Mortality after hip resurfacing versus total hip arthroplasty in young patients: a single surgeon experience
Introduction
Hip resurfacing arthroplasty (HRA) is an alternative to standard total hip arthroplasty (THA) in young, physically active patients (1). While both procedures are highly successful at relieving the pain of end-stage degenerative hip diseases, there are unique benefits to HRA in this population. It preserves their proximal femoral bone stock with better revision options if necessary in the future. It restores a more anatomic mechanical loading pattern to the hip, thereby reducing proximal stress shielding. It also reduces the risk of prosthetic dislocation and decreases the likelihood of leg length discrepancy. Very few of the currently performed hip arthroplasties are HRA’s due, in part, to concerns over the safety of the metal-on-metal bearing. While some metal-on-metal arthroplasty devices, particularly large diameter THA, demonstrated high early failure rates, certain HRA implants have shown excellent implant survivorship in carefully selected populations. Less is known about comparative mortality rates between THA and HRA.
Large longitudinal patient registries from countries with universal healthcare systems and national mortality databases have reported statistically significant reductions in patient mortality with HRA compared to THA in multivariate analyses. This stimulated our interest in reviewing our own mortality rates. Specifically, the purpose of this study was to (I) evaluate the mortality rates in patients age 55 years and younger who underwent HRA versus THA and to (II) assess whether the type of operation was independently associated with mortality.
Methods
Patient population
After institutional review board (IRB) approval, a review of the senior author’s (PJB) arthroplasty database was performed to identify patients age 55 years and younger, who underwent a primary hip arthroplasty between January 01st, 2002 and December 31st, 2010. HRA began in September 2006. This review yielded 505 patients who had undergone HRA between 2006 and 2010, with a mean age of 48 years (range, 14.0 to 55.0 years), and 124 patients who had undergone THA with a mean age of 47 (range, 18.0 to 55.0 years) (Table 1). Most of the THAs (114 of 124; 92%) were performed prior to the initiation of the HRA practice. The mean follow-up of the HRA group was 7 years (range, 1 to 11 years), and the mean follow-up of the THA group was 6 years (range, 1 to 16 years). A total of 467 of 505 (92%) patients in the HRA cohort and 105 of 124 (85%) patients in the THA cohort had more than 60-month follow-up.

Full table
Description of experiment, treatment, or surgery
All procedures performed by the senior author were done in the same hospital, with the same peri-operative care, using a transgluteal anterolateral approach. The implant utilized for HRA was the Birmingham Hip Resurfacing (Smith and Nephew, Memphis, TN, USA). The implant utilized for THA was a cementless Synergy stem, with Reflection socket, with either a ceramic on ceramic, or ceramicised metal-on cross-linked polyethylene bearing (Smith and Nephew, Memphis, TN, USA). Spinal anesthesia was used on all patients unless there was a contraindication. Pain control, mobilization, and anticoagulation protocols were standardized for all patients.
A review of the electronic medical record was performed to collect the following demographic variables: age, gender, race, body mass index (BMI), Charlson Comorbidity Index (CCI), and preoperative diagnosis. Preoperative diagnoses were divided into five major categories: primary osteoarthritis, osteonecrosis, dysplasia, slipped capital femoral epiphysis (SCFE), and other. The primary postoperative outcome was mortality. Mortality was determined through a combination of electronic chart reviews, patient phone calls, and online obituary searches. Participation was voluntary and no financial compensation was provided.
Data analysis
The characteristic distribution of the entire cohort was assessed utilizing a descriptive analysis stratified by type of surgery performed. The analysis of continuous variables was presented using means and ranges and categorical variables were presented using counts and percentages. A univariate analysis was performed to identify statistical difference between the two cohorts for each patient characteristic. Wilcoxon Sign Rank tests were performed for continuous variables and chi-square tests were used for categorical variables, unless there were not enough occurrences in the categorical groups, in which case, Fisher’s exact tests were used.
