain a larger reduction on both SBP and DBP than life modification alone (MDSBP =10.48, 95% CI: 8.47–12.49; MDDBP =10.38, 95% CI: 8.03–12.73).

The network analysis showed that there was no statistical significance in the inconsistency test of the pre-post BP change for the other 9 therapies (SBP: P=0.6434, DBP: P=0.9001). The pooled results showed that acupuncture seemed to have a better effect on SBP reduction than ARB (MD =11.15, 95% CI: 3.99–18.31) and there was no significant difference on both SBP and DBP reduction between acupuncture and conventional medication (Figures S1,S2). Furthermore, the results showed that acupuncture combined with medication may have more SBP reduction than medication alone (Figure S1), while there was no significant difference between combined therapies and monotherapies on DBP reduction (Figure S2).
Pre-post treatment BP change value (long-term)
Eleven studies (6,17,19,20,26,28-30,34,37,41) with 903 participants reported a pre-post treatment BP change value after 10 types of long-term treatment (Figure 3B). The study compared CCB with acupuncture combined with CCB (29), but it did not form a connected loop with the other 8 types of treatments. This study showed that a combined therapy had a better effect than monotherapy on both SBP and DBP reduction (MDSBP =10.75, 95% CI: 5.70–15.84; MDDBP =5.85, 95% CI: 2.98–8.74).
The network analysis showed that there is no statistical significance of the inconsistency test of the Pre-Post BP change for the other 8 therapies (SBP: P=0.8131, DBP: P=0.5306). The pooled results showed that acupuncture might gain more reduction both on SBP and DBP than sham acupuncture and no-treatment, while there was no significant difference between acupuncture and other monotherapies on BP reduction (Figures S3,S4).

The response rate of treatment (immediacy)
Only one study (15) that compared acupuncture with nifedipine reported the response rate of treatment. It showed that there was no significant difference between acupuncture and nifedipine 30 min after treatment, while a significantly higher response rate was observed in the acupuncture group at 60 min after treatment, and an extremely lower rate in the acupuncture group at 120 mins after treatment (Figure 4).
The response rate of treatment (short-term)
Fifteen articles (12-14,18,22-25,31-33,35,36,39,40) comprising 1,350 cases of participants reported a short-term response rate for the treatment. Twelve types of treatments are worth noting (Figure 5). One study (35), which did not form a loop with the other therapies, reported acupuncture combined with life modification compared with life modification alone. The results showed that the combined treatment seemed to have a higher response rate than monotherapy (OR =4.14, 95% CI: 1.38–12.43). The inconsistency analysis showed that there was no statistical significance (P=0.9142). The pooled results showed that acupuncture seemed to have a higher response rate than β-blockers, and there seemed to be no significant statistical differences between acupuncture and other treatments. The results also demonstrated that combined therapies might have a better effect than monotherapies (Figure S5).
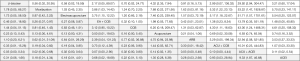
The response rate of treatment (long-term)
Three articles (21,27,38) that involved 266 participants reported a long-term response rate of treatment. Six types of interventions were focused on in these three articles, and four types formed a connected loop (Figure 5B). The pooled results showed that there was no significant difference between the four treatments (Figure 6). The disconnected study which focused on acupuncture combined with CCB and CCB alone also showed that there was no difference between the two treatments (OR =2.4, 95% CI: 0.93–6.16).
Adverse effects
Eleven studies (6,20,21,23,30,32,34-36,39,41) reported adverse effects. Based on these studies, there were few cases of serious adverse effects during acupuncture therapy, which were mainly represented by specific pain or discomfort. As most of the studies failed to report the adverse effects in a standard way (42), it was impossible to conduct a quantitative analysis of the adverse effects in this review.
