Salvage procedures for chronic gastric leaks after sleeve gastrectomy: the role of laparoscopic Roux-en-Y fistulo-jejunostomy
As laparoscopic sleeve gastrectomy (LSG) is nowadays the most popular bariatric procedure in the world, treatment options for managing complications, in particularly gastric leaks, are also emerging (1). Various treatment options for gastric leaks have been described. Key steps in the management of leaks are broad spectrum antibiotic therapy and prompt drainage of the extra-gastric collection, which can be performed by surgical, percutaneous, or endoscopic approaches. Conventional surgical management consisting of relaparoscopy with peritoneal lavage and external drainage is indicated in case of unstable patients with diffuse peritonitis. Nevertheless, further complementary treatment may be required and endoscopy has been proved to be a very valuable tool in our arsenal (2). Conservative endoscopic management with internal drainage, via double pigtail, is often successful for contained gastric leaks in hemodynamically stable patients (3). The success rate is higher when early diagnosis is made (4). Efficient internal drainage creates a favorable pressure gradient, allowing rapid mobilization and removal of external drainage, preventing the formation of a chronic fistula tract. Despite advances in the treatment of gastric leaks after bariatric surgical procedures, chronic leaks and fistula have been reported in the current literature (5,6). Chronic leaks are more challenging to treat due to their persistence (7,8). Treatment failure of these chronic complications is the case in some patients, needing further aggressive management to successfully address this issue once and for all.
A gastric leak after LSG should be considered chronic after 12 weeks and surgical management is then warranted, especially after failure of adequate endoscopic, radiologic and nutritional healing protocols (9). This type of leak will have a lining to the fistula tract and cavity, making it difficult to resolve without surgical intervention. Redo surgery can only take place after an optimal sepsis control and a thorough management of all nutritional deficiencies. Multiple treatment options have been proposed for managing chronic fistulas following LSG. Laparoscopic Roux-en-Y gastric bypass may promote fistula healing by relieving the pressure within the gastric tube (10). However, leaving the fistula tract in very high localization and additional stomach transection close to the inflamed fistula tract remain serious limitations of the approach. Total gastrectomy may treat the problem (11,12), but must be avoided as a first option because of subsequent cumbersome nutritional consequences and relatively high risk of complications related to the oesophago-jejunal anastomosis.
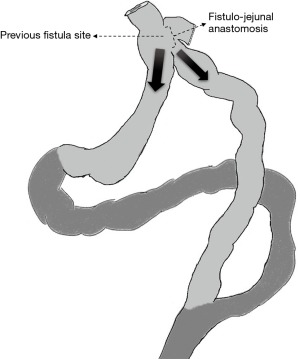
Finally, Roux-En-Y fistulo-jejunostomy (RYFJ) may be the preferred option for the treatment of such chronic gastric leaks or fistulas (Figure 1). It was first described by Baltasar et al. in 2007 (13) and it offers an option for completely controlling the fistula orifice while preserving the remnant gastric tube. Surgical technique has been previously described (14). A laparoscopic approach should be preferred when possible. The dissection of fibrotic adhesions and identification of the fistula orifice at the upper part of the gastric tube remain the most difficult parts of the procedure, leading to conversion in some cases. Dissection of the oeso-gastric junction is better carried out from right to left, using previously non-dissected planes to release and take down the distal third of the oesophagus. When the fistula orifice is isolated, debridement and removal of fibrotic scars is preferred to allow an anastomosis on healthy tissue. Roux limb anastomosis is then performed and a drainage is placed around the fistulo-jejunostomy for postoperative surveillance.
There are numerous other reports describing RYFJ technique and results. Vilallonga et al. presented the safety and efficacy of such an approach in 18 patients with chronic fistulas, with a mean length of hospital stay of 18.4 days (15). Chouillard et al. presented one of the largest series including 21 patients, showing satisfactory fistula control and postoperative results (16). A more recent work reported very good mid-term results, suggesting the durability of fistula healing and weight control (17). The recently published paper by Amor et al. (18) illustrates in the best way the success of LRYFJ for the treatment of chronic fistula after LSG, stretching the safety and effectiveness of this approach. In addition, we fully agree with the authors concluding that it remains a technically challenging procedure that should be reserved to specialized centers.
