
Surgical management of pectus excavatum in China: results of a survey amongst members of the Chinese Association of Thoracic Surgeons
Introduction
Pectus excavatum is the most common congenital chest wall deformity, affecting 1 to 8 out of 1,000 live births (1). Profiting fully from the advent of the minimally invasive pectus repair, namely the NUSS procedure for pectus excavatum, there has been a dramatic increase in the number of patients presenting for surgery (2). Moreover, a lot of refinements and innovations of the NUSS procedure have arisen, leading to a large variety of new clinical practices (3-5). Inevitably divergences come up in PE surgery about indications, age, surgery strategies, bar-removal timing, anesthesia and rehabilitation, etc. There are no randomized trial or higher level of evidence than case studies to guide thoracic surgeons in this field. This study investigates current clinical practices amongst Chinese Association of Thoracic Surgeon (CATS) members in order to seek potential consensus and divergence to provide possible evidence for further guidelines in guiding clinical practice.
Methods
A web-based questionnaire was designed by a subgroup of CATS Pectus Excavatum Management Working Group, and all CATS members were invited to respond from November 2017 to December 2017.
The questionnaire was designed following a clue focusing on surgical management of pectus excavatum, especially some debatable aspects. The questionnaire was composed of 27 questions, which could be subdivided into sections listed as follows: preoperative evaluations, indications, timing of surgery, anesthesia and analgia, rehabilitation, etc. For some questions multiple options were permitted, while for the others only single option was allowed (see Appendix).
Only fully completed questionnaires by the CATS members were enrolled in the final analysis of this literature.
Data are presented in both numbers and percentages. Percentages are rounded to two decimal places.
Results
Three hundred eighty-five questionnaires were mailed to available CATS members. Moreover, 208 questionnaires were retrieved, of them, 170 were finally available for analysis.
Responders
Of these 170 responders, categorized by the Chinese physician professional title system, 8 (4.71%) responders were resident surgeons, 28 (16.47%) responders were attending surgeons, 67 (39.41%) responders were associate chief surgeons, 64 (37.65%) responders were chief surgeons, and 3 (1.76%) responders were unknown or others.
Preoperative evaluations
For preoperative evaluation of the manners of PE surgery, thoracic CT scan, electrocardiograph and color Doppler echocardiography are deemed mandatory by nearly all of the responders, with a proportion of 98.82%, 91.18% and 89.41% respectively. A pulmonary function test is considered to be necessary by 54.12% of the surveyed cohort. Meanwhile, 34.71% of the responders think psychology assessment should also be undertaken, and another 10% declare that they apply for 3D printing program before surgery. Concerning CT scans, 3D reconstruction of the chest is performed additionally by two thirds (64.12%) of the investigated cohort.
The responders are segregated with regard to the impact of surgery on PE patients accompanied with scoliosis. 15.29% of the responders think that the surgery will lead to an exacerbation of scoliosis. While on the contrary, 25.29% of the responders consider it may lead to a relief of scoliosis, 54.12% consider it to be depending on the severity of scoliosis, 57.65% consider it to be depending on the severity of PE deformity, 51.76% consider it to be depending on the type of the PE deformity, and 57.06% of the responders consider that the effect of PE surgery is related to whether or not the patient undertaking correct postoperative gestures.
Patients’ demands and indications
As for the most common reason that PE patients request for surgery in a surgeons’ daily work, psychological discomfort from PE deformity ranks 1st, with a certification from 56.89% of the responders. Cosmetic requests come second with a proportion of 17.34%. Whereas, only 7.78% responders declare the complaints of obvious cardiopulmonary symptoms to be the most common reason.
Referring to the indications of surgery for PE, a Haller index of >3.25 of thoracic CT scan is agreed by 92.94% of the responders. Restricted pulmonary ventilation disorder, abnormal in ECG and accompanied with mitral valve prolapse are agreed as indications of surgery in 85.29%, 44.12% and 31.76% responders. Severe deformity and ongoing deterioration of deformity are thought to be indications in 84.71% and 75.88% responders. While, severe social-psychological problems from deformity and cosmetic requests are also considered as indications by 89.41% and 49.41% surveyed cohort.
