
Impact of early mobilization on length of stay after primary total knee arthroplasty
Introduction
The volume of knee arthroplasties is projected to increase exponentially in the coming decades largely due to the growing aging population (1). Despite advances in post-operative care and pain management, and the proliferation of ambulatory surgical centers (ASC), most patients undergoing total knee arthroplasty (TKA) require hospitalization. The overall costs for a primary TKA, along with the projected increase in the volume of cases poses an important economic burden to the healthcare system (2,3). Increased hospital length of stay (LOS) have been correlated with increased complication rates including deep venous thrombosis, pulmonary embolism, urinary retention, and infection (4,5). Reducing LOS has been shown to improve functional recovery and a more rapid return to independent living (2,6).
There are multiple factors that dictate the LOS for a patient including hospital specific discharge requirements, patient specific factors, and patient health during the post-operative course. Some patient specific factors also play a role in LOS including patient age, body mass index (BMI), co-morbid conditions, pre-operative mental and functional status, and the patient social situation (7-11). The expectations and goals set by the care providers as well as the motivation of the individual patients also can affect length of hospitalization. Institutional factors that affect LOS include: the efficiency of the post anesthesia care unit (PACU) to transfer the patient to the orthopaedic floor, the availability of ancillary staff who are trained in the care of post-operative total joint arthroplasty care, and physical therapy (PT) resources.
Early mobilization might play a role in LOS; therefore, the purpose of this study was to determine if mobilization on the day of surgery [post-operative day 0 (POD 0)] can decrease LOS compared to mobilization on post-operative day 1 (POD 1), and whether there is a difference in discharge destination between the two groups, in patients undergoing primary TKA.
Methods
An analysis was performed on 406 consecutive primary TKAs performed at a single institution by the same surgeon with the same implant design from July 1, 2015 to June 30, 2016. After institutional review board approval, each chart was de-identified, manually reviewed, and appraised for further evaluation based on the above mentioned selection criteria. Demographic data (age, gender, and BMI), medical and surgical data [comorbidities, diagnosis leading to surgery, side of procedure, surgical approach, American Society of Anesthesiologists Score (ASA), and perioperative hemoglobin levels], PT metrics (day of mobilization, method of mobilization, distance of ambulation), and discharge data (LOS, discharge disposition) were collected. Patients mobilized on the day of surgery were categorized as POD 0 and patients who initiated PT mobilization on the day after surgery were categorized as POD 1. All patients received a pre-operative femoral and sciatic block along with total intravenous anesthesia (TIVA) and on occasion general anesthesia if the patient had a difficult airway. The institutional PT protocols, surgical techniques, and anesthesia protocols were not altered for the study and remained uniform throughout the study. A knee immobilizer was used in all cases due to the use of a femoral/sciatic block which can increase the risk of falls.
The institutional PT protocols involved getting out of bed, transferring to a chair, ambulating, and climbing stairs as patients progressed during the post-operative course. Patients were mobilized on POD 0 versus POD 1 based on the timing of the patient’s arrival to the orthopaedic floor along with the availability of the PT staff. Patients who arrived to the orthopaedic floor prior to 5 PM were mobilized on the same day of surgery. Patients who arrived after 5 PM on the day of surgery were mobilized on POD 1 due to lack of PT staff availability. Patients were discharged when medically stable and cleared by the PT staff. The therapy goals at the time of discharge included the ability to safely transfer from bed to chair, independent ambulation of at least 100 feet, and safe stair navigation. Once patients met the medical and therapy goals, they were discharged to home. Patients were discharged to a sub-acute facility if they were unable to meet their PT goals or due to social reasons if they did not have any family resources at home. Patients were not eliminated from analysis based on the reason for discharge to sub-acute facility as the vast majority of patients in both groups went to sub-acute rehab.
The two groups were compared for LOS using univariate analysis. A student’s t-test was performed for comparing LOS between POD 0 and POD 1 groups. A chi-squared test was performed to compare destination at discharge. Age, gender, ASA score, and BMI matched cases between the two groups were analyzed for the final statistical analysis. The level of significance was set at a P value of <0.05.
