
Retrospective study of the interlaminar approach for percutaneous endoscopic lumbar discectomy with the guidance of pre-operative magnetic resonance neurography
Introduction
Percutaneous endoscopic lumbar discectomy (PELD) has evolved over the past 3 decades and has become a truly minimally invasive procedure in the treatment of intervertebral disc herniation. At present, interlaminar-PELD (IL-PELD) and transforaminal-PLED (TF-PELD) are most common in full-endoscopic procedures, and both approaches can be used to achieve sufficient decompression of the intervertebral disc. Although Yeung and Tsou (1) suggested that TF-PELD could be performed at all lumbar levels, even including at L5/S1, the approach is associated with several disadvantages. For example, it may cause injury to the exiting nerve root and intraforaminal vessels. In addition, most TESSYS techniques are required to abrade the superior articular, which might interfere with spinal stability. Therefore, it is difficult to use the transforaminal approach to manage central and paracentral herniation, which may be better treated by the interlaminar approach.
The interlaminar approach was first reported by Ruetten et al. (2) and Choi et al. (3), who suggested that this method should be performed at the L5/S1 level for the relatively larger inter-laminar windows and easier intraoperative punctures. Several studies were carried out to investigate the interlaminar approach, and the indications for this approach include L5/S1 herniation, calcified herniation, and migrating L4/5 herniation (4-8).
The development of minimally invasive techniques for the treatment of spinal lesions is inseparable from the in-depth study of the spinal anatomy, especially that of the neural structure. In recent years, with the development of advanced imaging technologies such as MRN, many scholars have begun to use MRN to study the diagnosis (9) and pre-operative evaluation (10-13) of neural structures. However, most of the studies on pre-operative evaluation were carried out on healthy volunteers. Therefore, this study is the first to report that herniation can be managed effectively under the guidance of pre-operative MRN in patients with spinal lesions. By observing the MRN and CT imaging data of the patients, we found that the origin of the lumbar nerve roots from the dural sac from S1 to L2 segments gradually decreased, and the vertical distance from the lower edge of the corresponding lamina increased. Therefore, the higher the lumbar segment was, the more likely the upper nerve root was injured. For this reason, it is necessary to evaluate the safety of the upper nerve roots during the interlaminar approach by analyzing the patients’ MRN imaging data.
In this report, 127 patients treated between June 2015 and February 2017 were retrospectively analyzed to study the value of pre-operative MRN in the procedural analysis and clinical outcome evaluation of IL-PELD, so as to demonstrate the feasibility and safety of the interlaminar approach. Under the guidance of pre-operative MRN, the application of the interlaminar approach was optimized. In the opinion of the authors, the interlaminar approach can be used for some patients suffering herniation from L2/3 to L5/S1. In addition, the indications of the interlaminar approach were confirmed in this study.
Methods
General data
Among the patients undergoing IL-PELD between June 2015 and February 2017, 127 patients with evident clinical symptoms of disc herniation and radicular symptoms were selected, all of which suffered from a single segment of unilateral intervertebral disc herniation. The patients included in the study were based on their own natural bony structures, which were with appropriate interlaminar window conditions.
Patients received at last 8 weeks of conservative treatment, but no significant pain relief was observed. In addition, there was no previous history of lumbar surgery at the same level. The exclusion criteria for the subjects of this study were as follows: (I) definite congenital anomalies, including lumbarization and spondylolysis; (II) recurrent disc herniation with adhesions at the same level; (III) severe interlaminar space narrowing, or lateral recess stenosis; (IV) extraforaminal disc herniation.
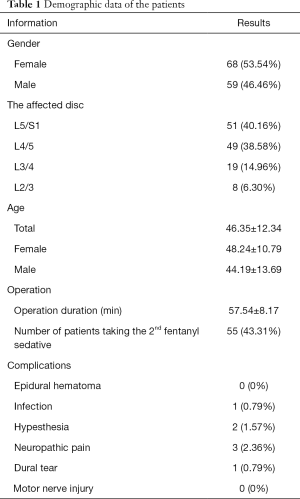
The demographic data are shown in Table 1.
