
High-flow oxygen therapy for treating re-expansion pulmonary edema
Introduction
Re-expansion pulmonary edema (REPE) is a lethal complication, which usually occurs after rapid re-expansion of a collapsed lung by chest tube insertion. As REPE sometimes induces respiratory failure, adequate treatment is required. We reviewed a case in which a patient with REPE after medical thoracoscopy was treated successfully with a high-flow nasal cannula rather than a mechanical ventilator. The results indicated that use of a high-flow nasal cannula in REPE is advantageous compared to mechanical ventilation.
Case presentation
A 43-year-old man was admitted to our hospital due to a 1-month history of aggravated dyspnea. He had undergone subtotal gastrectomy (Roux-en-Y) 1 year earlier. The final pathological diagnosis was adenocarcinoma, T2N3aM0; adjuvant chemotherapy was performed eight times. Initial vital signs were as follows: pulse rate, 105/min; blood pressure, 130/75 mmHg; respiratory rate, and 25 breaths/min; the room-air pulse oximetry saturation was 96%. Physical examination revealed absence of breath sounds over the right hemithorax. Chest X-ray confirmed the clinical diagnosis of massive pleural effusion in the right hemithorax with a completely collapsed right lung (Figure 1A). Therefore, medical thoracoscopy was performed to drain fluid and diagnose the cause of pleural fluid. A 24 Fr chest tube was then inserted through the sixth intercostal space in the operating room. After medical thoracoscopy, pleural fluid was naturally drained without chest tube clamping.
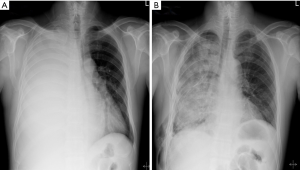
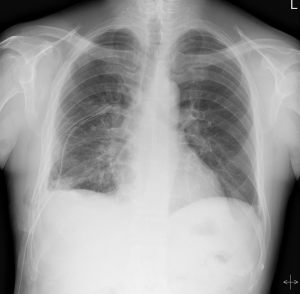
However, 2 hours after tube insertion, the patient began to produce serous yellowish sputum, followed by gradually worsening dyspnea. Oxygen saturation dropped to 86% on supplementation with oxygen at 15 L/min via nasal prongs. Chest X-ray showed diffuse, dense opacification on the right pulmonary field, consistent with severe unilateral REPE (Figure 1B). Despite supplementation of oxygen at 15 L/min via a non-breathing mask, the patient’s condition and symptoms deteriorated progressively and arterial blood gas analysis showed pH 7.382, PaO2 52.3 mmHg, PCO2 32.6 mmHg, and hydrogen carbonate 19.5 mM, 3 hours after chest tube insertion; he was thus transferred to the intensive care unit (ICU). He was not intubated, but received high-flow nasal cannula oxygen therapy with O2 (L/min): 30, FiO2 (%): 60, and low dose diuretics (furosemide) and inotropic agent (dobutamine) was continuously infused for removal of lung fluid and hemodynamic support. The patient had complete uneventful recovery within the next 72 hours and chest X-ray showed resolution of the pulmonary edema (Figure 2). Therefore, he was transferred to the general ward after 4 days with complete resolution of pulmonary edema in the ICU. The final pathological result of pleural biopsy was metastatic adenocarcinoma from gastric cancer. After talc pleurodesis, the chest tube was removed on day 35 of hospitalization and he was discharged on day 38.
Discussion
REPE is a complication that may occur after chest tube insertion, with a reported mortality rate of more than 20%. It is suggested that caution should be required to prevent the occurrence of REPE in the guideline of British Thoracic Society published in 2010 (1). Lung injury develops due to increased endovascular permeability, caused by rapid expansion of the collapsed lung during chest tube insertion. When REPE occurs, ventilation/perfusion mismatch occurs due to the coexistence of the normal part of the lung and the part with the generated edema. Especially, ventilator care is usually necessary in severe hypoxemia; this is because the lung with pulmonary edema has lower compliance than the rest of the lung, such that positive pressure of the ventilator causes excessive expansion of the normal part without adequate ventilation of the edematous part. This results in a decrease in pulmonary artery blood flow in the normal part of the lung and an increase in the edematous part. Ventilator therapy used for oxygen supply may cause deterioration of ventilation/perfusion mismatch, which in turn may increase the risk to the patient during the early treatment period (2).