Out of the 406 total TKA’s reviewed, 185 patients were mobilized on POD 0 (45.6%) and 221 (54.4%) patients were mobilized on POD 1. Cases were matched based on age, gender, ASA score, and BMI, yielding a total of 143 cases in each group, or a total of 286 demographics matched patients that were used for the statistical analysis. Cases that lacked all data points, such as BMI or ASA score, were excluded. The average age for all included patients was 66.7 (range, 45–86) years. The average age for POD 0 was 66.95 (range, 49–87) years. The average age for the POD 1 group was 66.53 (range, 45–85) years. There were 106 males and 180 females with a male to female ratio of 1:1.69. The average BMI for the POD 0 group was 31.9 (range, 22–47). The average BMI for POD 1 was 32.06 (range, 20.3–47). There was no significant difference in age, sex, ASA scores, or BMI between POD 0 and POD 1 groups (P=0.696, 1.000, 0.286, 0.708 respectively) (Table 1).
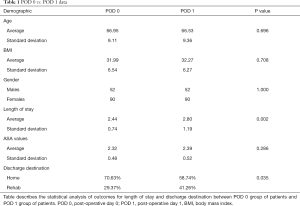
Full table
There were 142 right sided TKAs performed, 135 left sided TKAs performed and 9 bilateral TKAs performed. The mean ASA score of all patients was 2.36. The mean ASA score for POD 0 was 2.32 and 2.39 for POD 1 (Table 1). There were 101 sub-vastus and 42 parapatellar approaches for POD 0. There were 92 sub-vastus and 51 parapatellar approaches in the POD 1 group.
Results
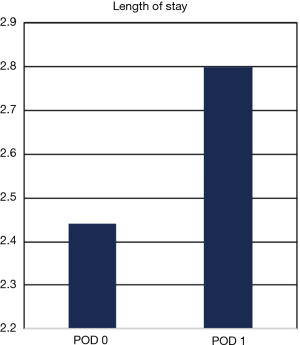
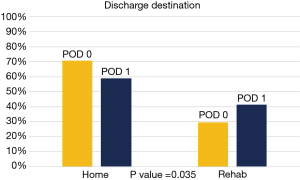
There was a significant difference in LOS between POD 0 and POD 1 groups, 2.44 vs. 2.80 days (P=0.002) (Figure 1). There was a significant difference in discharge to home versus subacute facility between POD 0 and POD 1 groups (Figure 2). There were 70.63% (n=101) discharged home in POD 0 group versus 58.74% (n=84) in POD 1 group (P=0.035). There was no significant difference between pre-op, POD 0 and POD 1 hemoglobin levels in POD 0 vs. POD 1 groups (P=0.368, 0.541, 0.793 respectively).
Discussion
Lengths of stay and discharge criteria following primary TKA can vary among institutions. There are multiple complex factors that play a role in determining the timing of discharge such as the patient’s age, overall health status, existing co-morbid conditions, and home social situation. Our institution is in a bundled payment program and had no insurance criteria restrictions on when to discharge a patient either to home or a sub-acute rehabilitation facility. While the patient’s social situation may have played a role in the discharge disposition to home versus a sub-acute facility, the LOS in large part was dependent on the patient’s ability to meet the PT discharge criteria. Given the consecutive series of 406 patients, we feel that the social issues dictating discharge to home versus subacute would be somewhat negated. Other factors that can be modified include having the patient play an active role through pre-operative education, post-operative pain management protocols, and early or immediate mobilization following surgery.
At our tertiary care hospital system, approximately 45.5% of the patients were mobilized on POD 0 following primary TKA. We believed that early mobilization would lead to reduced lengths of hospital stay and optimization of discharge status to home. Our results demonstrated a significant difference in the LOS and discharge disposition between patients who were mobilized on POD 0 versus patients who mobilized on POD 1 (P=0.002). Increased emphasis on early or rapid mobilization can help decrease the financial burden for hospital systems by reducing the overall LOS and help decrease post-operative complications. Rapid mobilization protocols concentrate on aggressive PT on the same day of surgery which has shown encouraging results with respect to functional outcome and reduced LOS.