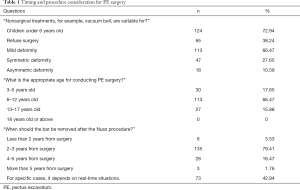
Timing and procedure consideration for PE surgery (see Table 1)
Full table
Nonsurgical treatments, such as vacuum bell, is believed to be suitable for children under 6 years old and mild deformities by 72.94% and 66.47% of the responders.
About the appropriate age to undertake PE surgery, 2 surgeons out of 3 (66.47%) considered the best age interval as 6–12 years old. About 17.65% think it should be 3–5 years old. 15.88% think it should be 13–17 years old, and nobody choose 18 years or older. Moreover, after the Nuss procedure, the majority (79.41%) of the responders agreed on the removal of the bar 2–3 years from surgery. Meanwhile, 42.94% stated that for specific cases, it depends on the individual real-time situation.
When coming to a consideration about adopting open surgery or minimal-invasive surgery, history of thoracic surgery is a concerning factor in 65.88% of the responders. Furthermore, nearly half of the responders emphasize following factors: treatment outcomes, Haller index, the symmetry of deformity and operators’ experience and preference. Only 29.41% considered age as a concerning factor.
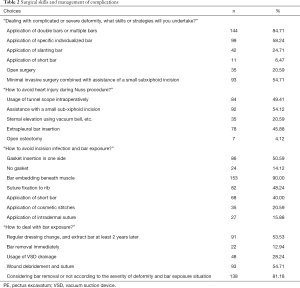
Surgical skills and management of complications
Totally 64.12% of the responders never performed an osteotomy of the sternum or costal cartilage during PE surgery, and only 3.53% do it routinely. Moreover, a small number of surgeons performed it under specific circumstances: in asymmetric deformity (31.76%), in severe deformity (27.06%) and in adults (14.12%).
When coming to talk about the advantage of double bar strategy, 91.18% responders think it provides a better orthopedic effect, and 49.41% for the prevention of a recurrence, 34.12% for the prevention of a bar shifting, 21.76% for the avoidance of an assisted incision or open surgery, 10.00% for less pain. Only 2.94% surgeons refused the double bar strategy. As for the short bar strategy, advantages are as follows: easier for bar removal (62.94%), better cosmetic appearance (35.29%), more stable against bar shifting (24.71%), better orthopedic effect (22.94%), and 16.47% responders consider it has no advantage.
Dealing with complicated or severe deformities, 84.71% of surgeons utilized a double bar or multiple bar strategy and 58.24% indicated the usage of a specific individualized bar strategy (see Table 2).
Full table
The strategies to avoid cardiac injury during the Nuss procedure included the assistance with a small sub-xiphoid incision (54.12%), intraoperative usage of tunnel scope (49.41%), extrapleural bar insertion (45.88%), and so on. Moreover, the strategies to avoid an incision infection and bar exposure contain: bar embedding beneath muscle (90.00%), gasket insertion in one side (50.59), suture fixation to rib (48.24%), application of short bar (40.00%), etc. Dealing with bar exposure, 54.71% responders undertake wound debridement and suture; 53.53% undertake regular dressing change, and extract bar at least 2 years later, etc.
Anesthesia and analgesia for PE surgery
The majority of responders (92.35%) preferred general anesthesia combined with intubation in PE surgery, while other methods such as intravenous anesthesia combined with a laryngeal mask, local anesthesia combined with non-intubation and epidural anesthesia were seldom used or never adopted. As for anesthesia methods adopted in the procedure of Nuss bar removal: 72.35% responders choose general anesthesia combined with intubation, 49.41% intravenous anesthesia combined with a laryngeal mask, 13.53% Local anesthesia, and 7.06 epidural anesthesia. The options of postoperative analgesia methods for PE surgery consist of 75.88% oral, 56.47% intravenous pump, 54.12% intramuscular or intravenous, 18.24% epidural pump, 14.71% paravertebral blockage, and 13.53% peripheral nerve blockage.
Rehabilitation for PE surgery
For preoperative rehabilitation measures, 21.76% of the responders asserted they do not undertake any rehabilitation measures. More than half of the responders declared that they utilized measures like posture training, deep breathing exercise and chest and dorsal muscle exercise, with a proportion of 73.53%, 65.88% and 54.12% respectively.