Full table
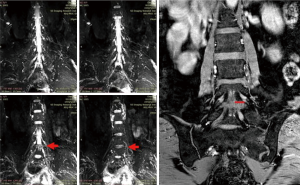
The clinical records of the patients, including pre-operative and post-operative data, were reviewed, followed by 3, 6 and 12 months of follow-up. The pre-operative data included visual analog scale (VAS) scores, the Oswestry Disability Index (ODI), the distance between the dural sac and the nerve root in the coronary scan of the ipsilateral side (distance T), and the contralateral side (distance C) of the protrusion in MRN (Figure 1). The operation data included the operation duration, the dosage of opioids received during the operation, and complications. The 3- and 12-month follow-up data included the VAS and ODI. The 6-month follow-up data included the VAS, ODI and repeated MR scans.
Outcome observations
A VAS score of 0–100 was used to compare the pre-operative and post-operative sciatic pain. The ODI (ODI, version 2.1a) was used to assess the disturbance to daily life caused by neural discomfort (14). In addition, distance T and distance C were measured and compared.
MRN scanning
All magnetic resonance (MR) imaging was performed on a clinical Siemens 3.0-T MR imager. Examinations were carried out by the same radiologist to ensure an adequate coverage of the lumbosacral plexus and the area of interest. The coronal scan, the reconstruction of the lumbosacral plexus, the traditional transverse scan, and the sagittal scan were examined before PELD. Patients were imaged in the supine position. Combined with the T2 weighted axial and sagittal images, the coronal MRN scan was performed on the target area. The posterior edge of the marker line was located at the posterior edge of the spinal canal, while the midline was located at the midpoint of the L3 vertebral body (using the L3 nerve root as an Example). The MRN coronal image scanning ranged from the upper edge of the L1 vertebral body to the lower edge of the S1 vertebral body.
Subsequently, the distance between the ganglion midpoint and the ipsilateral dural edge in the coronal plane was calculated as the distance between the nerve root and the dural sac by using the above method. The distance on the ipsilateral side with protrusion in MRN was defined as distance T, while the distance on the contralateral side (the control side) was defined as distance C (Figure 1).
Surgical procedures
The operations were carried out by a skilled surgeon using the same equipment. A 30° endoscopic surgical system (Joimax GmbH, Karlsruhe, Germany) was used. All patients were placed in a prone position with a soft cushion beneath their abdomen. Under fluoroscopic guidance, the midpoint of the affected intervertebral space was selected as the skin entry point. Local anesthesia was applied in most patients, while fentanyl was used when necessary.
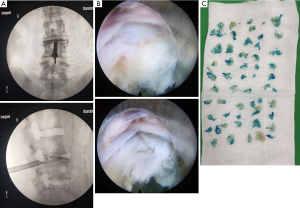
After skin infiltration by 5 mL of 1% lidocaine, a spinal needle was inserted until its tip reached the target: the lateral border of the interlaminar window of the A/P image, and the posterior vertebral line on the lateral image. Subsequently, a 1.5 mL mixture of iohexol and methylene blue (9:1) was injected to perform the discography and staining of the degenerated nucleus pulposus. Thereafter, 0.5% lidocaine was applied to the facet joint (10 mL) and the lateral recess (5 mL), followed by the creation of a 6 mm incision to sequentially insert 6 dilators. In the next step, the working canal and an endoscope were inserted to gradually dilate the ligamentum and to place the working canal into the epidural space. After the working cannula was placed, we first relieved the pressure in the field of vision, then we rotated the working canal according to the prominent position of the imaging examination. With the stepwise removal of the protruding nucleus pulposus, the space in the patient’s spinal canal for exploration was enlarged. Then the slope of the endoscope was adjusted towards the cephalic direction (Figure 2) to the rotation of the working canal to observe the axillary and exiting nerve roots, followed by the shoulder and the traversing nerve roots. If necessary, the working canal was pushed into the central zone. During this process, the protruded or sequestrated disc pieces were gently removed with a pair of disc forceps. When the pulsation of the dura was adequate and the color of the pale nerve root turned to pink, complete decompression was achieved. After hemostasis was achieved using a radiofrequency current, both the endoscope and the working canal were removed, and the cleft of the ligamentum flavum was closed before the incision was sutured. If the interlaminar space was too narrow, the laminar space was expanded with a simple burr/drill and a Kerrison punch.
Statistical methods
Data analysis was performed using SPSS Statistics 24 (SPSS Inc, Chicago, IL, USA). The data were summarized based on the mean value and range, while CI 95% and percentages were used to measure variability. The paired t-test, Mann-Whitney test, and Chi-square test were used to determine inter- and intra-group differences. Linear regression was used to test the time-trends in VAS and ODI values during follow-up. All significance tests were two-tailed, and a statistically significant level was set at a two-sided P<0.05.
