
The application of selective neck dissection while preserving the cutaneous branches of cervical plexus in the surgical treatment of differentiated thyroid cancer—experiences from thousands of cases
Introduction
Cervical lymphadenectomy, or neck dissection, plays an important role in the management of patients with thyroid cancer (1,2). As known, the classic or radical neck dissection entails removal of some functional non-lymphatic structures routinely, including the spinal accessory nerve, the sternocleidomastoid muscle (SCM), and the internal jugular vein (IJV) (3). However, given the significant morbidity but the controversial influence of oncologic outcome while sacrificing the important structures, surgeons discreetly minimized the functional deficits based on the comparative prognosis in differentiated thyroid cancer (4,5). In 1951, Martin et al. declared that the techniques sparing the spinal accessory nerve “should be condemned unequivocally” (6). Since the lymphatic drainage of the thyroid cancer has been well demonstrated, it allows surgeons to perform more conservative neck dissections to avoid functional injury while maintaining oncologic outcome. In 1955, George Crile reported similar outcomes for patients with thyroid cancer undergoing either radical or conservative neck dissections. Thus, he further emphasized that radical procedures were unnecessary for thyroid cancer, which anatomically drain primarily to the central compartment first and only secondarily to the jugular chain (7).
Based on the knowledge of lymphatic drainage of differentiated thyroid cancer and the increasing emphasis on functional preservation, we began to develop a selective neck dissection focused on preserving the cervical sensory nerves in 1999 (8). Anatomically, the cervical plexus is a plexus of the anterior rami of the first four cervical spinal nerves which arise from C1 to C4 cervical segment. It is located in the neck, posterior to the SCM. Nerves formed from the cervical plexus innervate the back of the head, as well as some neck muscles. The cervical plexus has two types of branches, cutaneous and muscular. Muscular branches are buried in the deeper part of deep cervical fascia thus hardly to see, which could routinely be retained in the traditional modified neck dissection. We paid more attention to the four cutaneous branches including great auricular nerve, transverse cervical nerve, lesser occipital and supraclavicular nerves (9). The procedure of selective neck dissection while preserving the cutaneous branches of cervical plexus will be shown in this study.
Patient information
The patient is a 39-year-old female. She came to our hospital because she found thyroid nodule and cervical lymph nodes enlargement in medical examination 2 months ago. The patient had no radiation history or family history. Ultrasonography showed a 1.5-cm solid hypoechoic mass with dot like calcification in the right lobe [Thyroid Imaging Reporting and Data System (TI-RADS): 4C], central and lateral enlarged lymph nodes in III, IV and VI levels. CT showed a thyroid malignancy in the right lobe and cervical multiple lymph nodes enlargement in III, IV and VI levels. Fine needle aspiration (FNA) biopsy demonstrated the papillary thyroid cancer with cervical lymph nodes metastasis. The metastatic lymph nodes were all smaller than 1 cm without extra-nodal extension, and the primary tumor was unifocal and smaller than 2 cm without extrathyroidal extension. The patient was evaluated as intermediate risk and would not need radioactive iodine (RAI) therapy at the moment. Thus, the right thyroid lobectomy and unilateral selective neck dissection while preserving the cutaneous branches of cervical plexus was taken as initial treatment.
Operative techniques
The techniques of our procedure were described as below. The supraclavicular 1-cm cervical collar curved incision about 8–10 cm from the contralateral SCM margin to the affected side of the external jugular vein (EJV) is used. Flaps are elevated in the subplatysmal plane, developed from the inferior border of the mandible superiorly, to the clavicle inferiorly, and from the midline of the neck but with no extension to the posterior beyond the anterior border of the SCM, preventing backward branches of cervical plexus from injury. In developing the superior skin flap, extending may run along the lower border of mandible into capsule of submandibular gland, exposing the anterior belly of digastric muscle in the lower margin of the submandibular gland. The EJV and great auricular nerve are visualized. Lower end of the parotid gland is pull back so that the posterior belly of digastric muscle serves. The skin flap is extended along the anterior border of SCM, from posterior belly of digastric superiorly to the lower end of SCM. Care must be taken to preserve the cervical plexus when extends to the posterior midpoint of SCM, where the cervical plexus originates. The accessory nerve is covered by the superior part SCM when exposing. The dissection extends to the upper end of the posterior triangle superior to splenius capitis and levator scapulae. Then SCM is retracted, omohyoid is exposed with free dissociation as appropriate. The carotid sheath is exposed. By dissociating the IJV, carotid artery and vagus nerve, the dissection has been carried down to the prevertebral fascia overlying the deep muscle structures, starting from the superior to the inferior, the inside to the outside. Following the cervical plexus nerve, the dissection proceeds into posterior triangle with care for three main branches of supraclavicular nerve. The free dissociation of omohyoid close to the clavicle end is proceeded as appropriate, without the exposure of accessory nerve from the posterior margin of SCM to trapezius. The dissection is completed with the preservation of SCM, EJV, IJV, accessory nerve and cervical plexus, also with the radical resection of metastatic lymph nodes.
