A 6-year trends analysis of infections after revision total hip arthroplasty
Introduction
Although uncommon, surgical site infections (SSIs) are severe complications following revision total hip arthroplasty (THA), and can lead to increased morbidity and mortality as well as the need for additional surgeries. Revision surgeries in particular are of concern for infection, as an extensive surgical approach can impose substantial insult to the surrounding soft tissue envelope, creating a greater inherent risk for SSIs than primary procedures. Because of the post-operative consequences of SSIs, a number of preventive infection measures have been adopted over the years, such as prophylactic antibiotic therapy, pre-operative patient optimization, operating room filtration systems, and many others (1-8). Intra-operative strategies include irrigation, intra-wound powdered antibiotics, and newer suture types and techniques. To protect the wound, different dressing types, such as negative pressure wound therapy, has been shown to significantly reduce SSI risks [relative risk 0.43, 95% confidence interval (CI): 0.32 to 0.57, P<0.0001] (9). Although a number of different SSI preventative strategies have been adopted, there is still conflicting evidence regarding THA infection trends, particularly in revision cases (10).
The current literature reports infection rates after primary THA to be between 0.2% and 0.7%. However, that number varies substantially between 0.95% and 22% for revision THAs (10,11). Phillips et al. investigated Medicare claims data for revision THA between 1995 and 1996 and found infections rates to be 1.1% (12). In more recent data from 2000 to 2011, Everhart et al. investigated risk factors for infection in 652 revision THA and found the infection incidence to be 6.2% (13). Due to these inconsistencies, the importance to track our progress in fighting infections, and the need for more up-to-date analyses, it is critical to continuously assess nationwide infection trends.
Although the current literature shows an increasing incidence of infection after revision THA, the data is varied and not current. Due to the increased mortality associated with infections after revision THA, we need to re-evaluate if our current SSI prevention strategies have slowed down the increasing trend of infection. Furthermore, although specific measures and their direct effects on infection incidences have often been investigated, the collective influence of all these efforts over an extended period of time has not been well-assessed in the literature. Therefore, the question than remains, have we been able to slow down the increasing trend of SSI rates in revision THA? To answer this, we tracked the annual rates and trends of: (I) overall; (II) deep; and (III) superficial SSIs following revision THA.
Methods
Data source
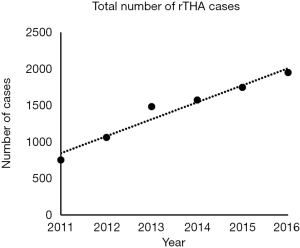
The American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) database prospectively collects data from millions from community and academic centers across the United States. Using Current Procedural Terminology (CPT) code 27134, patients who underwent revision THAs were identified from the database from January 1, 2011 to December 31, 2016. The query results in 8,562 cases, which were initially stratified according to the year of surgery. A 260% increase in the annual number of revision THA cases performed was observed from 2011 (750 cases) to 2016 (1,951 cases; Figure 1). Because the data was de-identified and publicly available, this study was deemed exempt by the Institutional Review Board.
Outcomes of interest
SSIs that occurred within 30 post-operative days for each patient were extracted from the database. SSIs were classified as either deep or superficial incisional SSIs. Deep SSIs included those with purulent drainage, or a deep incision that dehisces, or an infection found on reoperation. Superficial SSIs were identified by swelling or erythema, which required less aggressive treatment. An overall deep plus superficial SSI rate was also analyzed.
Data analyses
For each year, overall, deep, and superficial SSI incidences were calculated. Correlative analyses associating the year of surgery and infection incidence were determined with Pearson correlation coefficients. Annual infection incidences for each type of SSI were plotted against the year of surgery for trends analyses.
The infection incidence of the most recent year, 2016, was compared to the preceding 4 years utilizing univariate analysis with Pearson’s chi-squared tests. Percent differences between infection rates in 2016 and infection rates of each previous year were also calculated to evaluate rate changes. Data analyses were conducted using SPSS version 22.0 for Windows (IBM, Armonk, New York, USA) and statistical significance was maintained at a P value of less than 0.05.
Results
Overall SSI
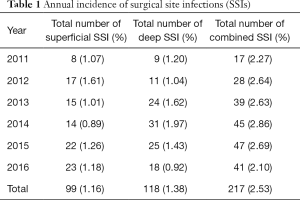
Over the 6-year study period, a total of 217 (2.53%) out of 8,562 revision THA cases were complicated by any SSI. The lowest incidence of overall SSIs was in the most recent year tabulated, 2016 (2.10%), while the highest incidence was in the earliest year, 2014 (2.86%; Table 1).