Multivariable Cox-Regression analyses were used to determine whether type of operation was independently associated with mortality. Patient demographics and preoperative characteristics that were either: (I) significantly different between the cohorts or (II) were considered clinically significant predictors of mortality were adjusted for in our multivariable logistic regression models, including: surgery type, CCI, gender, age, and diagnosis have all been implicated in mortality and were therefore included as clinically relevant co-variates in our statistical models. Only patients with a minimum of 60 months of follow-up or mortality at any time were included in the multivariate analysis. There were more smokers in the THA cohort than in the HR cohort (see Table 1). As a sensitivity analysis, the survival analyses were repeated by limiting patient selection to non-smoking patients. All analyses were carried out using SPSS 24.0 (International Business Machine Corporation, Armonk, NY, USA). All P values less than 0.05 were considered statistically significant.
Results
Mortality rates
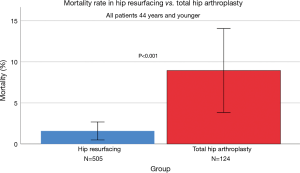
A total of 467 of 505 (92%) patients in the HRA cohort and 105 of 124 (85%) patients in the THA cohort had more than 60 months of follow-up. There were 8 mortalities (1.6%) in the HRA and 11 mortalities (8.9%) in the THA cohort (P<0.001) (Figure 1). Limiting patient selection to a primary diagnosis of osteoarthritis (Table 1) did not significantly alter the difference in mortality rates (1.9% in HRA and 6.0% in THA cohorts). When patient selection was limited to non-smokers in both cohorts, this also did not alter the difference in mortality rates (1.1% in the HRA and 12.7% in THA cohorts, P<0.001).
Multivariate analysis
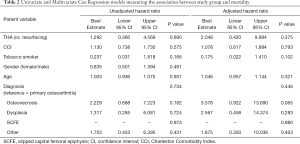
The small number of mortality events limited the statistical power. On multivariate regression analysis, we did not detect a mortality risk difference between patients who underwent THA compared to those who underwent HRA (HR 2.05; 95% CI, 0.420 to 9.994, P=0.375) (Table 2). In addition, typical mortality-related patient risk factors such as CCI, smoking, gender, age, and diagnosis were also not associated with higher risk of mortality.
Full table
When the survival analysis was repeated in non-smoking patients in both cohorts, the univariate cox regression analysis trended in favor of HRA (Beta =0.331, 95% CI, 0.075–1.467; P=0.146. In multivariate cox regression, increasing BMI was significantly associated with mortality (Beta =1.090, 95% CI, 1.028–1.156; P=0.004).
Discussion
We chose to study patients age 55 years and younger because of the primary indication for hip resurfacing being in younger patients, as well as the severe social and economic consequences of mortality in this population (2-9). We have demonstrated that patients age 55 and younger who undergo HRA have a significantly lower mortality rate than those undergoing THA (1.6% vs. 8.9%). This is consistent with previously published large database studies (2-4). Such studies analyze large heterogeneous populations of patients, surgeons, and devices. This increases the overall number of patients included to allow for multivariable analysis. Our study uniquely examined only patients age 55 or younger from a single high-volume surgeon using a single device. We achieved high rates of 5-year clinical follow-up with over 85% in each group.
In the present study, there was a significantly higher number of patients in THA cohorts that were smokers, a factor that may have potentially contributed to the higher mortality rates in these patients. However, in our sensitivity sub-analysis in which we included only non-smoking patients in both cohorts, mortality continued to be significantly higher in the THA cohort. We also re-conducted the survival analysis in this subset of patients.
There are some important limitations to the study. This is a retrospective study with the potential for selection bias. Prospective, randomized controlled studies of HRA vs. THA are difficult to conduct due to patient preferences for one procedure over the other. However, 92% of the THAs in this study were completed in the four study years prior to the availability of HRA. This ameliorates the potential concern that only healthier patients were resurfaced as evidenced by the low comorbidity burden in each group. There were a small number of mortality events and many potential contributors to mortality. This presented statistical challenges for multivariate analysis. Despite these limitations, this study represents the first single-surgeon comparison of mortality after HRA and THA.