There are several protocols across many institutions that aim to achieve the goal of reducing LOS and reduce patient complications. The specific protocols vary in detail among institutions; however, all of them involve a multidisciplinary team approach to provide rapid mobilization which has shown to improve functional outcome (12,13). The multi-disciplinary team approaches frequently involved preoperative risk stratification, specific anesthesia protocols, and use of local anesthetic injections in order to make postoperative rehabilitation easier, as well as aggressive PT protocols in hospitalized patients. Prior studies have demonstrated the use of rapid mobilization protocols in reducing the lengths of stay (14-18).
A meta-analysis of five randomized control trials by Guerra et al. found that early mobilization following hip or knee joint arthroplasty surgery has reduced LOS by 1.8 days, compared to traditional protocols (19). Most of the published studies have varied protocols including both hip and knee arthroplasty patients. Although a majority of these studies show that early mobilization reduces length of hospital stay there are a few that contradict that claim. A recent study by Karim et al. evaluated both THA and TKA length of discharge after initiation of rapid mobilization protocol on POD 0. Karim et al. showed that the LOS was not significantly shorter in the TKA or THA group (20).
An inherent weakness of the present study is its retrospective design. Several factors are uncontrolled that could also play a role on patient mobilization such as length of time spent in the PACU, availability of PT resources, level of post-operative pain control, duration of the motor nerve block which limits the patient’s ability to mobilize the quadriceps muscle, and the inherent motivation level of the patient. A strength of the study is that all procedures were performed at a single institution by a single surgeon with the same surgical technique and implant design, anesthesia, nursing and PT teams. Despite the limitations, we feel that this is useful data which demonstrates the benefits of early mobilization of patients following primary TKA with respect to decreasing LOS and discharge disposition. These results are important for providers and health care administrators involved in the care of patients undergoing TKA.
At our facility there were multiple reasons for a delay in mobilization following primary TKA including lack of PT resources, the use of motor nerve blocks, delays in transferring patients to the orthopaedic floor from the PACU following surgery due to lack of available orthopedic beds and at times the motivation level of the patient. Based on this study, our institution has increased PT resources and staffing hours to go beyond 5 PM. We have eliminated all motor blocks, and improved efficiency in the PACU to transfer patient to the orthopaedic floor in a timely manner. If the patient spends more than 2 hours in the PACU, then PT will mobilize the patient in the PACU.
This study suggests that mobilizing patients undergoing primary TKA on POD 0 decreases LOS and plays a role in discharge disposition more frequently to home versus a subacute facility. At a tertiary hospital system, aligning all the stakeholders to accomplish a task of early mobilization can be challenging. Based on hospital 2014 CFO reports, the average cost savings for a patient for a half day reduction in LOS would be on average $900 (21). Given the cost savings with decreased LOS and increased discharged to home status, it would be beneficial for hospital administrators to work with the total joint programs at their institutions including the perioperative staff, anesthesiologists, nursing and physical therapists in order to provide resources to mobilize 100% of patients on day of surgery following primary TKA.
Acknowledgements
None.
Footnote
Conflicts of Interest: MA Mont, MD—AAOS: Board or committee member. American Association of Hip and Knee Surgeons: Board or committee member. Cymedica: Paid consultant. DJ Orthopaedics: Paid consultant; Research support. Flexion Therapeutics: Paid consultant. Johnson & Johnson: Paid consultant; Research support. Journal of Arthroplasty: Editorial or governing board. Journal of Knee Surgery: Editorial or governing board. Knee Society: Board or committee member. Medicus Works LLC: Publishing royalties, financial or material support. Microport: IP royalties. National Institutes of Health (NIAMS & NICHD): Research support. Ongoing Care Solutions: Paid consultant; Research support. Orthopedics: Editorial or governing board. Orthosensor: Paid consultant; Research support. Pacira: Paid consultant. Peerwell: Paid consultant; Stock or stock Options. Performance Dynamics: Paid consultant. Pfizer: Paid consultant. Skye Biologics: Paid consultant. Stryker: IP royalties; Paid consultant; Research support. Surgical Techniques International: Editorial or governing board. Tissue Gene: Paid consultant. TissueGene: Research support. Up-to Date: Publishing royalties, financial or material support. USMI: Stock or stock Options. Wolters Kluwer Health-Lippincott Williams & Wilkins: Publishing royalties, financial or material support. AL Malkani—AAOS: Board or committee member. Journal of Arthroplasty: Editorial or governing board. Stryker: IP royalties; Paid consultant; Paid presenter or speaker; Research support. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the University of Louisville Institutional Review Board as a retrospective study with a full waiver of consent. Therefore, written informed consent was neither obtained nor required to conduct the research.