Results
Demographic and operational data
In this study, 127 patients undergoing PELD via the interlaminar approach between June 2015 and February 2017 were enrolled. There were 68 females (aged 48.24±10.79 years) and 59 males (aged 44.19±13.69 years) patients. Among these patients, 51 underwent L5/S1-operation, 49 underwent L4/5-operation, 19 underwent L3/4-operation, and 8 underwent L2/3-operation (Table 1).
The mean duration of the operation was 57.54±8.17 min, and 55 patients took repeated doses of fentanyl during the operation.
The MRN image
In a coronal scan, the distance between the nerve root and dural sac was measured on the coronal plane (Table 2). The mean of distance T at L5/S1, L4/5, L3/4, and L2/3 was 14.85±0.89, 13.19±0.86, 10.30±0.72 and 8.73±0.85 mm, respectively, while the mean of distance C at these positions was 12.48±0.59, 10.52±0.72, 7.51±0.48 and 6.81±0.46 mm, respectively, indicating statistically significant differences between the two sides. The reason for such observations might be that the herniated disc pushed the nerve root laterally. The range of distance T at L5/S1, L4/5, L3/4, and L2/3 was 13.60–16.20, 11.80–14.80, 9.10–11.70 and 7.80–10.10 mm, respectively.

Full table
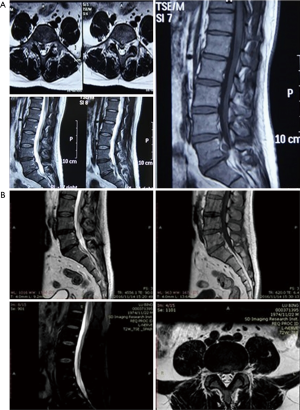
All patients underwent another MRI examination at 6 months after the operation (the results of 1 patient are shown in Figure 3). The MRI results showed no recurrence of disc herniation up to the end of the follow-up.
VAS and ODI
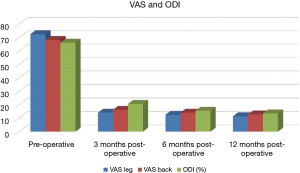
As shown in Figure 4, compared to pre-operation, there were huge reductions in VAS leg, VAS back, and ODI values at the end of 3-month follow-up (VAS leg t=50.422, P<0.001; VAS back t=60.498, P<0.001; and ODI t=32.136, P<0.001), reduced by 58.4, 52.0, and 45.6, respectively. The VAS leg, VAS back, and ODI values all showed statistically significant gradual decreasing trends from 3- to 12-month follow-up, on average, decreased by 0.8 and 1.1, 2.2 every 3 months (P≤0.022), respectively; the reductions were not so large as before.
Postoperative complications
Incomplete removal of the nucleus pulposus was not observed. In 2 patients (1.57%), mild sensory hypesthesia in the legs was detected after the operation, while 3 (2.36%) patients developed cautery-like neuropathic pain after the operation. However, the above symptoms were transient and were alleviated within 3 months. One patient (0.79%) suffered mild infection of the intervertebral space, but the infection was cured with antibiotics. One patient (0.79%) developed a slight dural tear during placement of the working catheter. No other severe complications, such a epidural hematoma, and nerve root laceration, occurred during the procedure. No patients were converted to open surgery. Furthermore, no recurrence of disc herniation and iatrogenic instability occurred by the end of follow-up.
Discussion
Despite the tremendous progress made in the field of minimally invasive surgery, there has been no great advance in the minimally invasive treatment of disc herniation since its initial invention in the early 1930s (15). Kambin and Sampson first applied the posterolateral endoscopic approach in the decompression of the percutaneous lumbar disc in the 1980s (16), which was followed by the rapid development of instruments and techniques in PELD (17-19).
The interlaminar approach of PELD has gained popularity since it was first used in the early 1980s by Forst (20) to carry out the endoscopic inspection of the intervertebral space. Ruetten et al. (2) and Choi et al. (3) showed that 94.7% of operations in the L5/S1 region were performed using the interlaminar approach to achieve a satisfactory rate of 85%. In fact, when the interlaminar approach was used to treat L5/S1 herniation, it was found that the puncture procedure became easier, the operation time became shorter, and the incidence of nerve injury was reduced. Considering some disadvantages of the transforaminal approach, including its detrimental effects on spinal stability by abrading the superior articular process, its possible damage to the exiting nerve root and intraforaminal vessels, and its difficultly in the management of central and paracentral herniation (1,21,22), this study attempted to evaluate the value of the interlaminar approach in the treatment of L4/5 herniation.