For ambulation of patients after PE surgery, 39.41% responders gave their permission on POD 1 (1st postoperative day), 38.82% on POD 2–3, 14.71% on POD 4–5, the left 7.06% on POD 6 or above or after discharge. As for non-competitive aerobic exercises, such as running, 10.00% responders permitted it within 4 weeks after surgery, 10.00% 5–7 weeks, 13.53% 8–12 weeks, 59.41% 12 weeks and above, and 7.06% think it should not be allowed until bar removal.
Discussion
Since the wide adoption of the NUSS procedure, more and more patients have received surgery every year, and the abundance of different practices of different surgeons leads to divergencies in those fields including indications, evaluations, surgical skills, anesthesia, rehabilitation, etc.
As for indications, besides complaints of symptoms, a moderate to severe deformity by physical exam, a Haller CT index >3.2, pulmonary function deviance and cardiology evaluation abnormality, Professor NUSS Donald and his colleagues (6) have listed “Poor body image and psycho-social maladjustment” as one of their published six criteria for patients who are deemed suitable candidates for NUSS procedure. In this study, severe social-psychological problems from deformity and cosmetic request are considered as indications for PE surgery by 89.41% and 49.41% of the surveyed cohort. Meanwhile, as for reasons of PE patients’ request for surgery in surgeons’ daily outpatient, cosmetic request and psychological discomfort from deformity together possess the most common reason in 72.46% responders. This elucidates that, besides physiological factors (shortness of breath, palpitation, and so on), psychological factors (body image, discomfort, low self-esteem, and so on) play a more and more indispensable role in decision making of PE surgery for both surgeons and patients. Several studies (7-9) have shown an obvious improvement of emotional well-being, self-esteem, body image, etc. In this study, 34.71% of the surveyed cohort thinks that psychology assessment should also be undertaken routinely before surgery.
There is a controversy in the consideration about the timing of surgery. It is still debatable whether the patients should receive surgery before adolescence, peri-adolescence, or after adolescence. It is easy to comprehend that as patients grow elder, particularly in adults, their chest cages become stiffer, which may increase the difficulty of PE surgery and diminish the orthopedic effect. However, surgery as early as possible is neither advised. Thoracic surgeons (10) have noted the flexibility and malleability of the chest wall in young children, and they found that too early surgery might lead to disturbance in the development of children’s chest cages. Besides, Haller and colleagues (11) have found the side effects of too early and extensive PE surgery in young children, and they recommend a delay in operative repair in small children until at least 6 to 8 years old, with the median age of 14 years. When talking about the timing of bar removal procedure, NUSS and his colleagues (12) have concluded that: if the bar is removed too soon, the recurrence rate will increase; the bar should be removed 3 years later in order to gain an ideal recurrence rate. In this survey, children under 6 years old are believed to be suitable for nonsurgical treatments, such as vacuum bell, by 72.94% of the responders. Nearly 2 surgeons out of 3 (66.47%) consider the most appropriate age interval to undertake PE surgery is 6–12 years old. Moreover, after the Nuss procedure, the majority (79.41%) of the responders agree on the removal of the bar 2–3 years from surgery.
As previously stated, there have been more and more refinements and innovations in the field of the NUSS procedure, as a result of the prevalence of the NUSS procedure itself. These modifications are mostly aimed at minimizing potential complications (13), like cardiac injury and bar displacement. The key point to prevent cardiac injury is to create a sufficient view of substernal space to perform a safe dissection through it. Moreover, many manners have evolved, such as usage of thoracoscopy, including tunnel scope and bilateral thoracoscopy; assistance with a subxiphoid incision (14); sternal elevation (15) using vacuum bell, Crane Technique, etc. Utilization of stabilizers and fixation techniques (16) have helped reduce postoperative bar displacement rate; and so does double or multiple bar strategy (17). We find that, in our survey, about half of the responders undertake cardiac injury prevention strategies including tunnel scope, a subxiphoid incision, and sternal elevating means. Only 84.71% of the responders agree on the application of double or multiple bar strategy when dealing with complicated or severe deformity.
General anesthesia combined with intubation is widely considered as a standard maneuver in PE surgery (18), and this is confirmed in this survey, with a proportion as high as 92.35%. For bar removal procedure, nearly half of the responders also list intravenous anesthesia combined with the laryngeal mask as an alternative, which is believed to be of similar safety and feasibility (19). Varieties of postoperative analgesia methods are adopted in both our survey and other studies (20-22).