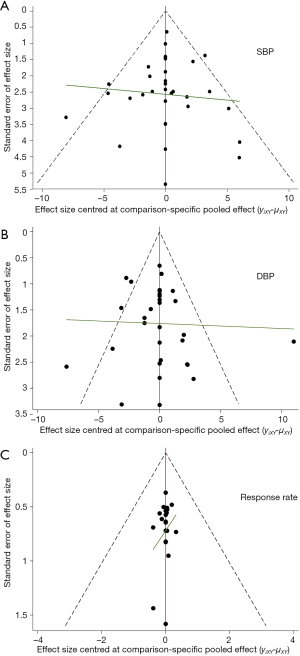
Small sample size effect
As shown in Figure 7, there was a significant small sample size effect between the included studies.
Discussion
The current situation of clinical on acupuncture therapy in the treatment of hypertension
This review included 31 original articles on acupuncture therapy for hypertension. Higher methodological bias risk existed in all of the included studies. Hypertension is a common cardiovascular disease and also an important risk factor for cardiovascular and cerebrovascular diseases. The main target for hypertension control is reducing MACE. MACE and the control rates of BP should be regarded as the main outcomes in the clinical research of hypertension. However, among these original pieces of research included in this meta-analysis, none of the studies focused on this type of indicator. Therefore, it is impossible to evaluate the exact efficacy of acupuncture therapy for hypertension. Additionally, there was little research focusing on the health-economic indicators and patients’ preference for acupuncture in the treatment of hypertension. Thus, it is hard to establish a comprehensive evidence system for acupuncture therapy in the treatment of hypertension (43).
Meanwhile, in the preliminary studies, we found out there is a lack of standardization in the reporting of clinical randomized control trials about acupuncture therapy for the treatment of primary hypertension. They were not reported in accordance with the Consolidated Standards for Reporting of Trials (CONSORT) standard (44) and its expansion version, Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) (45). This made it impossible to acquire accurate partial information, resulting in a loss of readability and credibility of the articles, and a reduction in the evidence quality.
Summary of findings in this review
In this study, we found that it seems likely that acupuncture therapy has a therapeutic effect on hypertension, and, irrespective of being long-term or short-term treatment, there is no significant clinical difference between acupuncture therapies with medication. Moreover, the findings in this review also showed that acupuncture combined with medication might have more BP reduction than medication alone, which demonstrated combined therapy may have a better effect in clinical practice.
Nevertheless, the credibility and precision of the results were not stable, and the evidence quality was very low. Although some of the results showed there to be a significant statistical difference, they still had no clinical difference. The main causes of which were the low quality of the methodological design (such as incomplete allocation concealment), incomplete blinding, small sample size, etc. This bias, taken together, leads to the inability to precisely evaluate the effect of acupuncture for hypertension.
Strength and limitations
Compared with the traditional head-to-head meta-analysis, the results of the direct comparisons and indirect comparisons were taken into account in the network meta-analysis, which can increase the sample size for the final pooled analysis. Until now, there has been no study that has evaluated the efficacy and safety of acupuncture therapy on hypertension based on network meta-analysis. The current study may provide a reference for the clinical practice in the way of a network meta-analysis.
However, due to the likelihood of bias and lack of results assessing the endpoint of hypertension, the value of this review for guiding clinical practice is limited.
Therefore, the precise effects of acupuncture therapy for treating hypertension remain unknown as a consequence of the lack of robust evidence and high overall risk of bias in our included studies.
Conclusions
In conclusion, the existing evidence indicates that the combination of acupuncture with conventional treatment can reduce the BP value of hypertensive patients; there was no statistical and clinical difference between acupuncture and medication. Nevertheless, due to the lower quality of original research, the evidence quality of this conclusion is low, and high quality RCTs with larger sample sizes are still required to assess the efficacy of acupuncture therapy for hypertension.
Acknowledgments
Funding: This work was supported by the Science and Technology Project of Jiangsu Traditional Chinese Medicine Bureau (ID: YB2015006) and the Wuxi Science, Education and Health Young Medical Talents Project (ID: QNRC085).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation 2012;125:e2-220. [PubMed]
- Chobanian AV, Bakris G, Black HR. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 Report, 2003.