After studying the anatomy of the operation area and conducting the pre-operative coronary scan and MRN, it was proposed that the interlaminar approach could be used to treat a wider range of indications. Therefore, in addition to extraforaminal and intraforaminal herniation, the authors attempted to use the interlaminar approach in most of the patients suffering from L5/S1 herniation, and to extend the application of this approach to the upper segments, including the L4/5 and even the L3/4 and L2/3 segments, as long as the interlaminar windows were sufficiently large. In other words, the indications for the interlaminar approach were selected according to the herniated zone instead of the affected segments.
The development of minimally invasive technique for the treatment of spinal lesions is inseparable from the in-depth study of spinal anatomy, especially that of neural structures. However, the bulk of the previous research on neural structures focused on the study of cadaver specimens, and the data from live patients are hard to find. Since MRN uses diffusion techniques to suppress the signals from adjacent tissues like muscles, fats and blood vessels, it is superior to the standard MRI in neuroimaging because it highlights the neuroanatomy with a better contrast (23,24).
Despite this data, most of the studies on pre-operative MRN were carried out on healthy volunteers. Therefore, this study was the first to study MRN in patients with herniation.
Before the PELD was performed in this study, the coronal scan, the reconstruction of the lumbosacral plexus, the transverse scan, and the sagittal scan were examined carefully to locate the abnormalities in patients, such as laterally shifted nerves or swelling in the dorsal root ganglion and the distal spinal nerve (Figure 1). For some patients, the affected nerve root was either the exiting root or the traversing root. In other patients, both the exiting root and the traversing root were affected. Since sciatic pain is caused by the affected nerve root, herniations could be managed individually during the operation. Also, the distance T between the nerve root and the dural sac on the operation side was measured at the coronal plane. The mean and minimum values of distance T of L5/S1, L4/5, L3/4, and L2/3 in the MRN images were all larger than the diameter of the working canal (7.3 mm), thus suggesting the neuro-safety feasibility of the procedure. There was a significant difference between the values of distance C and T because the herniated nucleus might have pushed the dura matter away from the nerve root. As a result, the working canal could be easily placed into the ipsilateral side of the protrusion. In the process of placing the working canal, no patient complained of nerve irritation, suggesting that an adequate distance was maintained between the nerve and the protrusion for insertion of the working canal. Therefore, the interlaminar approach should not be limited to the L5/S1 level and should be used at other levels as well.
In the process of preoperative evaluation, we carefully analyzed the size of the laminar window through X-ray and CT image. If the patient’s laminar window was found to be a bit narrow, we usually used the SPINENDOS dynamic system to remove a little part of the inferior articular process or vertebral lamina, and appropriately enlarged the laminar window, which was more conducive to puncture; while the local grinding of the lamina and inferior articular process has no significant effect on the stability of the spine, even some can be self-repairing in the future. For those patients with poorly narrow vertebral windows, which were not suitable for the posterior approach, we used the intervertebral foramen approach, and these patients were not included in the scope of this article.
In addition to feasibility, the results of the IL-PELD confirmed the neurological safety of this procedure. In this study, most of the IL-PELD operations were successfully performed, and 121 patients (95.3%) showed good results. The visual analog scale and the Oswestry Disability Index were used to compare the pre-operative and post-operative sciatic pain along with the disturbance of daily life by sciatic pain. The VAS for leg and back pain decreased dramatically, while the ODI improved significantly after the operation (Figure 4). The results of this study were similar to previous reports (17,22). The overall rate of complications was significantly lower in this study. None of the patients in this study were converted to open surgery, which should be attributed to the experienced surgeon’s capable endoscopic technique, and the proper selection of patients after checking the MRN and other radiographic examinations. In addition, incomplete removal of the nucleus pulposus was not observed, nor was there any recurrence of disc herniation by the end of the last follow-up. Few patients suffered from severe post-operative nerve injuries, epidural hematomas or dural tear during the procedure. These results were also consistent with previous studies (25).
During the procedure, the approach could directly locate the reference on bony structures, thus reducing the difficulty of puncture. Coaxial expansion was adopted to establish the working channel, thus minimizing disturbance to the nerve roots and the spinal canal tissues. The treatment of the ligamentum flavum was performed by incision instead of resection, thus minimizing the destruction of the ligamentum flavum and effectively reducing the formation of epidural scar adhesion. Therefore, the procedure did not induce damage to the facet joints and did not cause any iatrogenic instability.
