
Astym® therapy improves FOTO® outcomes for patients with musculoskeletal disorders: an observational study
Introduction
The US healthcare system continues to evolve, with current trends pointing towards a value-based system in which reimbursement rates may depend on patient outcomes. As such, obtaining and providing proof of positive outcomes is an essential element in modern day outpatient physical therapy practice. Achieving good outcomes will affect payment for services, insurance contracts, referrals, and an individual physical therapist’s employment, salary, and professional development at large. Despite the increasing importance of providing optimal outcome measures, challenges to promoting these measures do exist. For the individual clinician, these challenges include: lack of standardization of care for most musculoskeletal pathologies, a delay between discovery of evidence-based research and implementation into clinical education, and the financial cost of continuing education in accessing that evidence-based practice. For the employer, limitations include: variations in skill set and experience between physical therapist employees, and the financial cost of supplying the most up to date equipment. Given the importance of obtaining positive outcomes measures and the challenge of consistent delivery, it is important to identify evidenced based approaches that can be applied across a broad range of treatment styles and clinical settings yet allow for positive patient outcomes in the face of non-standardized treatment plans.
One such evidence-based treatment approach is Astym® therapy (Performance Dynamics, Muncie, IN, USA). Astym therapy is a non-invasive treatment designed to address soft tissue dysfunction by engaging the regenerative mechanisms of the body. This treatment was built upon evidence elucidating the degenerative nature of many tendon pathologies and has since been shown to improve tendon repair (1), improve functional ability (2,3) and normalize movement patterns (4). The positive effects of Astym therapy are, in part, due to the stimulation of healing on a cellular level. Astym therapy has been found to increase: growth factor release, fibroblast activity, macrophage mediated phagocytosis, and dysfunctional capillary exudation (3,5-7).
Astym treatment also includes functional exercises and stretches which load the tissue of interest in order to promote healthy, functional alignment of new collagen (8). Astym therapy can enhance these exercise programs, as studies have shown increased strength and flexibility immediately following this treatment (9-11).
Although this therapy utilizes hand-held instruments, it is distinctly different from tool-assisted soft tissue work, such as “Tooling”, “Scraping”, or IASTM (Instrument Assisted Soft Tissue Mobilization). These techniques typically utilize a tool to treat cross-fiber, with the goal being to mechanically “break down” what is thought to be dysfunctional tissue (11-13). The tool assisted methods are often not well-tolerated (11,14), have been shown to cause increased pain and decreased perception of function (11,14), and achieve the same results as no treatment in cases of tendinopathy (11,15). A systematic review published in 2016 evaluated the existing research on IASTM and concluded that the current research does not support the efficacy of IASTM for musculoskeletal pathologies (16).
In contrast to these techniques, Astym therapy has consistently demonstrated safety and effectiveness and is well-tolerated, across a wide patient population range (11). Astym therapy differs from other treatment techniques precisely because of its proven ability to promote cellular regeneration. Additionally, the established protocols ensure consistency of application throughout a variety of clinical settings and patient populations. While treatment application is standardized in Astym therapy, exercise prescription and other factors in the patient’s plan of care are not standardized. One of the main benefits of Astym therapy is that it can be incorporated into a wide variety of therapy styles while offering the same positive patient outcomes (9,17). Consequently, Astym therapy has the potential to improve outcomes across treatment approaches in an environment where no gold standard treatment plan exists.
The objective of this paper is to: (I) compare the effectiveness of rehabilitation utilizing Astym therapy (treatment sample) and traditional treatment without Astym (control sample); and (II) determine whether the inclusion of Astym therapy results in improved outcome scores, as compared to treatment without Astym therapy. We do this by utilizing Focus on Therapeutic Outcomes (FOTO) data to compare outcomes in a control group (receiving traditional, non-standardized physical therapy) verses a treatment group (receiving Astym therapy, in addition to non-standardized physical therapy). Outcomes data includes functional score (FS), functional score change (FSCH) utilization index (UI), and treatment visits (TV). It is our hypothesis that Astym therapy is an evidenced-based, non-invasive, and cost-effective treatment which improves outcome measures in the outpatient rehabilitation setting. If our critical review of information supports this hypothesis, it is our assertion that Astym therapy has the potential to improve patient outcomes throughout a wide variety of clinical settings.