- Li Y, Yang L, Wang L, et al. Burden of hypertension in China: A nationally representative survey of 174,621 adults. Int J Cardiol 2017;227:516-23. [Crossref] [PubMed]
- Li D, Lv J, Liu F, et al. Hypertension burden and control in mainland China: Analysis of nationwide data 2003-2012. Int J Cardiol 2015;184:637-44. [Crossref] [PubMed]
- Huang ST, Chen GY, Lo HM, et al. Increase in the vagal modulation by acupuncture at neiguan point in the healthy subjects. Am J Chin Med 2005;33:157-64. [Crossref] [PubMed]
- Flachskampf FA, Gallasch J, Gefeller O, et al. Randomized trial of acupuncture to lower blood pressure. Circulation 2007;115:3121-9. [Crossref] [PubMed]
- Macklin EA, Wayne PM, Kalish LA, et al. Stop Hypertension with the Acupuncture Research Program (SHARP): Results of a randomized, controlled clinical trial. Hypertension 2006;48:838-45. [Crossref] [PubMed]
- Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med 2015;8:2-10. [Crossref] [PubMed]
- Shim S, Yoon BH. Network meta-analysis: application and practice using Stata. Epidemiol Health 2017;39:e2017047. [Crossref] [PubMed]
- Chaimani A, Higgins JP, Mavridis D, et al. Graphical tools for network meta-analysis in STATA. PLoS One 2013;8:e76654. [Crossref] [PubMed]
- White IR, Barrett JK, Jackson D, et al. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods 2012;3:111-25. [Crossref] [PubMed]
- Chen BG, Qian CY, Zhang JN, et al. Clinical observation on the hypotensive effect of point Feng-Chi acupuncture on hypertension. Shanghai J Acupunc and Moxibus 2006;25:15-6.
- Qian CY. A clinical research of the depressurization effect of Acupuncture at Fengchi (GB20) Point in the treatment of hypertension and the influence on IL-6 and ET. Hubei University of Chinese Medicine, 2005.
- Huang F, Yao GX, Huang XL, et al. Clinical observation on acupuncture for treatment of hypertension of phlegm-stasis blocking collateral type. Zhongguo Zhen Jiu 2007;27:403-6. [PubMed]
- Chen HX, Zhang CR, Zhang JS. An observation of short-term therapeutic effect of Acupuncture at Chiqian Point in the treatment of Sub-Acute hypertension. J Emerg Tradit Chin Med 2008;17:1362-3.
- Zhang HX, Zhang TF, Liu YP. Contorl observation on acupuncture of Quchi (LI 11) and Medication in transient action of decreasing blood pressure. Zhongguo Zhen Jiu 2001;21:6-7.
- Wu QM, Feng GX. The correlation between hypotensive effect and plasma Ang II after warm Acu-Moxi Kaisiguan and Bahui points. Journal of New Chinese Medicine 2003;35:45-7.
- Wan WJ, Ma ZY, Xiong XA, et al. Clinical observation on therapeutic effect of electroacupuncture at Quchi (LI 11) for treatment of essential hypertension. Zhongguo Zhen Jiu 2009;29:349-52. [PubMed]
- Guo YH. A clinical observation of Acupuncture in the treatment of hypertension insulin resistance. Acta Chinese Medicine and Pharmacology 2007;35:51-3.
- Yin C, Seo B, Park HJ, et al. Acupuncture, a promising adjunctive therapy for essential hypertension: A double-blind, randomized, controlled trial. Neurol Res 2007;29:S98-103. [Crossref] [PubMed]
- Gao YT. Clinical observation of Acupuncture at Siguan Point, Quchi (LI 11) Point and Xingjian (LR2) Point in the treatment of Yin-Deficiency and Excess Yang type essential hypertension. Hunan University of Chinese Medicine, 2007.
- Si YY. Clinical observation curative effect on electro-aupuncture Quchi and Taichong point treating youth essential hypertension and discussion it's action mechanism. Shandong University of Chinese Medicine, 2009.
- Xie B, Lin YP. Efficacy observation on acupuncture for essential hypertension of yin deficiency due to yang hyperactivity pattern. Zhongguo Zhen Jiu 2014;34:547-50. [PubMed]
- Luo H, Li K. The efficacy of midnight-midday ebb flow acupuncture for treating 44 hypertensive patients. Hunan J Tradit Chin Med 2015;31:80-2.