References
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Mabrey JD, Toohey JS, Armstrong DA, et al. Clinical pathway management of total knee arthroplasty. Clin Orthop Relat Res 1997.125-33. [PubMed]
- Oldmeadow LB, McBurney H, Robertson VJ. Hospital stay and discharge outcomes after knee arthroplasty: implications for physiotherapy practice. Aust J Physiother 2002;48:117-21. [Crossref] [PubMed]
- Beard DJ, Murray DW, Rees JL, et al. Accelerated recovery for unicompartmental knee replacement--a feasibility study. Knee 2002;9:221-4. [Crossref] [PubMed]
- Reilly KA, Beard DJ, Barker KL, et al. Efficacy of an accelerated recovery protocol for Oxford unicompartmental knee arthroplasty--a randomised controlled trial. Knee 2005;12:351-7. [Crossref] [PubMed]
- Pearson S, Moraw I, Maddern GJ. Clinical pathway management of total knee arthroplasty: a retrospective comparative study. Aust N Z J Surg 2000;70:351-4. [Crossref] [PubMed]
- Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: Fast-track experience in 712 patients. Acta Orthop 2008;79:168-73. [Crossref] [PubMed]
- den Hartog YM, Mathijssen NMC, Hannink G, et al. Which patient characteristics influence length of hospital stay after primary total hip arthroplasty in a “fast-track” setting? Bone Joint J 2015;97-B:19-23. [Crossref] [PubMed]
- Forrest G, Fuchs M, Gutierrez A, et al. Factors affecting length of stay and need for rehabilitation after hip and knee arthroplasty. J Arthroplasty 1998;13:186-90. [Crossref] [PubMed]
- Foote J, Panchoo K, Blair P, et al. Length of stay following primary total hip replacement. Ann R Coll Surg Engl 2009;91:500-4. [Crossref] [PubMed]
- Sharma V, Morgan PM, Cheng EY. Factors influencing early rehabilitation after THA: a systematic review. Clin Orthop Relat Res 2009;467:1400-11. [Crossref] [PubMed]
- Khan F, Ng L, Gonzalez S, et al. Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane database Syst Rev 2008.CD004957. [PubMed]
- Dowsey MM, Kilgour ML, Santamaria NM, et al. Clinical pathways in hip and knee arthroplasty: a prospective randomised controlled study. Med J Aust 1999;170:59-62. [PubMed]
- Renkawitz T, Rieder T, Handel M, et al. Comparison of two accelerated clinical pathways--after total knee replacement how fast can we really go? Clin Rehabil 2010;24:230-9. [Crossref] [PubMed]
- Husted H, Hansen HC, Holm G, et al. What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg 2010;130:263-8. [Crossref] [PubMed]
- Husted H, Otte KS, Kristensen BB, et al. Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg 2010;130:1185-91. [Crossref] [PubMed]
- Husted H, Jensen CM, Solgaard S, et al. Reduced length of stay following hip and knee arthroplasty in Denmark 2000-2009: from research to implementation. Arch Orthop Trauma Surg 2012;132:101-4. [Crossref] [PubMed]
- Tayrose G, Newman D, Slover J, et al. Rapid mobilization decreases length-of-stay in joint replacement patients. Bull Hosp Jt Dis (2013) 2013;71:222-6. [PubMed]
- Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil 2015;29:844-54. [Crossref] [PubMed]
- Karim A, Pulido L, Incavo S. Does Accelerated Physical Therapy After Elective Primary Hip and Knee Arthroplasty Facilitate Early Discharge? Am J Orthop (Belle Mead NJ) 2016;45:E337-42. [PubMed]
- Average cost per inpatient day across 50 states. Cited 2019 Jan 29. Available online: https://www.beckershospitalreview.com/finance/average-cost-per-inpatient-day-across-50-states-2016.html