Therefore, to overcome the initial phenomena associated with ventilator use, it is necessary to supply a high concentration of oxygen using spontaneous ventilation where possible. The application of positive pressure in the alveolar region blocks plasma leakage from the alveoli to the capillary artery and interstitium, and can aid in oxygenation by maintaining a high oxygen concentration in the alveoli. If spontaneous breathing is maintained, it is possible to minimize ventilation/perfusion mismatch due to the ventilator. Noninvasive ventilation (NIV), which is capable of applying positive pressure to the alveoli while maintaining spontaneous breathing, has recently emerged as a method of treatment for REPE (3,4). However, NIV therapy has the disadvantage that effective treatment is difficult if the compliance of the treated patient is low. Therefore, it is difficult to perform NIV without sufficient knowledge of REPE patients with increased anxiety due to acute respiratory distress, and ventilator care is preferred over NIV because of the difficulty of applying the latter method.
Recently, a high-flow nasal cannula has been developed to solve the difficulties of NIV application and is widely used in patients with respiratory difficulty (5,6). A nasal cannula or mask cannot evenly deliver O2 to the alveoli if the respiratory pattern is rough and shallow. However, the high-flow nasal cannula is able to deliver a consistent oxygen supply to the alveoli by constantly applying positive pressure, enabling the patient to maintain a high level of oxygen supply comparable to that obtained using a ventilator.
Considering the clinical features of REPE, we felt that it would be better to apply the high-flow nasal cannula than NIV or a ventilator. The high-flow nasal cannula is an open gas delivery system. The high-flow overcomes labored breathing and generates positive pressure in the alveoli. The difference between the inspiratory volume and the amount of gas delivered to the alveoli is small, and FiO2 is applied relatively consistently. Therefore, high-flow O2 therapy can produce a high positive oxygen concentration in the alveoli by generating positive pressure during spontaneous breathing (7).
In addition, it can be applied promptly in cases of acute dyspnea due to the simplicity of application, because it does not require patient knowledge, in contrast to NIV. We applied high-flow nasal cannulas in the treatment of REPE. Another advantage of the high-flow nasal cannula is that it reduces the duration of treatment. Generally, the period of high oxygen therapy is short, as the dangerous hypoxic state of REPE is not long. However, if a ventilator is used, additional time is needed for weaning off the ventilator, which inevitably increases the duration of treatment. High-flow nasal cannulas can be used to treat patients without ventilator care, thus reducing the duration of treatment. In conclusion, the high-flow nasal cannula, which is widely used for the treatment of respiratory distress, is effective for treatment of REPE because it allows spontaneous breathing while maintaining positive pressure in stable alveoli, and a stable supply of a high concentration of oxygen.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Havelock T, Teoh R, Laws D, et al. Pleural procedures and thoracic ultrasound: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii61-76. [Crossref] [PubMed]
- Mahfood S, Hix WR, Aaron BL, et al. Reexpansion pulmonary edema. Ann Thorac Surg 1988;45:340-5. [Crossref] [PubMed]
- Frat JP, Ragot S, Girault C, et al. Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post-hoc analysis of a randomised trial. Lancet Respir Med 2016;4:646-52. [Crossref] [PubMed]
- Sakellaridis T, Panagiotou I, Arsenoglou A, et al. Re-expansion pulmonary edema in a patient with total pneumothorax: a hazardous outcome. Gen Thorac Cardiovasc Surg 2012;60:614-7. [Crossref] [PubMed]
- Pickard K, Harris S. High flow nasal oxygen therapy. Br J Hosp Med (Lond) 2018;79:C13-c5. [Crossref] [PubMed]
- Atwood CW Jr, Camhi S, Little KC, et al. Impact of Heated Humidified High Flow Air via Nasal Cannula on Respiratory Effort in Patients with Chronic Obstructive Pulmonary Disease. Chronic Obstr Pulm Dis 2017;4:279-86. [Crossref] [PubMed]
- Spoletini G, Alotaibi M, Blasi F, et al. Heated Humidified High-Flow Nasal Oxygen in Adults: Mechanisms of Action and Clinical Implications. Chest 2015;148:253-61. [Crossref] [PubMed]