Methods
Design
This study is a cross-sectional observational study that draws inferences about the effects of Astym treatment on patient outcomes as captured by FOTO’s Patient Inquiry® survey (18,19). The assignment of patients into a treatment or control group was outside of the control of the investigators (20).
Data collection
Data was derived from the database managed by Focus On Therapeutic Outcomes, Inc. (FOTO) Knoxville, TN, USA, an international medical rehabilitation outcomes database management company. Briefly, patients with varied orthopedic impairments were followed during their treatment in outpatient rehabilitation clinics participating with FOTO. Prior to initial evaluation and intake, patients entered demographic data and completed self-report surveys using the Computerized Adaptive Test (CAT) called Patient Inquiry®, a computer program developed by FOTO (21-24). Demographic variables consisted of age, gender, symptom acuity, surgical history, number of comorbid conditions, exercise history, and payer source. Age was collected as a continuous variable and categorized as 18–44, 45–64, and >65 years). Gender was categorized as female and male. Symptom acuity, which is operationally defined as the number of calendar days from the date of onset of the condition being treated to the date of initial therapy evaluation, was categorized as acute (<22 days), subacute (22–90 days), and chronic (>90 days). Surgical history was categorized as none, 1 or more surgeries related to the condition being treated. Number of comorbid conditions was assessed using a list of 30 conditions common to patients entering an outpatient rehabilitation clinic (25,26). Number of comorbid conditions was categorized as 0, 1–2, 3–4, and 5 or more comorbid conditions. Exercise history prior to receiving therapy was categorized as exercising 3 times a week or more, exercising 1 to 2 times a week, or exercising seldom or never. Last, 16 payer sources (e.g., Preferred Provider, Medicare) were listed for patient to select.
When clinic staff recorded patient data into the software, the staff selected “orthopedic” impairment and a specific anatomical area as the broad heading for the reason for treatment. The patient then answered condition-specific questions measuring functional status (FS) as supplied by FOTO (27). For example, patients with knee impairments were presented with questions such as: “Today, do you or would you have any difficulty at all with:” followed by activities such as “walking 2 blocks” or “performing light activities around your home”. For this example, five response categories were used: (I) extreme difficulty; (II) quite a bit of difficulty; (III) moderate difficulty; (IV) a little bit of difficulty; and (V) no difficulty. In addition, the patient could elect “Not Applicable” for any item, which was recorded as missing data and not used in FS estimation. Patients with impairments in more than one anatomical area received different sets of functional status items for each impairment.
All patients’ FS estimates ranged from 0 to 100 with higher measures representing higher functioning. Data was labeled as “intake” data when the patient completed FOTO’s CAT prior to initial evaluation whereas data was labeled “discharge” when the patient completed the CAT at the time of discharge. FS score change (FSCH) was defined by subtracting the FS score at intake from the FS score at discharge (FSCH = discharge FS − intake FS). Duration was defined as calendar days between the date of admission and date of discharge.
Setting and participants
Patients were identified as part of the treatment group if they: were 18 years old or older, were managed for their orthopedic problem(s), received outpatient physical therapy services, responded to FOTO Patient Inquiry® computer-based functional status items at admission and at discharge between September 2008 and January 2013, and if their therapists had checked the ‘Astym System’ as a procedure on the staff discharge report.
Once the treatment sample was identified, an equal sample size of control group patients was randomly selected from the aggregate FOTO data set that matched the characteristics of the patients in the treatment sample. These characteristics include: impaired anatomical area, age, gender, and symptom acuity at the group level. To ensure that the treatment and control group participants were similar, continuous characteristics (ex: age) were tested by two-sample t-tests and categorical characteristics (ex: acuity) were tested by Chi-square tests of independence. The matched selection process was replicated until there were no differences between the samples. If after 50 times of random selection process the ideal matched sample could not be achieved, the best matched sample was selected for the smallest difference in patient characteristics across groups.
Analytical procedure
We compared the results between the treatment group and control group using two approaches. First, differences between each dependent variable was tested using one-way analyses of covariance (ANCOVA) using the intake FS score as the covariate. The ANCOVA model for effectiveness data used discharge FS score as the dependent variable, treatment group as the independent variable, and intake FS score as the covariate. The ANCOVA model for efficiency data used visits and duration as dependent variables, treatment group as the independent variable, and intake FS score as the covariate. The ANCOVA model for utilization data used utilization index (unit of functional improvement per visit = FSCH divided by number of treatment visits) as the dependent variable, treatment group as the independent variable, and intake FS score as the covariate.