Comments
The main purpose of this study is to show the procedure of selective neck dissection while preserving the cutaneous branches of cervical plexus in DTC. In surgery from an anatomical point of view, the superior and inferior cutaneous branches could be preserved. Firstly, flaps are elevated in the subplatysmal plane, great auricular nerve runs superficially and anteriorly, therefore, it is visualized and protected. Secondly, flaps are elevated without extension to the posterior beyond the anterior border of the SCM, while the lesser occipital nerve runs deeply and posteriorly and is less likely to be injured. At last, the cautious dissection proceeds into posterior triangle avoiding the injury of three main branches of supraclavicular nerves (Figure 1). However, the transverse cervical nerve is sacrificed in the exposure of the anterior margin of sternocleidomastoid. Fortunately, the sensory deficiency could be compensated by the contralateral one.

There are two challenges in operation: one is node dissection around accessory nerve posterior beneath sternocleidomastoid, the other is exposing supraclavicular nerve in the dissection of the posterior triangle of neck. While the traditional approach runs from the outside to the inside, the inferior to the superior, which makes it be more likely to resect supraclavicular nerve. We recommend running from the superior to the inferior and the inside to the outside, which is beneficial to follow and preserve the nerves.
It is noted that the process of our dissection was artificially divided into two parts by omohyoid. Level II and III dissection are in upper area; in general, level IV and V dissection is proceeded until the muscle is retracted inferiorly, the free dissociation of omohyoid is proceeded as appropriate when the muscle is too high to pull inferiorly. In this situation, dissociate omohyoid and then pull it superiorly to make it be more appropriate for dissection.
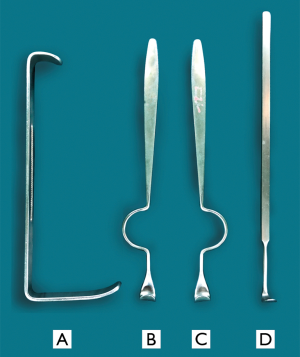
Based on the radical dissection with preservation of the cutaneous branches including the great auricular nerve, the lesser occipital nerve, the supraclavicular nerve, the complications of paresthesia and dysesthesia postoperatively in the lower neck, the shoulders and the area around the ear could be maximally decreased. Lymph node around the EJV is hardly involved in metastasis of thyroid cancer (10), thus the preservation of EJV can facilitate facial vein draining and alleviate the swelling of facial tissue. Cervical plexus, which run into the spinal root of accessory nerve, may participate in innervation of sternocleidomastoid, especially the trapezius muscles (11), so it is important to be preserved. On the other hand, the limitation of cervical sensory nerve preservation is the difficulty in the exposure of Level II and Level Va, thus it requires acquainted anatomy knowledge of neck and a great degree of expertise for the surgeon. At this point, we designed a set of retractors for elevation of the flap with better views (Figure 2). With the addition of long cutting electrotome, the dissection in area level II and Va may be improved to operated.
At last, it is necessary to emphasize that the traditional or modified neck dissection should be performed to ensure radical dissection in situations of extranodal invasion or fixed nodes. Since published literature has demonstrated the effectiveness of modified neck dissection in differentiated thyroid cancer, our approach proposes more functional preservation while the radical treatment as basic premise. In other words, all of the functional structures are preserved ultimately from surrounding tissue with en bloc resection of all affected nodes.