- Xing H, Zhang Y, Liu XD, et al. Clinical Study of Acupuncture in Treating Essential Hypertension of Accumulation of Phlegm and Dampness. Shandong J Tradit Chin Med 2016;35:802-6.
- Qiu JK, Jin XQ. The clinical research on the Acupuncture at Shenque (CV 8) Point in the treatment of essential hypertension by the principle of guiding fire to the origin. Journal of New Chinese Medicine 2015;47:181-3.
- Yang KD, Zhao XQ. Observation of effect of acupuncture combined with exercise therapy on essential hypertension. Shanxi J Tradit Chin Med 2017;33:26-7, 42.
- Kim HM, Cho SY, Park SU, et al. Can acupuncture affect the circadian rhythm of blood pressure? a randomized, double-blind, controlled trial. J Altern Complement Med 2012;18:918-23. [Crossref] [PubMed]
- Kong L, Song XL. Clinical observations on acupuncture treating the patients of essential hypertension with anxiety state. Tianjin J Tradit Chin Med 2014;31:456-8.
- Liu Y, Park JE, Shin KM, et al. Acupuncture lowers blood pressure in mild hypertension patients: A randomized, controlled, assessor-blinded pilot trial. Complement Ther Med 2015;23:658-65. [Crossref] [PubMed]
- Ma ZY, Wang YF, Wan WJ, et al. The effect of electroacupuncture in Quchi (LI 11) for patients with hypertension on concentration of plasma NPY and NT. Journal of New Chinese Medicine 2011;43:89-91.
- Chen NY, Zhou Y, Dong Q, et al. Observation on therapeutic effect of acupuncture in the treatment of German hypertension patients. Zhen Ci Yan Jiu 2010;35:462-6. [PubMed]
- Chen Q, Chen BG. Clinical Observation on Acupuncture at Quchi (LI 11) and Fengchi (GB 20) for Hypertension. Shanghai J Acupunc and Moxibus 2011;30:659-60.
- Terenteva N, Chernykh O, Sanchez-Gonzalez MA, et al. Acupuncture therapy improves vascular hemodynamics and stiffness in middle-age hypertensive individuals. Complement Ther Clin Pract 2018;30:14-8. [Crossref] [PubMed]
- Wu XM, Li B, Wu B, et al. Effect of puncturing from Baihui(GV20) to Qianding(GV21) with penetrating method on ambulatory blood pressure in grade 1 and 2 primary hypertension. Beijing J Tradit Chin Med 2015;34:931-5.
- Huo Y, Wei YB. Clinical observation on 145 cases of essential hypertension treated by Scar Moxibustion. Guangming J Chin Med 2017;32:2928-30.
- Zhang Y, Liu XG, Dong XY, et al. Clinical research of acupuncture adding psychotherapy in treating essential hypertension. Journal of Chengdu University of Traditional Chinese Medicine 2012;35:16-8.
- Zhang YB. Clinical Research of Acupuncture and medicine in the Treatment of Liver Yang Hyperactivity Type Hypertension. China Journal of Chinese Medicine 2011;26:1397-8.
- Wang YF. Clinical research on the rapeutic effect of electroacupuncture at Quch (LI 11) on blood plasma NPY and NT of essential hypertension patients. Hubei University of Chinese Medicine, 2012.
- Wu YR, Li HX. The clinical observation on acupuncture for treating hypertension. China Medical Herald 2011;8:102-3.
- Lai ZH. Clinical study on the effect of patients expectation to acupuncture for mild essential hypertension. Chengdu University of Chinese Medicine, 2016.
- Ioannidis JP, Evans SJ, Gotzsche PC, et al. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Ann Intern Med 2004;141:781-8. [Crossref] [PubMed]
- Chen H, Wang Y, Jiang WB, et al. The evidence system of traditional Chinese medicine based on the Grades of Recommendations Assessment, Development and Evaluation framework. Ann Transl Med 2017;5:435. [Crossref] [PubMed]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [Crossref] [PubMed]
- MacPherson H, Altman DG, Hammerschlag R, et al. Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med 2010;28:83-93. [Crossref] [PubMed]