Second, the comparative effectiveness of Astym therapy was examined by comparing risk-adjusted discharge FS score, number of treatment visits, and treatment duration between the treatment and control sample. For meaningful interpretations of observational outcomes data where patients are not randomly selected, the dependent variables must be risk-adjusted by controlling for the effects of independent variables. There is no standard way of performing the risk-adjustment process; therefore, a general linear model was employed, where multiple independent variables were added to the model. One model was estimated for each of the four dependent variables: discharge FS score, number of treatment visits, treatment duration, and utilization index. Each model was designed to estimate the risk-adjusted dependent variables while controlling for important independent variables: age, gender, symptom acuity, surgical history, impairment category, number of comorbid conditions, and intake FS score (covariate). Age and intake FS score were entered as continuous variables while the rest of the independent variables were treated as categorical variables. Once we obtained the risk-adjusted dependent variables, three analyses of variances (ANOVAs) were used to test the main factor of the treatment group. The critical alpha level was set at 0.05.
Results
Participants
Treatment sample
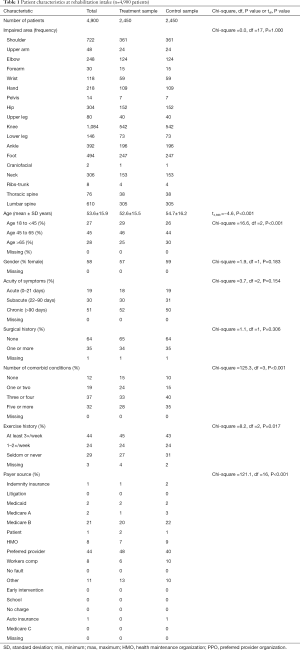
The treatment sample included data analyzed from 2,450 patients with varied orthopedic impairments receiving Astym therapy as part of their outpatient rehabilitation services in 116 cities in 17 states (Table 1). Patient mean ± SD age was 52.6±15.5 years old (min =18, max =99). Most of the patients were female (57%), had no surgical history (65%), reported their symptoms as chronic (52%), sub-acute (30%), and acute (18%). These patients averaged ± SD (13.2±8) visits over an episode duration of 47.8±31 calendar days. Identification of medical or surgical diagnoses was optional in the data collection, but of the patients with medical/surgical codes (91%), the most common diagnoses were associated with soft tissue disorders of muscle, synovium, tendon, bursa or enthesopathies (ICD-9 725–729) (27%), post-surgical conditions including discectomy and fusion (14%), and spinal pathology (ICD-9 codes 720–724) (8%), and sprains and strains including sacroiliac region, lumbar spine, sacrum (ICD-9 codes 846–848) (5%).
Full table
Control sample
The control sample included data from 2,450 patients with varied orthopedic impairments receiving outpatient rehabilitation services in 489 clinics in 34 states (U.S.). Patient mean ± SD age was 54.7±16.2 years old (min =18, max =99). Most patients were female (59%), had no surgical history (64%), reported their symptoms as chronic (50%) and sub-acute (31%) versus acute (19%). These patients averaged ± SD (12.3±7) visits over an episode duration of 47.5±30 calendar days. Of the patients with medical/surgical codes (77%), the most common diagnoses were associated with soft tissue disorders of muscle, synovium, tendon, bursa or enthesopathies (ICD-9 725–729) (20%), post-surgical conditions including discectomy and fusion (13%), and spinal pathology (ICD-9 codes 720–724) (8%), and sprains and strains including sacroiliac region, lumbar spine, sacrum (ICD-9 codes 846–848) (6%). See Table 1: intake patient characteristics of the treatment and control samples.
Compared to the control sample, patients in the treatment group tended to have higher FS intake scores (49.4 vs. 47.3, t=−5.1, df =4,989, P<0.001); be slightly younger (52.6 vs. 54.7 years, t=−4.6, df =4.898, P<0.001); report fewer comorbid conditions (Chi-square =125.3, df =3, P<0.001); exercise more often prior to rehabilitation (Chi-square =8.2, df =2, P=0.017); and self-paid for therapy services. (Chi-square =121.1, df =16, P<0.001).