The optimal surgical procedure for primary DTC tumor is the topic of general interest. There may be some doubts about the surgery for the primary tumor in this case. Lobectomy and unilateral neck dissection were not being performed widely in Western countries for thyroid cancer. American Thyroid Association’s (ATA’s) guideline still recommended a near-total or total thyroidectomy for the DTC patients with clinical N1 (1). However, we could recognize the trend that the surgical procedure of primary DTC tumor turns to be less and less invasive considering the favorable prognosis of DTC. As ATA’s guideline mentioned, “we must question whether total thyroidectomy and RAI remnant ablation is required in low to intermediate risk patients.” Many researches found no difference in a comparison of thyroidectomy and lobectomy, and some studies indicated that lobectomy was done in some high-risk patients (12-14). The case shown in the video (Figure 3) was evaluated as intermediate risk and would not need RAI therapy at the moment. Thus, the right thyroid lobectomy and unilateral selective neck dissection was taken as initial treatment. The approach has been performed in more than 2,000 cases since from 1999 in Fudan University Shanghai Cancer Center. Postsurgical physical examinations were performed every 3–6 months. All patients adhered to a 12-month follow-up period, and many patients had a longer follow-up period. As reported in our previous study, the prognosis of the patients in our center is favorable with low incidence of local recurrence and distant metastasis (16). In addition, according to patient feedback, the complications of paresthesia and dysesthesia postoperatively in the lower neck, the shoulders and the area around the ear could be maximally decreased effectively. However, the quantitative evaluation of the relief of paresthesia and dysesthesia remains to be done next, which is the limitation of this study. Further studies will be conducted with large number of patients and long follow-up time.
Acknowledgements
Grateful acknowledgement is made to Long Zhang PhD who gave considerable help by means of image and video editing.
Funding: This work was supported by the funds from the National Natural Science Foundation of China (grant No. 81272934 and 81572622 to QH Ji) and the National Natural Science Foundation of China (grant No. 81702649 to N Qu).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Stack BC Jr, Ferris RL, Goldenberg D, et al. American Thyroid Association consensus review and statement regarding the anatomy, terminology, and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid 2012;22:501-8. [Crossref] [PubMed]
- Robbins KT, Medina JE, Wolfe GT, et al. Standardizing neck dissection terminology. Official report of the Academy's Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg 1991;117:601-5. [Crossref] [PubMed]
- Robbins KT, Shaha AR, Medina JE, et al. Consensus statement on the classification and terminology of neck dissection. Arch Otolaryngol Head Neck Surg 2008;134:536-8. [Crossref] [PubMed]
- Robbins KT, Clayman G, Levine PA, et al. Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg 2002;128:751-8. [Crossref] [PubMed]
- Martin H, Del Valle B, Ehrlich H, et al. Neck dissection. Cancer 1951;4:441-99. [Crossref] [PubMed]
- CRILE G Jr. SUHRER JG Jr, HAZARD JB. Results of conservative operations for malignant tumors of the thyroid. J Clin Endocrinol Metab 1955;15:1422-31. [Crossref] [PubMed]
- Thompson JC. Netter's concise orthopaedic anatomy. 2nd edition. Elsevier Health Sciences, 2009.
- Shen Q, Tian AL, Qu HO. Preservation of cervical plexus in the functional neck dissection of differentiated thyroid cancer. China Oncology 2001;(4):75-7.
- Huang X, Li L, Wen Y. Basic research on neck dissection with external jugular vein and cervical plexus preserved. Hua Xi Kou Qiang Yi Xue Za Zhi 2003;21:118-20. [PubMed]
- Kocabiyik N. Cervical Plexus. In: Tubbs RS, Shoja MM, Loukas M. editors. Bergman's Comprehensive Encyclopedia of Human Anatomic Variation. John Wiley & Sons, Inc., 2016:1062-7.
- Mendelsohn AH, Elashoff DA, Abemayor E, et al. Surgery for papillary thyroid carcinoma: is lobectomy enough? Arch Otolaryngol Head Neck Surg 2010;136:1055-61. [Crossref] [PubMed]
- Barney BM, Hitchcock YJ, Sharma P, et al. Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck 2011;33:645-9. [Crossref] [PubMed]
- Qu N, Zhang L, Ji QH, et al. Risk Factors for Central Compartment Lymph Node Metastasis in Papillary Thyroid Microcarcinoma: A Meta-Analysis. World J Surg 2015;39:2459-70. [Crossref] [PubMed]
- Qu N, Zhang TT, Wen SS, et al. Selective neck dissection with preserving cervical plexus in papillary thyroid cancer. Asvide 2019;6:113. Available online: http://www.asvide.com/article/view/31095
- Haigh PI, Urbach DR, Rotstein LE. Extent of thyroidectomy is not a major determinant of survival in low- or high-risk papillary thyroid cancer. Ann Surg Oncol 2005;12:81-9. [Crossref] [PubMed]