It is found that postoperative rehabilitation may improve postoperative pulmonary function (23), and may help adjust postoperatively forced posture, known as “round back” (24). It is suggested that (25) we should encourage patients’ ambulation on POD 1; and permit non-competitive aerobic exercises 6 weeks after PE surgery. In our survey, preoperative rehabilitation, postoperative early-stage ambulation and exercises are deemed as necessary maneuvers by the majority of the responders. However, a divergence exists in aspects like ambulation timing, and this may reflect that we lack enough concern for rehabilitation.
This survey provides a time-sensitive perspective of clinical practices in PE surgery at the moment. Moreover, this “self-report” study bears several limitations. We sent 385 questionnaires, but retrieved only 170 available feedbacks, elucidating a relatively low efficient responding rate. This may due to that they were too busy to reply, or they delayed their feedback beyond the deadline of 7 days since delivery. Meanwhile, the responders cannot represent all surgeon’s choice nationwide, for some may conduct tens or hundreds of PE surgery yearly while others just several cases. Bias may arise in the feedback data of the survey, depending on how true and accurate the responders are. This survey cannot cover every aspect of PE surgery. Moreover, some questions of the questionnaire could be modified to gain more objective results. Further studies are needed to establish clinical practice guidelines for thoracic surgeons in PE surgery.
This survey reveals a remarkable consistency of practice patterns in several aspects, and the given results can be used as evidence in guiding clinical practice in circumstances where no evidence of higher levels exists, although divergences exist. Future studies, especially randomized trials, are needed to establish clinical practice guidelines for thoracic surgeons in PE surgery.
Supplementary
CATS Pectus Excavatum Management Working Group Questionnaire
Attention: be aware of single choice or multiple choices.
- Your hospital belongs to (in Chinese Hospital Grade System) (Single choice)
- Grade III hospital
- Grade II hospital
- Children specialized hospital
- Others
- What is your title by the Chinese physician professional title system? (Single choice)
- Resident surgeon
- Attending surgeon
- Associate chief surgeon
- Chief surgeon
- Others
- What is number of pectus excavatum (PE) surgery or other chest deformities in your department yearly? (Single choice)
- Less than 10 cases
- 10-30 cases
- 31-50cases
- More than 50 cases
- Which is the most common reason for PE patients’ demands for surgery in your daily work? (Single choice)
- Complaints of obvious cardiopulmonary symptoms
- Cosmetic request
- Psychological discomfort from deformity
- Recommendation from pediatrician or physician
- Self-recognition of PE by the means of internet, etc
- Easily catching a cold or fever
- Will you perform surgery on mild deformity PE patients for their cosmetic requests? (Single choice)
- Yes
- No
- Depends on real-time circumstances
- In your opinion, nonsurgical treatments, for example, vacuum bell, are suitable for? (Multiple choices)
- Children under 6 years old
- Refuse surgery
- Mild deformity
- Symmetric deformity
- Asymmetric deformity
- Preoperative evaluation of PE surgery should include? (Multiple choices)
- Thoracic CT scan
- X-ray chest radiography
- Pulmonary function test
- Electrocardiograph
- Color doppler echocardiography
- Psychology assessment
- 3D printing
- For 3D reconstruction of chest by CT scan, should it be performed routinely? (Single choice)
- Yes
- No
- What’s your Indications of surgery for PE? (Multiple choices)
- Cosmetic request
- Haller index >3.25
- Abnormal in electrocardiograph (ECG)
- With mitral valve prolapse
- Severe deformity
- Ongoing deterioration of deformity
- Restricted pulmonary ventilation disorder
- Severe social-psychological problems from deformity
- What is the impact of surgery on PE patients accompanied with scoliosis? (Multiple choices)
- Exacerbation of scoliosis
- Relief of scoliosis
- It depends on the severity of scoliosis
- It depends on the severity of PE deformity
- It depends on the type of PE deformity
- It depends on whether patients holding onto the correct postoperative gestures
- What’s the appropriate age for conducting PE surgery? (Single choice)
- 3–5 years old
- 6–12 years old
- 13–17 years old
- 18 years old or above
- What’s your preoperative rehabilitation measure? (Multiple choices)
- None
- Deep breathing exercise
- Chest and dorsal muscle exercise
- Dietary management
- Posture training
- Others
- Which is your most preferred anesthesia method in PE surgery? (Single choice)
- Local anesthesia + non-intubation
- Epidural anesthesia
- General anesthesia + intubation
- Intravenous anesthesia + laryngeal mask
- Which factor will you take into account about adopting open surgery or minimal-invasive surgery? (Multiple choices)
- Age
- Haller index
- Symmetry of deformity
- History of thoracic surgery
- Operators’ experience and preference
- Treatment outcomes
- How to avoid heart injury during Nuss procedure? (Multiple choices)
- Usage of tunnel scope intraoperatively
- Assistance with a small sub-xiphoid incision
- Sternal elevation by means of vacuum bell, etc.