In conclusion, laparoscopic RYFJ seems to be a good surgical option for the treatment of chronic gastric leaks after LSG. However, it is a challenging procedure and should be performed in experienced bariatric centers by expert bariatric surgeons. Careful patient selection is essential since this approach should only be considered in patients with adequate nutritional status and after failure of a well conducted endoscopic management.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Angrisani L, Santonicola A, Iovino P, et al. IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obes Surg 2018;28:3783-94. [Crossref] [PubMed]
- Kim J, Azagury D, Eisenberg D, et al. ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis 2015;11:739-48. [Crossref] [PubMed]
- Donatelli G, Dumont JL, Cereatti F, et al. Treatment of Leaks Following Sleeve Gastrectomy by Endoscopic Internal Drainage (EID). Obes Surg 2015;25:1293-301. [Crossref] [PubMed]
- Lainas P, Tranchart H, Gaillard M, et al. Prospective evaluation of routine early computed tomography scanner in laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 2016;12:1483-90. [Crossref] [PubMed]
- Parikh M, Issa R, McCrillis A, et al. Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy: a systematic review and meta-analysis of 9991 cases. Ann Surg 2013;257:231-7. [Crossref] [PubMed]
- Rebibo L, Bartoli E, Dhahri A, et al. Persistent gastric fistula after sleeve gastrectomy: an analysis of the time between discovery and reoperation. Surg Obes Relat Dis 2016;12:84-93. [Crossref] [PubMed]
- Thompson CE 3rd, Ahmad H, Lo Menzo E, et al. Outcomes of laparoscopic proximal gastrectomy with esophagojejunal reconstruction for chronic staple line disruption after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 2014;10:455-9. [Crossref] [PubMed]
- Puig CA, Waked TM, Baron TH Sr, et al. The role of endoscopic stents in the management of chronic anastomotic and staple line leaks and chronic strictures after bariatric surgery. Surg Obes Relat Dis 2014;10:613-7. [Crossref] [PubMed]
- Rosenthal RJ. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis 2012;8:8-19. [Crossref] [PubMed]
- Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc 2013;27:240-5. [Crossref] [PubMed]
- Bruzzi M, Douard R, Voron T, et al. Open total gastrectomy with Roux-en-Y reconstruction for a chronic fistula after sleeve gastrectomy. Surg Obes Relat Dis 2016;12:1803-8. [Crossref] [PubMed]
- Martin-Malagon A, Rodriguez-Ballester L, Arteaga-Gonzalez I. Total gastrectomy for failed treatment with endotherapy of chronic gastrocutaneous fistula after sleeve gastrectomy. Surg Obes Relat Dis 2011;7:240-2. [Crossref] [PubMed]
- Baltasar A, Bou R, Bengochea M, et al. Use of a Roux limb to correct esophagogastric junction fistulas after sleeve gastrectomy. Obes Surg 2007;17:1408-10. [Crossref] [PubMed]
- van de Vrande S, Himpens J, El Mourad H, et al. Management of chronic proximal fistulas after sleeve gastrectomy by laparoscopic Roux-limb placement. Surg Obes Relat Dis 2013;9:856-61. [Crossref] [PubMed]
- Vilallonga R, Himpens J, van de Vrande S. Laparoscopic Roux limb placement for the management of chronic proximal fistulas after sleeve gastrectomy: technical aspects. Surg Endosc 2015;29:414-6. [Crossref] [PubMed]
- Chouillard E, Chahine E, Schoucair N, et al. Roux-En-Y Fistulo-Jejunostomy as a salvage procedure in patients with post-sleeve gastrectomy fistula. Surg Endosc 2014;28:1954-60. [Crossref] [PubMed]
- Chouillard E, Younan A, Alkandari M, et al. Roux-en-Y fistulo-jejunostomy as a salvage procedure in patients with post-sleeve gastrectomy fistula: mid-term results. Surg Endosc 2016;30:4200-4. [Crossref] [PubMed]
- Amor IB, Debs T, Dalmonte G, et al. Laparoscopic Roux-En-Y Fistulo-Jejunostomy, a Preferred Technique after Failure of Endoscopic and Radiologic Management of Fistula Post Sleeve Gastrectomy. Obes Surg 2019;29:749-50. [Crossref] [PubMed]