At large, patients in the treatment and control groups did not differ by impaired body parts (Chi-square =0.0, df =17, P=1.000), gender (Chi-square =1.9, df =1, P=0.183), acuity (Chi-square =3.7, df =2, P=0.154), and surgical history (Chi-square =1.1, df =1, P=0.306).
Effectiveness
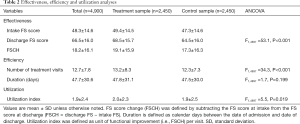
Effectiveness was defined as the final functional score (FS) upon discharge. These results are displayed in Table 2. Compared to the control sample, patients who received Astym treatment had higher discharge FS scores and the difference was significant when the intake FS scores were controlled statistically (68.5 vs. 64.5, F1,4897 =53.1, P<0.001). This shows that patients in the treatment group reported a statistically significant improvement in function as compared to patients in the control group, who did not receive Astym therapy.
Full table
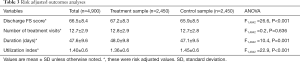
A risk adjusted outcome analysis was then performed to account for the lower initial functional scores found in the control group. These results are displayed in Table 3. The risk adjusted discharge FS score remained higher for patients in the treatment sample (67.2±8.3) compared to the control sample (65.9±8.5) (ANOVA F1,4842 =26.6, P<0.001).
Full table
Efficiency
Two separate measures were used to determine efficiency: (I) the number of visits and (II) the total time spent in outpatient physical therapy. Patients in the treatment sample received more treatment visits (13.2±8.3) (mean ± SD) compared with patients in the control sample (12.3±7.3) (ANCOVA F1,4897 =34.3, P<0.001) (Table 2). However, after risk adjustment (factoring in the lower initial FS scores for the control sample), there was no difference in the number of treatment visits (Table 3). There was no difference in duration of treatment episode across groups (Astym, 47.8±31.1 days; control, 47.5±30.0 days) (ANCOVA F1,4897 =1.7, P=0.199).
After risk adjustment, there was no difference in number of treatment visits (treatment, 12.8±2.9; control, 12.7±2.8) but slightly different duration of treatment episode across groups (Astym, 48.0±9.8 days; control, 47.1±9.5 days) (ANOVA F1,4842 =10.4, P=0.001) (Table 3).
Utilization
The utilization index (functional improvement per visit), was higher for patients in the treatment sample (Astym, 2.0±2.3; control, 1.9±2.5) (ANCOVA F1,4897 =5.5, P=0.019), suggesting that the treatment sample demonstrated more improvement for each delivered treatment. However, after risk adjustment was done to account for the lower initial FS scores of the control group, the utilization index was higher in the control sample (treatment, 1.36±0.6; control, 1.45±0.6) (ANOVA F1,4842 =22.9, P<0.001) (Table 3).
Discussion
Data from this observational study indicated that patients in the outpatient, rehabilitation setting who were treated with Astym therapy experienced increased treatment effectiveness as compared to those who did not receive Astym treatment. Astym therapy can only be provided by therapists who have completed specific training and certification. This study was conducted in clinics where Astym therapy was provided by some therapists, but not by others. The most obvious strength of this study is the size of the treatment and control group, as well as the similarity of characteristics between each group. The comparison groups in this study were large (almost 2,500 patients each) and the patients in each group were well matched. Lastly, there is a high generalizability of findings in this study as treatment was performed by many different clinicians across a wide variety of clinical settings.
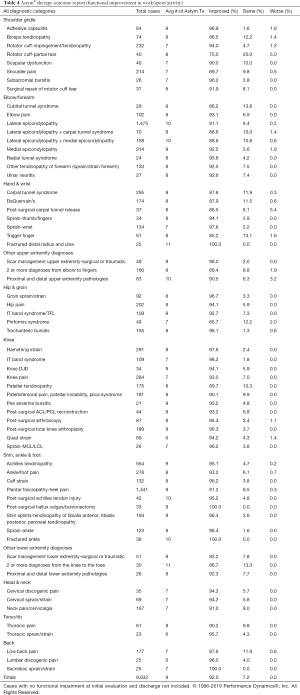
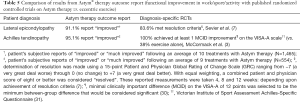
To date, there are no randomized controlled trials (RCTs) assessing the addition of Astym therapy to non-standardized rehabilitation program across a wide variety of orthopedic diagnoses. However, this study’s observational design can be used to evaluate the impact of Astym therapy in a real-world setting. In fact, it has been recommended that observational research be utilized in order to supplement RCTs as it allows for a more fitting translation of RTC findings into clinical practice (28,29). Consistent with these recommendations, outcome data on Astym therapy has been collected and analyzed on over 10,000 patients who received Astym therapy (Table 4). Astym therapy was delivered by hundreds of different clinicians, across multiple sites and in various settings (including outpatient therapy clinics, hospitals, in the military, within industry and in the workplace). The outcomes data collected is consistent with the results shown in two RCTs on Astym therapy (3,7) (Table 5). According to a recent Cochrane Review (32), there is little difference between the results obtained from quality RCTs and observational studies, indicating that both types of studies are inherently valuable. Subsequently, we can assume that conclusions drawn from observational studies are consistent with conclusions drawn from RCTs regarding the effectiveness of Astym therapy.