The anatomic target of the interlaminar approach was the disc herniation associated with the nerve roots. Methylene blue was used to stain the degenerated nuclear tissues to facilitate identification of the diseased tissues. According to the relationship between the protrusions and the accompanying nerve roots, the working channel was inserted until its tip reached the protrusion as viewed under the X-ray, thus reducing the difficulty of puncture and increasing the accuracy of puncture. In addition, the entry point was modified in this study to the mid-point of the intervertebral space (Figure 2), which made it easier for the working canal to reach the target, thus reducing the chances of dural matter laceration. Only one of the patients showed complications of cerebrospinal fluid leakage. After the initial removal of the herniation under the endoscope, the working canal was gently shifted to the opposite side so that bilateral sciatica patients could be managed. During the procedure, the bone structures of the facet were not resected because the changes to the facet could disturb post-operative bone stability.
For the ligamentum flavum, the needle was penetrated directly into the disc. After a gradual dilation, the working canal was directly placed into the epidural space. When the working canal was withdrawn along with the endoscope, the cleft of the ligamentum flavum was closed. Some reports have suggested a similar approach (3), while others have proposed an incision in the ligamentum flavum using the endoscope (2,5). For an open surgery, several reports have recommended preserving the ligamentum flavum to reduce post-operative epidural adhesion and to preserve the anatomic plane (26,27). However, the authors of this study believed that penetration instead of incision could reduce the rate of nerve injury, especially for unskilled surgeons, and hence could avoid post-operative epidural adhesion. Indeed, this study shows that choosing penetration does not significantly increase the incidence of dural tear. Li et al. (27) retrospectively studied their patients and suggested that the preservation of the ligamentum flavum could achieve better clinical outcomes and reduce the incidence of epidural fibrosis.
As long as the interlaminar window is large enough, the interlaminar approach is feasible, safe and advantageous. Therefore, this paper suggests that the indications of the interlaminar approach should be determined according to the herniated zone instead of the affected segments: if the herniation is extraforaminal only, the transforaminal approach can be used for extraforaminal herniation, while the transforaminal approach should be considered if the herniation is intraforaminal only. However, if the herniation was in the central and/or paracentral zones, the interlaminar approach should be used, regardless of whether the herniation contained the intraforaminal zone. Nevertheless, the conclusion of this study requires further verification.
Limitations
This study was not a random control study and included a shorter follow-up duration.
Conclusions
The MRN suggests that the impingement of the herniated disc increases over the distance between the nerve root and the dural sac, thus making the interlaminar approach more suitable for the treatment of the herniation as long as the interlaminar window is sufficiently large. The procedures and clinical outcomes of the PELD demonstrated the safety and other advantages of the interlaminar approach.
Acknowledgements
Funding: This research was supported by the Science and Technology Development Project of Weifang City (No. 2018YX092).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional review board of Weifang yidu Hospital at all sites prior to any subject enrollment. IRB approval was obtained for the study (No. 201548).
References
- Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722-31. [Crossref] [PubMed]
- Ruetten S, Komp M, Godolias G.. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes: prospective 2-year results of 331 patients. Minim Invasive Neurosurg 2006;49:80-7. [Crossref] [PubMed]
- Choi G, Lee SH, Raiturker PP, et al. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery 2006;58:ONS59-68; discussion ONS59-68.