- Extrapleural bar insertion
- Open osteotomy
- Do you perform osteotomy of sternum or costal cartilage routinely?” (Multiple choices)
- Routinely performed
- Never
- In asymmetric deformity
- In severe deformity
- In adults
- Dealing with complicated or severe deformity, what skills or strategies will you undertake? (Multiple choices)
- Application of double bars or multiple bars
- Application of specific individualized bar
- Application of slanting bar
- Application of short bar
- Open surgery
- Minimal invasive surgery combined with assistance of a small subxiphoid incision
- What’s the advantage of double bar strategy? (Multiple choices)
- Better orthopedic effect
- Less pain
- Prevention of bar shifting
- Prevention of recurrence
- Avoidance of assisted incision or open surgery
- Refuse double bar strategy
- What’s the advantage of short bar strategy? (Multiple choices)
- No advantage
- Better orthopedic effect
- More stable against bar shifting
- Better cosmetic appearance
- Easier for bar removal
- When should the bar be removed after the Nuss procedure? (Multiple choices)
- Less than 2 years from surgery
- 2–3 years from surgery
- 4–5 years from surgery
- More than 5 years from surgery
- For specific cases, it depends on the real-time situations.
- Which anesthesia method do you adopt in the procedure of bar removal? (Multiple choices)
- Local anesthesia
- Epidural anesthesia
- General anesthesia + intubation
- Intravenous anesthesia + laryngeal mask
- How to avoid incision infection and bar exposure? (Multiple choices)
- Gasket insertion in one side
- No gasket
- Bar embedding beneath muscle
- Suture fixation to rib
- Application of short bar
- Application of cosmetic stitches
- Application of intradermal suture
- How to deal with bar exposure? (Multiple choices)
- Regular dressing change, and extract bar at least 2 years later
- Bar removal immediately
- Usage of vacuum suction device (VSD) drainage
- Wound debridement and suture
- Considering bar removal or not according to the severity of deformity and bar exposure situation
- What is your postoperative analgesia method for PE surgery? (Multiple choices)
- Oral
- Intramuscular or intravenous
- Intravenous pump
- Epidural pump
- Paravertebral blockage
- Peripheral nerve blockage
- When should the patients be allowed for ambulation after PE surgery? (Single choice)
- Postoperative day (POD) 1
- POD 2–3
- POD 4–5
- POD 6 or above or after discharged
- When should the patients be allowed for ambulation all by themselves after PE surgery? (Single choice)
- Within a week after surgery
- 1–2 weeks after surgery
- 2 weeks to 1 month after surgery
- 1–3 months after surgery
- More than 3 months
- When should the patients be allowed for non-competitive aerobic exercises (such as running)? (Single choice)
- Within 4 weeks after surgery
- 5–8 weeks after surgery
- 9–12 weeks after surgery
- 13 weeks and above
- After bar removal
Acknowledgements
The authors thank CATS Pectus Excavatum Management Working Group: Wei Liu, Jianhua Li, Wenliang Liu, Wenying Liu, Hongbin Duan, Jinfen Liu, Linyou Zhang, Mingwu Chen, Jianhua Zhang, Wanli Lin, Lijia Gu, Yusheng Yan, Kaican Cai and all CATS members for their cooperation in completing the survey.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics approval was not required for that this study was a result of a survey on the investigated surgeons.