Several other studies have also reported lower mortality rates in patients who undergo HRA compared to THA (2,4). In perhaps the most compelling report on mortality following HRA vs. THA, Kendal et al. (3) compared all-cause mortality between approximately 8,000 patients who underwent HRA, 22,000 patients who underwent cemented THA, and 24,000 patients who underwent cementless THA. Multivariate analysis considered not only age, gender, and co-morbidities, but also an Index of Multiple Deprivation that looked at social variables such as income, employment, disability, education, crime, and housing. The authors applied a Rosenbaum bounds sensitivity analysis to their data and believed that residual confounding was unlikely (3). They concluded that patients undergoing HRA had an increased odds of survival when compared to cemented [hazard ratio (HR) 0.51] and cementless (HR 0.55) THA. The Australian Joint Registry Mortality Supplement has consistently reported decreased mortality among resurfaced patients compared to those receiving THA, after age and gender adjustment, from 2014–2018 (5-9). McMinn, reviewing data from the National Joint Registry of England and Wales reported similar results (4).
On the contrary, some studies have demonstrated increased mortality in HRA when compared to THA. In a Finnish Arthroplasty Register study, the overall patient survivorship was higher in THA when compared to all HRA devices. However, when stratified by the type of implant used in this study, they showed a slightly higher survivorship with HRA when compared to THA (93% vs. 92%) (10).
Inevitably, questions arise as to the possible reasons for the reduced mortality with HRA. Some benefits of HRA over THA have been demonstrated that might conceivably affect mortality rates. Gait analysis studies of patients who underwent a HRA vs. a THA have demonstrated that HRA patients had a higher walking speed, accepted more weight at top walking speeds, pushed off with greater force, and overall had a gait more closely resemble a normal control group (11,12). Gait speed has been identified as a predictor of human longevity (13). Stride length is also related to the development of type 2 diabetes (14). Haddad et al. has demonstrated embolization of fat and/or marrow elements during THA that may be reduced or eliminated with HRA, where the recommended technique includes a suction vent during femoral component preparation and implantation (15). These could be potential reasons for the difference in the mortality rates found in this study. Alternatively, HRA patients may intangibly be more concerned with their health, maintain higher activity levels, or apt to visit health-related internet websites where they discover surgical options to which other patients are never exposed.
Conclusions
We have demonstrated that patients age 55 and under who undergo HRA have a significantly lower mortality rate than those undergoing THA. This is consistent with previously published large database studies. Such findings suggest that hip resurfacing should be considered in young, active patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: PJ Brooks is a Paid consultant of Smith & Nephew and Zimmer. D Brigati is a Board or committee member of AAOS. AS Greenwald reports the following: 4Web: Research support; AAOS: Board or committee member; Applied Medical Technologies: Research support; Arthrex, Inc.: Research support; Clinical Orthopaedics and Related Research: Editorial or governing board; Conformis: Research support; DePuy, A Johnson & Johnson Company: Research support; Journal of Arthroplasty: Editorial or governing board; Journal of Bone and Joint Surgery - American: Editorial or governing board; Lima Corporate: Research support; Materialise: Research support; Orthopaedic Research and Education Foundation: Board or committee member; Orthopedics: Editorial or governing board; Orthopedics Today: Editorial or governing board; Renovis: Research support; Seminars in Arthroplasty: Publishing royalties, financial or