- Nie H, Zeng J, Song Y, et al. Percutaneous Endoscopic Lumbar Discectomy for L5-S1 Disc Herniation via an Interlaminar Approach versus a Transforaminal Approach: A Prospective Randomized Controlled Study with 2-year Follow-up. Spine (Phila Pa 1976) 2016;41 Suppl 19:B30-7. [Crossref] [PubMed]
- Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: transforaminal versus interlaminar approach. Pain Physician 2013;16:547-56. [PubMed]
- Dabo X, Ziqiang C, Yinchuan Z, et al. The Clinical Results of Percutaneous Endoscopic Interlaminar Discectomy (IL-PELD) in the Treatment of Calcified Lumbar Disc Herniation: A Case-Control Study. Pain Physician 2016;19:69-76. [PubMed]
- Joswig H, Richter H, Haile SR, et al. Introducing Interlaminar Full-Endoscopic Lumbar Diskectomy: A Critical Analysis of Complications, Recurrence Rates, and Outcome in View of Two Spinal Surgeons' Learning Curves. J Neurol Surg A Cent Eur Neurosurg 2016;77:406-15. [Crossref] [PubMed]
- Kong W, Liao W, Ao J, et al. The Strategy and Early Clinical Outcome of Percutaneous Full-Endoscopic Interlaminar or Extraforaminal Approach for Treatment of Lumbar Disc Herniation. Biomed Res Int 2016;2016:4702946. [Crossref] [PubMed]
- Delaney H, Bencardino J, Rosenberg ZS. Magnetic resonance neurography of the pelvis and lumbosacral plexus. Neuroimaging Clin N Am 2014;24:127-50. [Crossref] [PubMed]
- Quinn JC, Fruauff K, Lebl DR, et al. Magnetic Resonance Neurography of the Lumbar Plexus at the L4-L5 Disc: Development of a Preoperative Surgical Planning Tool for Lateral Lumbar Transpsoas Interbody Fusion (LLIF). Spine (Phila Pa 1976) 2015;40:942-7. [Crossref] [PubMed]
- Guan X, Gu X, Zhang L, et al. Morphometric Analysis of the Working Zone for Posterolateral Endoscopic Lumbar Discectomy Based on Magnetic Resonance Neurography. J Spinal Disord Tech 2015;28:E78-84. [Crossref] [PubMed]
- Menezes CM, de Andrade LM, Herrero CF, et al. Diffusion-weighted magnetic resonance (DW-MR) neurography of the lumbar plexus in the preoperative planning of lateral access lumbar surgery. Eur Spine J 2015;24:817-26. [Crossref] [PubMed]
- Wang HL, Jiang JY, Lv FZ, et al. Magnetic resonance neurography in analysis of operative safety of transforaminal lumbar interbody fusion in Chinese subjects. Orthop Surg 2014;6:203-9. [Crossref] [PubMed]
- Liu H, Tao H, Luo Z. Validation of the simplified Chinese version of the Oswestry Disability Index. Spine (Phila Pa 1976) 2009;34:1211-6; discussion 1217. [Crossref] [PubMed]
- Dandy WE. Recent advances in the diagnosis and treatment of ruptured intervertebral disks. Ann Surg 1942;115:514-20. [Crossref] [PubMed]
- Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res 1986.37-43. [PubMed]
- Ahn Y, Lee SH, Park WM, et al. Posterolateral percutaneous endoscopic lumbar foraminotomy for L5-S1 foraminal or lateral exit zone stenosis. Technical note. J Neurosurg 2003;99:320-3. [PubMed]
- Kim JS, Choi G, Lee SH. Percutaneous endoscopic lumbar discectomy via contralateral approach: a technical case report. Spine (Phila Pa 1976) 2011;36:E1173-8. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 2009;10:476-85. [Crossref] [PubMed]
- Forst R, Hausmann B.. Nucleoscopy - a New examination technique. Arch Orthop Trauma Surg 1983;101:219-21. [Crossref] [PubMed]
- Choi I, Ahn JO, So WS, et al. Exiting root injury in transforaminal endoscopic discectomy: preoperative image considerations for safety. Eur Spine J 2013;22:2481-7. [Crossref] [PubMed]
- Ahn Y, Lee SH, Park WM, et al. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine (Phila Pa 1976) 2004;29:E326-32. [Crossref] [PubMed]
- Takahara T, Hendrikse JT, Mali W, et al. Diffusion-weighted MR neurography of the brachial plexus: feasibility study. Radiology 2008;249:653-60. [Crossref] [PubMed]
- Chhabra A, Andreisek G, Soldatos T, et al. MR neurography: past, present, and future. AJR Am J Roentgenol 2011;197:583-91. [Crossref]
- Markovic M, Zivkovic N, Spaic M, et al. Full-endoscopic interlaminar operations in lumbar compressive lesions surgery: prospective study of 350 patients. "Endos" study. J Neurosurg Sci 2016. [Epub ahead of print]. [PubMed]
- Askar Z, Wardlaw D, Choudhary S, et al. A ligamentum flavum-preserving approach to the lumbar spinal canal. Spine (Phila Pa 1976) 2003;28:E385-90. [Crossref] [PubMed]
- Li S, Xia H, Han C. Retrospective analysis on correlation factors of preserving the ligamentum flavum in microendoscopic discectomy. Clin Neurol Neurosurg 2015;139:46-50. [Crossref] [PubMed]