Full table
Full table
Realistically, this study could not have been conducted as a randomized controlled trial (RTC) design. Simply put, the ability to adequately control treatment and control samples in a double-blind situation is costly and unreasonable for this inquiry. For this same reason, observational studies comprise a growing proportion of comparative effectiveness research (CER) because of their efficiency, generalizability to clinical practice, and ability to examine differences in effectiveness across patient subgroups. Concerns about selection bias in observational studies can be mitigated by measuring potential confounders and analytic approaches, including multivariable regression, propensity score analysis, and instrumental variable analysis. RCTs are a major component of CER, however, RCTs often have restrictive enrollment criteria so that the participants do not resemble patients in practice, particularly in clinical characteristics such as comorbidity, age, medications or in sociodemographic characteristics such as race, ethnicity, and socioeconomic status. Additionally, RCTs are often not feasible, either because of expense, ethical concerns, or patient acceptance. Finally, given their expense and enrollment restrictions, RCTs are rarely able to answer questions about how an intervention’s effectiveness may vary across patients or clinical settings.
The strengths and limitations of observational studies for clinical effectiveness research have been debated for decades (19,28,29,32). Observational studies often have relatively large numbers of participants who are more representative of the general population, as the incremental cost of including an additional participant is generally low. Large, diverse study populations make the results more generalizable to real-world practice and enable the examination of variation in effect across patient subgroups. This advantage is particularly important for understanding effectiveness among vulnerable populations who are often underrepresented in RCT participants (33).
There are limitations to this study which should be discussed. First, researchers were not in control of data collection procedure as data was collected via a proprietary database management company. Similarly, the researchers were not in control of the specific timetable in which patients were to be assessed, as participating physical therapist did not receive any formal training in data collection prior to initiation of the study. However, since patients and those collecting the data were not aware of this study being conducted, both the patients and treating therapists were effectively blinded. Second, results from this study may have limited generalizability as not all outpatient physical therapy clinics utilize FOTO, and fundamental differences between clinics that utilize this outcome measure and clinics that do not may be significant. Third, it is possible that patients who seek and receive Astym therapy are inherently more educated regarding their treatment options and more health conscious at baseline. This could have resulted in an unintended selection bias of patients who are more compliant with their plan of care and more motivated to return to a higher level of function. Compared to the control sample, patients in the treatment group tended to have higher FS intake scores (49.4 vs. 47.3, t=−5.1, df =4,989, P<0.001); be slightly younger (52.6 vs. 54.7 years, t=−4.6, df =4.898, P<0.001); report fewer comorbid conditions (Chi-square =125.3, df =3, P<0.001); exercise more often prior to rehabilitation (Chi-square =8.2, df =2, P=0.017); and self-pay for therapy services (Chi-square =121.1, df =16, P<0.001). This could indicate that assignment to the treatment group represents an inherent selection bias.
The findings in this study are supported by published data and outcome reports which demonstrate the beneficial use of Astym therapy in the management of a variety of musculoskeletal disorders. These include patients with limited ROM and function of the knee and shoulder (2,34), mid-portion Achilles tendinopathy (35), patellar tendinopathy (36), high-hamstring tendinopathy (37), and chronic ankle sprain (10). In another large case series, clinicians from across the country independently entered their treatment data to create the Astym therapy outcome report shown in Table 4. This data demonstrates that Astym therapy is safe, effective and well-tolerated across a wide range of musculoskeletal disorders and patient populations. The established protocols utilized with Astym therapy assure consistency of application across a variety of therapy styles, while offering the same positive patient outcomes.