References
- Obermeyer RJ, Goretsky MJ. Chest wall deformities in pediatric surgery. Surg Clin North Am 2012;92:669-84. [Crossref] [PubMed]
- Nuss D, Obermeyer RJ, Kelly RE. Nuss bar procedure: past, present and future. Ann Cardiothorac Surg 2016;5:422-33. [Crossref] [PubMed]
- Haecker FM. The vacuum bell for conservative treatment of pectus excavatum: the Basle experience. Pediatr Surg Int 2011;27:623-7. [Crossref] [PubMed]
- Al-Assiri A, Kravarusic D, Wong V, et al. Operative innovation to the "Nuss" procedure for pectus excavatum: operative and functional effects. J Pediatr Surg 2009;44:888-92. [Crossref] [PubMed]
- Varela P, Torre M. Thoracoscopic cartilage resection with partial perichondrium preservation in unilateral pectus carinatum: preliminary results. J Pediatr Surg 2011;46:263-6. [Crossref] [PubMed]
- Nuss D, Kelly RE. The Minimally Invasive Repair of Pectus Excavatum. Operative Techniques in Thoracic and Cardiovascular Surgery: A Comparative Atlas 2014;19:324-47.
- Kelly RE Jr, Cash TF, Shamberger RC, et al. Surgical Repair of Pectus Excavatum Markedly Improves Body Image and Perceived Ability for Physical Activity: Multicenter Study. Pediatrics 2008;122:1218-22. [Crossref] [PubMed]
- Grozavu C, Iliaş M, Marin D, et al. Minimally invasive repair for pectus excavatum - aesthetic and/or functional? Chirurgia (Bucur) 2013;108:70-8. [PubMed]
- Lomholt JJ, Jacobsen EB, Thastum M, et al. A prospective study on quality of life in youths after pectus excavatum correction. Ann Cardiothorac Surg 2016;5:456-65. [Crossref] [PubMed]
- Kelley SW. Surgical Diseases of Childhood. 3rd Ed. The CV Mosby Co. 1929;1:537.
- Haller JA Jr, Colombani PM, Humphries CT, et al. Chest wall constriction after too extensive and too early operations for pectus excavatum. Ann Thorac Surg 1996;61:1618-24. [Crossref] [PubMed]
- Nuss D. Minimally invasive surgical repair of pectus excavatum. Semin Pediatr Surg 2008;17:209-17. [Crossref] [PubMed]
- Frantz F. W. Indications and guidelines for pectus excavatum repair. Curr Opin Pediatr 2011;23:486-91. [Crossref] [PubMed]
- St Peter SD, Sharp SW, Ostlie DJ, et al. Use of a subxiphoid incision for pectus bar placement in the repair of pectus excavatum. J Pediatr Surg 2010;45:1361-4. [Crossref] [PubMed]
- Park HJ, Kim KS, Lee S, et al. A next-generation pectus excavatum repair technique: new devices make a difference. Ann Thorac Surg 2015;99:455-61. [Crossref] [PubMed]
- Croitoru DP, Kelly RE Jr, Goretsky MJ, et al. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg 2002;37:437-45. [Crossref] [PubMed]
- Yoon YS, Kim HK, Choi YS, et al. A modified Nuss procedure for late adolescent and adult pectus excavatum. World J Surg 2010;34:1475-80. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Du X, Mao S, Cui J, et al. Use of laryngeal mask airway for non-endotracheal intubated anesthesia for patients with pectus excavatum undergoing thoracoscopic Nuss procedure. J Thorac Dis 2016;8:2061-7. [Crossref] [PubMed]
- Patvardhan C, Martinez G. Anaesthetic considerations for pectus repair surgery. J Vis Surg 2016;2:76. [Crossref] [PubMed]
- Kolvekar S, Pilegaard H, Ashley E, et al. Pain management using patient controlled anaesthesia in adults post Nuss procedure: an analysis with respect to patient satisfaction. J Vis Surg 2016;2:37. [Crossref] [PubMed]
- Jaroszewski DE, Temkit M, Ewais MM, et al. Randomized trial of epidural vs. subcutaneous catheters for managing pain after modified Nuss in adults. J Thorac Dis 2016;8:2102-10. [Crossref] [PubMed]
- Bal-Bocheńska MA. Evaluation of the effects of rehabilitation after surgery using the Ravitch and Nuss methods: a case study. Kardiochir Torakochirurgia Pol 2016;13:72-7. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr. Minimally Invasive Surgical Correction of Chest Wall Deformities in Children (Nuss Procedure). Adv Pediatr 2008;55:395-410. [Crossref] [PubMed]
- Kelly RE, Goretsky MJ, Obermeyer R, et al. Twenty-One Years of Experience With Minimally Invasive Repair of Pectus Excavatum by the Nuss Procedure in 1215 Patients. Ann Surg 2010;252:1072-81. [Crossref] [PubMed]