Full table
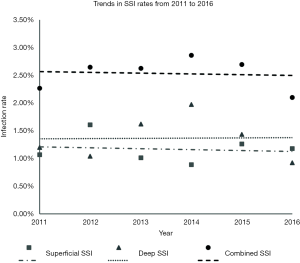
An inverse correlation between combined SSI rate and year was noted, however, this was not found to be statistically significant (P>0.05) (Figure 2).
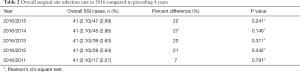
The combined SSI rate in 2016 decreased by 22% when compared to 2015 (2.10% vs. 2.69%, P>0.05). A larger, 27% decrease in rate was found between 2016 and 2014 (2.10% vs. 2.86%, P>0.05) (Table 2).
Full table
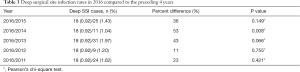
Deep SSIs
For deep SSIs, the incidence over 5 years was 1.38% (118 out of 8,562 cases). There was an inverse correlation between rate and year of surgery, however, this was not found to be significant (P>0.05; Figure 2).
There was a 35% decrease in deep SSI rate from 2015 to 2016 (1.43% vs. 0.92%, P>0.05). A larger, 53% decrease was seen between 2016 and 2014 (0.92% vs. 1.04%, P<0.01) (Table 3).
Full table
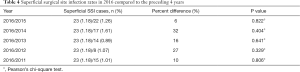
Superficial SSIs
In this 6-year period, 99 cases out of 8,562 were complicated by a superficial SSI; an incidence of 1.16%. The lowest superficial SSI incidence occurred in 2014 (n=14, 0.89%), while 2012 had the highest incidence (n=17, 1.61%) (Table 1).
There was an inverse correlation between rate and year, however, this was not statistically significant (P>0.05).
The rate in 2016 decreased by 6% when compared to 2015 (1.18% vs. 1.26%, P>0.05). A larger, 27% decrease in rate was observed between 2016 and 2012 (1.18% vs. 1.07%, P>0.05) (Table 4).
Full table
Discussion
Poor functional outcomes and increased rates of mortality after infection for total joint arthroplasty have led to a wide range of infection prevention measures which have now been the new standard over the past several years. Despite the fact that revision arthroplasty surgery is a risk within itself for SSI, there is limited literature evaluating the annual rates of infections after these procedures. Therefore, a newer, up-to-date analysis was needed to assess infection trends. The results from this study identified a decreasing trend both superficial and deep SSIs after revision THAs. For deep SSIs in particular, a significant, 53%, decrease (0.92% versus 1.04%, P<0.01) was noted from 2014 to 2016.
There are some limitations to this study. Because the data evaluated was collected from a number of different centers throughout the country, it was not possible to ensure the same infection classifications and criteria were used at each site. Nevertheless, because infections are relatively rare post-operative complications, it is necessary to use a large database such as NSQIP. Furthermore, although there is potential for data collection heterogeneity, because the data was collected from a large sampling of hospitals, it provides greater, nationwide generalizability than institution or region specific data. Additionally, the data analyzed included up to 30 post-operative day, so there is a potential for missed infections that occurred outside of this window. Nevertheless, to the best of the author’s knowledge, this study provides the most up-to-date trends analyses in infections after revision THA.
Some of the current evidence supports the decreasing trend of infection after revision THA. Pugely et al. reviewed 1,036 revision THAs in the years prior to our study, 2005 to 2010, using the same NSQIP database. They found a higher incidence of SSI, 2.9% and 1.7% for both overall and deep respectively (5). Additionally, Rasouli et al. evaluated SSIs using a Nationwide Inpatient sample database from 2002 to 2010 and found that over this time period, logistic regression showed that SSI rates declined with year. Furthermore, the authors of that study also evaluated infection trends in primary THA, and also found decreasing rates of overall, deep and, superficial infections.
In contrast to our study, Wolf et al. found increasing rates of complications following revision THA. In 337,874 revision THAs investigated between 1991 and 2008 using the United States Medicare Beneficiaries database, the group discovered a >20% increase in the readmission rate after revision THA. Over this time period, there was a steady increase in infection rates of 1.1%, 1.3%, 1.6%, 1.8%, 2.1%, and 2.9% respectively (P<0.0001) (14).
Some studies have identified important risk factors that could increase the rate of infection after revision THA. Kosashvili et al. reviewed 749 revision THAs at a mean follow up of 13.2±5.9 years, and found that infection occurred in 2.14% of these revisions. Interestingly, there was a direct and significant correlation between the number of revision THAs and the incidences of infection. Compared to a single revision surgery, infection rates increased by 42%, 84% and 480.7% after a 2nd 3rd and 4th or greater operation (15).
