Lipoblastoma of the left kidney: a case report and review of literature
Introduction
Lipoblastoma, known as an embryonic lipoma, is a rare benign tumor that usually arises from embryonic adipose tissue in infants and children under 3 years of age (1). This tumor comprises immature embryonic adipose tissue that persists and rapidly proliferates in the postnatal period, leading to a large mass (2). Most lipoblastomas are commonly found in superficial tissues, such as in the limbs, neck and trunk, and retroperitoneal lipoblastomas are rare, occurring in fewer than 5% of cases (3,4) and rarely present in the renal pelvis. Typically, patients are asymptomatic, but lipoblastomas can lead to symptoms such as poor digestion, vomiting, and constipation, as well as backache and hematuria, if the mass is located behind the peritoneal or urinary system (5). The main treatment is complete tumor resection, and the prognosis after the operation is good. The rates of recurrence are up to 26% (6), and only one case reported spontaneous tumor regression after 8 months of follow-up (7). We experienced a rare case of an 80-year-old female with a lipoblastoma located in the left renal pelvis. This study aims to report the diagnosis, treatment and histopathology, as well as review the previously reported cases of this rare tumor.
Case presentation
The patient, an 80-year-old female, was incidentally detected to have a left renal mass using medical examinations at the People’s Hospital of China Three Gorges University (Yichang, China) in May 2018. Ultrasonography was performed on the patient and showed a left kidney mass (6.5 cm × 5 cm) located in the left renal pelvis with low blood signals. Computed tomography (CT) and CT angiography (CTA) examinations were used, and the results suggested a high possibility of a renal lipoblastoma. Routine blood, coagulation and electrolyte test results were normal. Nevertheless, the patient had no urinary-related symptoms, such as backache, hematuria and urinary tract irritation, except for a history of chronic obstructive pulmonary disease of approximately 10 years. Upon physical examination, the mass was not palpable in the patient’s abdomen, there was no abdominal tenderness, there was no percussion pain in the surface area of the kidney, and there were no clinical manifestations, such as adrenal cortical hormone increase. To confirm the diagnosis, surgical excision and pathological biopsy were necessary. After obtaining consent from the patient and her family, the surgical treatment was completed. Then, on the basis of postoperative pathology, she was admitted.
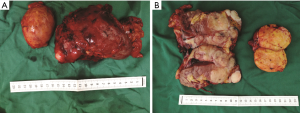
Plain CT and enhanced scanning of the patient’s upper abdomen revealed a heterogeneous mass (66 mm × 59 mm) located in the left upper renal pelvis and a solid cystic mass (84 mm × 51 mm) in the left adrenal gland (Figure 1A). The left kidney was pushed laterally by the mass with a nearly 73 mm intensified cross-section. Magnetic resonance imaging (MRI) also indicated that the left kidney was pressed by a large mass (68.7 mm × 40 mm × 60.5 mm) with an irregular short T1-weighted image signal and a slight T2-weighted image signal (Figure 1B). CTA showed that the rates of both renal blood reperfusion and renal glomerular filtration were not abnormal. Likewise, the biochemical parameters were within normal levels. Based on these examinations, the patient was presumed to be diagnosed with a left renal lipoblastoma and then underwent left radical nephrectomy by transperitoneal laparotomy. During the operation, a tough mass of approximately 5 cm × 6 cm in diameter was found to be located under the adrenal gland.

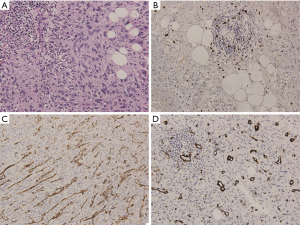
The postoperative pathological examination validated the diagnosis of lipoblastoma, indicating that the grayish yellow tumor in the left adrenal gland was tough and that the surface had a capsule (Figure 2A). Another grayish white, multinodular tumor located in the left kidney was undistinguishable from the surrounding kidney tissue; some tumors had macroscopically invaded the peripheral tissues (Figure 2B). Upon histological assessment, the specimen was composed of grapelike clusters of lobules and fat cells and separated by fibroblasts, neutrophils and leucocytes (Figure 3A). Immunohistochemical staining for the Ki67 marker was positive in the tumor cells (Figure 3B) and staining for CD31 and α-SMA were also positive in the inflammatory cells and endothelial cells of the tumors (Figure 3C,D). At the 3-month follow-up after discharge, the patient was asymptomatic and had a good recovery, as evaluated by urinary ultrasound.