material support; Smith & Nephew: Paid presenter or speaker; The Bone & Joint Journal: Editorial or governing board; Total Joint Orthopedics (TJO): Research support; Waldemar Link: Research support; Zimmer Biomet: Research support. MA Mont reports the following: AAOS: Board or committee member; American Association of Hip and Knee Surgeons: Board or committee member; Cymedica: Paid consultant; DJ Orthopaedics: Paid consultant; Research support; Flexion Therapeutics: Paid consultant; Johnson & Johnson: Paid consultant; Research support; Journal of Arthroplasty: Editorial or governing board; Journal of Knee Surgery: Editorial or governing board; Knee Society: Board or committee member; Medicus Works LLC: Publishing royalties, financial or material support; Microport: IP royalties; National Institutes of Health (NIAMS & NICHD): Research support; Ongoing Care Solutions: Paid consultant; Research support; Orthopedics: Editorial or governing board; Orthosensor: Paid consultant; Research support; Pacira: Paid consultant; Peerwell: Paid consultant; Stock or stock Options; Performance Dynamics: Paid consultant; Pfizer: Paid consultant; Skye Biologics: Paid consultant; Stryker: IP royalties; Paid consultant; Research support; Surgical Techniques International: Editorial or governing board; Tissue Gene: Paid consultant; TissueGene: Research support; Up-to Date: Publishing royalties, financial or material support; USMI: Stock or stock Options; Wolters Kluwer Health - Lippincott Williams & Wilkins: Publishing royalties, financial or material support. Other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of the Cleveland Clinic.
References
- Haddad FS, Konan S, Tahmassebi J. A prospective comparative study of cementless total hip arthroplasty and hip resurfacing in patients under the age of 55 years: a ten-year follow-up. Bone Joint J 2015;97-B:617-22. [Crossref] [PubMed]
- Ellams D, Forsyth O, Mistry A, et al. 7th Annual Report. National Joint Registry for England and Wales. Healthcare Quality Improvement Partnership. 2010.
- Kendal AR, Prieto-Alhambra D, Arden NK, et al. Mortality rates at 10 years after metal-on-metal hip resurfacing compared with total hip replacement in England: retrospective cohort analysis of hospital episode statistics. BMJ 2013;347:f6549. [Crossref] [PubMed]
- McMinn DJ, Snell KI, Daniel J, et al. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ 2012;344:e3319. [Crossref] [PubMed]
- Mortality following Primary Hip and Knee Arthroplasty. Other Joints. Annual Supplementary Reports 2018.
- Mortality following Primary Hip and Knee Arthroplasty. Supplementary Reports 2017.
- Mortality following Primary Hip and Knee Arthroplasty. Analysis of State and Territory Health Data. Annual Supplementary Reports 2016.
- Mortality following Primary Hip and Knee Arthroplasty. Annual Report 2015.
- Mortality following Primary Hip and Knee Arthroplasty. Supplementary Reports 2014.
- Seppänen M, Karvonen M, Virolainen P, et al. Poor 10-year survivorship of hip resurfacing arthroplasty. Acta Orthop 2016;87:554-9. [Crossref] [PubMed]
- Mont MA, Seyler TM, Ragland PS, et al. Gait analysis of patients with resurfacing hip arthroplasty compared with hip osteoarthritis and standard total hip arthroplasty. J Arthroplasty 2007;22:100-8. [Crossref] [PubMed]
- Aqil A, Drabu R, Bergmann JH, et al. The gait of patients with one resurfacing and one replacement hip: a single blinded controlled study. Int Orthop 2013;37:795-801. [Crossref] [PubMed]
- Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA 2011;305:50-8. [Crossref] [PubMed]
- Ko SU, Stenholm S, Chia CW, et al. Gait pattern alterations in older adults associated with type 2 diabetes in the absence of peripheral neuropathy--results from the Baltimore Longitudinal Study of Aging. Gait Posture 2011;34:548-52. [Crossref] [PubMed]
- Patel R, Stygall J, Harrington J, et al. Intra-operative cerebral microembolisation during primary hybrid total hip arthroplasty compared with primary hip resurfacing. Acta Orthop Belg 2009;75:671-7. [PubMed]