On a cellular level, Astym therapy has been shown to facilitate tendon healing by activation of fibroblasts, with fibroblast proliferation dependent upon the magnitude of the applied pressure (1,5). It is further hypothesized that Astym therapy activates a regenerative response via exudation of cellular mediators from dysfunctional capillaries, macrophage mediated phagocytosis, release of growth factors, as well as fibroblast recruitment and activation (1,5). Future studies connecting global outcomes data to healing on the cellular level could further elucidate the mechanism by which Astym therapy benefits patients seeking treatment for musculoskeletal disorders.
Conclusions
Patients with musculoskeletal disorders who received Astym therapy as part of the process experienced increased treatment effectiveness as compared to those who did not receive Astym therapy. The addition of Astym therapy improved physical therapy outcomes for patients across a broad range of treatment styles, clinical settings and therapist expertise.
In a healthcare environment with increasing emphasis on value-based models of reimbursement, the delivery of better patient outcomes is critical. Astym therapy is an evidence-based approach that has been shown to be an effective treatment that provides superior physical therapy outcomes across a wide variety of musculoskeletal disorders.
Acknowledgments
None.
Footnote
Conflicts of Interest: S Freedman, LS Harris, and YC Wang are paid consultants of Performance Dynamics Inc.
Ethical Statement: Ethics approval was not required for this study as this is an observational study, with both sets of participants receiving actual (not placebo) treatment.
References
- Davidson CJ, Ganion LR, Gehlsen GM, et al. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc 1997;29:313-9. [Crossref] [PubMed]
- Davies CC, Brockopp D, Moe K. Astym therapy improves function and range of motion following mastectomy. Breast Cancer (Dove Med Press) 2016;8:39-45. [Crossref] [PubMed]
- McCormack JR, Underwood FB, Slaven EJ, et al. Eccentric exercise versus eccentric exercise and soft tissue treatment (Astym) in the management of insertional Achilles tendinopathy: a randomized controlled trial. Sports Health 2016;8:230-7. [Crossref] [PubMed]
- Miller MM, Ray JM, Van Zant RS. The effects of Astym therapy® on a child with spastic diplegic cerebral palsy. Clin Med Insights Case Rep 2017;10:1179547617746992. [Crossref] [PubMed]
- Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc 1999;31:531-5. [Crossref] [PubMed]
- Branford OA, Brown RA, McGrouther DA, et al. Shear-aggregated fibronectin with anti-adhesive properties. J Tissue Eng Regen Med 2011;5:20-31. [Crossref] [PubMed]
- Sevier TL, Stegink-Jansen CW. Astym® treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. PeerJ 2015;3:e967. [Crossref] [PubMed]
- Virchenko O, Aspenberg P. How can one platelet injection after tendon injury lead to a stronger tendon after 4 weeks? Interplay between early regeneration and mechanical stimulation. Acta Orthop 2006;77:806-12. [Crossref] [PubMed]
- Kivlan BR, Carcia CR, Clemente FR, et al. The effect of Astym therapy of muscle strength: a blinded, randomized, clinically controlled trial. BMC Musculoskelet Disord 2015;16:325. [Crossref] [PubMed]
- Slaven EJ, Mathers J. Management of chronic ankle pain using joint mobilization and Astym® treatment: a case report. J Man Manip Ther 2011;19:108-12. [Crossref] [PubMed]
- Scheer NA, Alstat LR, Van Zant RS. Astym therapy improves bilateral hamstring flexibility and achilles tendinopathy in a child with cerebral palsy: a retrospective case report. Clin Med Insights Case Rep 2016;9:95-8. [Crossref] [PubMed]
- Daniels CJ, Morrell AP. Chiropractic management of pediatric plantar fasciitis: a case report. J Chiropr Med 2012;11:58-63. [Crossref] [PubMed]
- Solecki TJ, Herbst EM. Chiropractic management of a postoperative complete anterior cruciate ligament rupture using a multimodal approach: a case report. J Chiropr Med 2011;10:47-53. [Crossref] [PubMed]
- Vardiman JP, Siedlik J, Herda T, et al. Instrument-assisted soft tissue mobilization: effects on the properties of human plantar flexors. Int J Sports Med 2015;36:197-203. [PubMed]
- Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study. J Manipulative Physiol Ther 2011;34:123-30. [Crossref] [PubMed]
- Cheatham SW, Lee M, Cain M, et al. The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc 2016;60:200-11. [PubMed]
- Chughtai M, Newman JM, Sultan AA, et al. Astym® therapy: A Systematic Review. Ann Transl Med 2019;7:70. [Crossref] [PubMed]
- Dobrzykowski EA, Nance T. The Focus On Therapeutic Outcomes (FOTO) Outpatient Orthopedic Rehabilitation Database: results of 1994-1996. J Rehabil Outcomes Meas 1997;1:56-60.