Conclusions
Revision total hip arthroplasties exhibited a trend, although without statistical significance, of decreasing overall SSIs nationwide between 2011 and 2016. Deep SSI rates specifically had marked improvement between 2014 and 2016. This trend indicates some benefit from pre- and post-operative infection prevention strategies, but importantly indicates continued need for improvement. Due to the potentially devastating complications associated with infection in revision THAs, further research is necessary to identify revision-specific strategies to lower the rates of SSIs.
Acknowledgements
None.
Footnote
Conflicts of Interest: SM Kurtz: Celanese, Ceramtec, Elsevier, Ferring Pharmaceuticals, Exponent, Invibio, Simplify Medical, Stelkast, Kyocera Medical, Wright Medical Technology, Lima Corporate, Stryker, Zimmer; CA Higuera: 3M, American Association of Hip and Knee Surgeons, American Journal of Orthopedics, CD Diagnostics, Cempra, Cymedica, Journal of Hip Surgery, Journal of Knee Surgery, KCI, Mid-American Orthopaedic Association, Musculoskeletal Infection Society, Myoscience, National Quality Forum, OREF, Orthofix, Inc., Pacira, Stryker, TenNor Therapeutics Limited, The Academy of Medicine of Cleveland & Northern Ohio (AMCNO), Zimmer; MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc, Sage, Stryker: IP royalties, Surgical Technologies International, Kolon TissueGene. The other authors have no conflicts of interest to declare.
Ethical Statement: This study was deemed exempt by the Institutional Review Board.
References
- Prokuski L, Clyburn TA, Evans RP, et al. Prophylactic antibiotics in orthopaedic surgery. Instr Course Lect 2011;60:545-55. [PubMed]
- van Kasteren MEE, Manniën J, Ott A, et al. Antibiotic prophylaxis and the risk of surgical site infections following total hip arthroplasty: timely administration is the most important factor. Clin Infect Dis 2007;44:921-7. [Crossref] [PubMed]
- Ponce B, Raines BT, Reed RD, et al. Surgical Site Infection After Arthroplasty: Comparative Effectiveness of Prophylactic Antibiotics: Do Surgical Care Improvement Project Guidelines Need to Be Updated? J Bone Joint Surg Am 2014;96:970-7. [Crossref] [PubMed]
- Mistry JB, Naqvi A, Chughtai M, et al. Decreasing the Incidence of Surgical-Site Infections After Total Joint Arthroplasty. Am J Orthop (Belle Mead NJ) 2017;46:E374-87. [PubMed]
- Pugely AJ, Martin CT, Gao Y, et al. The Incidence of and Risk Factors for 30-Day Surgical Site Infections Following Primary and Revision Total Joint Arthroplasty. J Arthroplasty 2015;30:47-50. [Crossref] [PubMed]
- Sørensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg 2012;147:373-83. [Crossref] [PubMed]
- Del Savio GC, Zelicof SB, Wexler LM, et al. Preoperative nutritional status and outcome of elective total hip replacement. Clin Orthop Relat Res 1996.153-61. [Crossref] [PubMed]
- Chauveaux D. Preventing surgical-site infections: measures other than antibiotics. Orthop Traumatol Surg Res OTSR 2015;101:S77-83. [Crossref] [PubMed]
- Strugala V, Martin R. Meta-Analysis of Comparative Trials Evaluating a Prophylactic Single-Use Negative Pressure Wound Therapy System for the Prevention of Surgical Site Complications. Surg Infect (Larchmt) 2017;18:810-9. [Crossref] [PubMed]
- Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am 2003;85-A:27-32. [Crossref] [PubMed]
- Zhan C, Kaczmarek R, Loyo-Berrios N, et al. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am 2007;89:526-33. [Crossref] [PubMed]
- Phillips CB, Barrett JA, Losina E, et al. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am 2003;85-A:20-6. [Crossref] [PubMed]
- Everhart JS, Andridge RR, Scharschmidt TJ, et al. Development and Validation of a Preoperative Surgical Site Infection Risk Score for Primary or Revision Knee and Hip Arthroplasty. J Bone Joint Surg Am 2016;98:1522-32. [Crossref] [PubMed]
- Wolf BR, Lu X, Li Y, et al. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am 2012;94:e103. [Crossref] [PubMed]
- Kosashvili Y, Backstein D, Safir O, et al. Dislocation and infection after revision total hip arthroplasty: comparison between the first and multiply revised total hip arthroplasty. J Arthroplasty 2011;26:1170-5. [Crossref] [PubMed]