Discussion
Lipoblastoma, a kind of benign mesenchymal tumor, accounts for 15% of the benign tumors that occur in children before the age of 3 (8). Most common presentations of lipoblastomas in children are rapid growth, infiltration of the surrounding structures, no pain, and location near the surface. Surgical excision with clean neoplasm margins was usually recommended for the treatment of this tumor. To the best of our knowledge, there are a few reports on lipoblastomas arising from the kidney; there are only two cases, including ours (9). Previous reports on lipoblastomas revealed that they all occurred in infants and children. There was only one case of renal lipoblastoma that occurred in a child (10). However, this case shows the occurrence of a lipoblastoma in an elderly woman with no symptoms except a simple abdominal mass who achieved good treatment outcomes after surgery.
Diagnosing a lipoblastoma is not simple due to the lack of specific clinical symptoms, and a surgical biopsy is required in adult patients. However, ultrasonography, CT and MRI are helpful in depicting the area of the mass, and CTA can also accurately evaluate the blood. In our case, this mass could be resected completely because of these examinations before the operation.
Commonly, the diagnosis of a lipoblastoma is confirmed by histopathological testing. The use of histopathology was consistent with the previous case (9), where the tumor cells of the patient were composed of polygonal nests and numerous mature adipocytes that were isolated by fibrovascular stroma. Moreover, certain immunohistochemistry markers are also helpful in discriminating lipoblastomas from other tumors. The results showed that the mass was positive for Ki67, CD31 and α-SMA, suggesting that the lipoblastoma in this case was not malignant; the results further supported the diagnosis based on the tumor histopathologic features.
Conclusions
In summary, although lipoblastomas are rare, it is imperative to distinguish its diagnosis from other large masses, especially for elderly patients. Preoperative imaging results can help diagnosis the patients due to the lack of precise examinations for lipoblastomas. A complete surgical resection is still the standard treatment for patients with lipoblastoma, and histopathologic analysis of the tumors can confirm the definitive diagnosis of a lipoblastoma. Since lipoblastomas are so infrequent in the literature, we show this case as a reminder to consider lipoblastomas in the kidneys of elderly patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Spinelli C, Costanzo S, Severi E, et al. A thoracic wall lipoblastoma in a 3-month-old infant: A case report and review of the literature. J Pediatr Hematol Oncol 2006;28:594-600. [Crossref] [PubMed]
- Jandali D, Heilingoetter A, Ghai R, et al. Large Parotid Gland Lipoblastoma in a Teenager. Front Pediatr 2018;6:50. [Crossref] [PubMed]
- Burchhardt D, Fallon SC, Lopez ME, et al. Retroperitoneal lipoblastoma: a discussion of current management. J Pediatr Surg 2012;47:e51-4. [Crossref] [PubMed]
- Schoolmeester JK, Michal M, Steiner P, et al. Lipoblastoma-like tumor of the vulva: a clinicopathologic, immunohistochemical, fluorescence in situ hybridization and genomic copy number profiling study of seven cases. Mod Pathol 2018;31:1862-8. [Crossref] [PubMed]
- Coffin CM. Lipoblastoma: an embryonal tumor of soft tissue related to organogenesis. Semin Diagn Pathol 1994;11:98-103. [PubMed]
- Sakamoto S, Hashizume N, Fukahori S, et al. A large retroperitoneal lipoblastoma: A case report and literature review. Medicine (Baltimore) 2018;97:e12711. [Crossref] [PubMed]
- Kok KY, Telisinghe PU. Lipoblastoma: clinical features, treatment, and outcome. World J Surg 2010;34:1517-22. [Crossref] [PubMed]
- Morávek J, Snajdauf J, Kodet R, et al. Lipoblastoma of kidney in a child. J Pediatr Surg 2006;41:e29-30. [Crossref] [PubMed]
- Sharma P, Shakya U, Sayami G, et al. Lipoblastoma: an unusual tumour of the left ventricle. Eur J Cardiothorac Surg 2016;49:e147-8. [Crossref] [PubMed]
- Kucera A, Snajdauf J, Vyhnánek M, et al. Lipoblastoma in children: an analysis of 5 cases. Acta Chir Belg 2008;108:580-2. [Crossref] [PubMed]