- Swinkels IC, van den Ende CH, de Bakker D, et al. Clinical databases in physical therapy. Physiother Theory Pract 2007;23:153-67. [Crossref] [PubMed]
- Carlson MD, Morrison RS. Study design, precision, and validity in observational studies. J Palliat Med 2009;12:77-82. [Crossref] [PubMed]
- Hart DL, Wang YC, Stratford PW, et al. Computerized adaptive test for patients with knee impairments produced valid and responsive measures of function. J Clin Epidemiol 2008;61:1113-24. [Crossref] [PubMed]
- Hart DL, Wang YC, Stratford PW, et al. Computerized adaptive test for patients with foot or ankle impairments produced valid and responsive measures of function. Qual Life Res 2008;17:1081-91. [Crossref] [PubMed]
- Hart DL, Wang YC, Stratford PW, et al. A computerized adaptive test for patients with hip impairments produced valid and responsive measures of function. Arch Phys Med Rehabil 2008;89:2129-39. [Crossref] [PubMed]
- Hart DL, Werneke MW, Wang YC, et al. Computerized adaptive test for patients with lumbar spine impairments produced valid and responsive measures of function. Spine 2010;35:2157-64. [Crossref] [PubMed]
- Groll DL, To T, Bombardier C, et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 2005;58:595-602. [Crossref] [PubMed]
- Hart DL, Werneke MW, Deutscher D, et al. Effect of fear-avoidance beliefs of physical activities on a model that predicts risk-adjusted functional status outcomes in patients treated for a lumbar spine dysfunction. J Orthop Sports Phys Ther 2011;41:336-45. [Crossref] [PubMed]
- Hart DL, Wright BD. Development of an index of physical functional health status in rehabilitation. Arch Phys Med Rehabil 2002;83:655-65. [Crossref] [PubMed]
- Britton A, McPherson K, McKee M, et al. Choosing between randomized and non-randomized studies: a systematic review. Health Technol Assess 1998;2:i-iv, 1-124. [Crossref] [PubMed]
- Silverman SL. From Randomized Controlled Trials to Observational Studies. Am J Med 2009;122:114-20. [Crossref] [PubMed]
- Iversen JV, Bartels EM, Langberg H. The Victorian Institute of Sports Assessment– Achilles Questionnaire (VISA-A)—a reliable tool for measuring Achilles tendinopathy. Int J Sports Phys Ther 2012;7:76-84. [PubMed]
- Robinson JM, Cook JL, Purdam C, et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med 2001;35:335-41. [Crossref] [PubMed]
- Anglemyer A, Horvath HT, Bero L. Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev 2014.MR000034. [PubMed]
- Hart DL, Mioduski JE, Stratford PW. Simulated computerized adaptive tests for measuring functional status were efficient with good discriminant validity in patients with hip, knee, or foot/ankle impairments. J Clin Epidemiol 2005;58:629-38. [Crossref] [PubMed]
- Chughtai M, Mont MA, Cherian C, et al. A novel, nonoperative treatment demonstrates success for stiff total knee arthroplasty after failure of conventional therapy. J Knee Surg 2016;29:188-93. [Crossref] [PubMed]
- McCormack JR. The management of mid-portion Achilles tendinopathy with Astym® and eccentric exercise: a case report. Int J Sports Phys Ther 2012;7:672-7. [PubMed]
- Wilson JK, Sevier TL, Helfst RH, et al. Comparison of rehabilitation methods in the treatment of patellar tendinitis. Journal of Sports Rehabilitation 2000;9:304-14. [Crossref]
- McCormack JR. The management of bilateral high hamstring tendinopathy with Astym® treatment and eccentric exercise: a case report. J Man Manip Ther 2012;20:142-6. [Crossref] [PubMed]


