
Preoperative thromboprophylactic administration of low-molecular-weight-heparin significantly decreased the risk of intraoperative bleeding compared with heparin in patients undergoing video-assisted lobectomy for lung cancer
Introduction
Venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary embolism (PE) usually caused high morbidity and mortality which was associated with surgeries, especially for cancers (1). It was known that risk factors of VTE including elderly age, female sex, obesity, bed-rest, venous catheterization, radiotherapy and infections (2,3). Besides, malignancies and surgeries also were regarded as pivotal and well-recognizes risks factor for VTE (4-6). Lung cancer is the most common type cancer worldwide, which is estimated about 1.6 million new cases per year and 1.38 million deaths, it consists of 12.7% of new cancer diagnosis and 18.2% of all cancer related deaths (7). Currently, surgical resection is regarded as standard therapy for resectable lung cancer. However, cancer patients were reported to be about 5- to 7-fold higher risk of VTE compared with normal population (8), the incidence increased to 22 times for lung cancer patients and the incidence of VTE of lung cancer patients was 7 times higher compared with other cancers (9). What’s more, cancer patients undergoing major thoracic surgery were always related to high risk of thromboembolism, who were found to be more than threefold of risk of fatal PE than non-cancer patients undergoing similar thoracic surgery (10). The 1-year incidence of lung cancer patients suffered VTE were estimated to be 5–6% without administrating thromboprophylactic therapies (11). Therefore, there was no doubt that lung cancer patients were at a high risk of VTE, especially during and after-surgery (5,12).
American College of Chest Physicians Evidence-Based Clinical Practice Guidelines recommended either sodium heparin or low-molecular-weight-heparin (LMWH) for those patients at a high risk of vein thrombosis (13). However, the rational timing and precise dosage of the anti-coagulant agents were still lacking a consensus. Due to considering the risk of heparin related bleeding events, most thoracic surgeons chose to administrate anti-coagulant agents after surgery (2). Whereas, it was found the incidence of VTE was still existing from clinical practice, resulting in severe complications even death, which may be formed during or even before surgery, thoracic surgeons started to administrate anti-coagulants heparin sodium preoperatively to avoid VTE in most degree according to the need of actual clinical circumstance, the studies found there were no significant difference of coagulation function and bleeding volume between preoperative and postoperative administration of heparin (14,15). On basis of these outcomes and guidelines recommendation, we continued to further use LMWH preoperatively for providing lung cancer patients intended to receive video-assisted lobectomy with sufficient thromboprophylaxis. However, excessive intraoperative bleeding volume could indeed significantly affect vision of surgery field, making anatomical accuracy weakened and unexpected surgical injury to adjacent tissue, especially for video-assisted thoracoscopic surgery (VATS). On the condition of providing sufficient thromboprophylaxis, the more intraoperative bleeding volume decreased, the more clear view of surgery field would create in VATS. The question appeared that how to choose the correct anti-coagulant agent to create a more clear operative field. Thus, the aim of this study was to compare the bleeding risk and the influence of coagulation function of preoperative administration of heparin sodium and LMWH in patients undergoing VATS lobectomy for primary lung cancer.
Methods
The data of these patients who were diagnosed with lung cancer pathologically and conducted video-assisted major thoracic surgery lobectomy by one single surgical team (directed by Dr. Lin) under general anesthesia from August 2016 to January 2018 in our department were collected retrospectively. All the patients were from two groups: preoperative administration of heparin group (PH group) who had received heparin 5,000 IU, BID, both pre- and post-operatively. And the preoperative LMWH group (PL group) who had received LMWH 4,000 IU, QD, both pre- and post-operatively. BID means twice a day, while QD means once a day. All the patients were from a prospective study, patients admitted to our department to receive video-assisted major thoracic surgery lobectomy would be divided into two groups randomly, and one group received heparin or LMWH from admission to hospital until discharge, while another group patients accepted heparin or LMWH postoperatively until discharge. All the patients did not stop receiving the agents on admitted to our department until discharged unless the drainage volume exceeded 500 mL per 24 hours, if the postoperative drainage volume exceeded 500 mL per day, heparin sodium would be temporally ceased and restarted when the drainage volume was less than 500 mL per day in both group. The patients would accept blood transfusion: (I) acute large bleeding with unstable vital sign; (II) hemoglobin less than 70 g/L. The inclusion criteria were: (I) 18–75 years old without any preoperative VTEs; (II) patients diagnosed with primary lung cancer without metastasis; (III) patients received video-assisted major thoracic surgery lobectomy. The exclusion criteria included: (I) patients receiving any other therapeutic anticoagulation; (II) patients undergoing converted open thoracic surgery; (III) patients with severe renal or liver dysfunction; (IV) patients without complete data for analysis; (V) patient suffered from major bleeding more than 500 mL owing to major angiorrhexis of lung. Our study was approved by the Ethics Committee of West China Hospital, Sichuan University (approval number: 20160601). Since our study was a retrospective analysis and analyzed anonymously, the ethics committee waived the need for consent. The indications for removing of chest tube was the chest tube drainage volume was less than 250 mL/day, without air leak, and it was the same for all the patients.
All those patients were again routinely screened for VTEs rightly after remove of chest tube. The following data were collected for analysis: demographic data (including age, weight and gender), preoperative and postoperative duration of anti-coagulants, operation time, bleeding volume, drainage duration, mean drainage volume, pre- and post-operative coagulation parameters [including international normalized ratio (INR), activated partial thromboplastin time (APTT), prothrombin time (PT), fibrinogen (FIB), thrombin time (TT)], hematologic data [platelet count (PLT), hemoglobin value (HGB)]. The coagulation parameters and hematologic data were first examined on admission to our department, the second time to extract blood to do the examination was the first day after surgery.
Statistical analysis
All the data were presented by mean value ± standard deviation for continuous variables or number (%) for categorical data. Statistical analysis was conducted with SPSS 22.0 software (SPSS Corp., Chicago, IL, USA). For continuous variables, Student’s t-test or the Mann-Whitney non-parametric U-test was applied; as for categorical data, the Chi-square or Fisher’s exact test was used. A P value of <0.05 (two-sided) was considered to be statistically significant.
Results
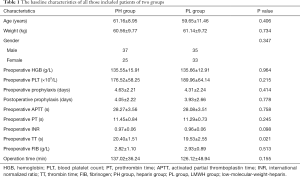
A total of 137 patients who undergone VATS lobectomy were eligible for this study, 67 patients were collected for preoperative administration of heparin group (PH group) while 70 patients belongs to LMWH group (PL group). Five patients of PH and 1 patient of PL group were excluded because of arteriorrhexis of lung, which was resulting from the process of dissecting the tumor-invaded artery or severe pleural adhesion. Besides, 1 patient of PL group was converted to open thoracic surgery owing to severe pleural cavity adhesion. Therefore, a total of 62 and 68 patients who were divided into PH and PL, respectively, were completely analyzed. The baseline characteristics including demographic data, preoperative hematologic data, pre- and post-operative duration of anti-coagulants were comparable between the two groups as showed in Table 1. Besides, Table 1 demonstrated there was no significant differences on operation time and preoperative coagulation parameters between PH group and PL group, except preoperative comparison of TT value (20.40±1.51 and 19.52±2.55, respectively; P=0.021), which could thought be the result of relatively small sample size.
Full table
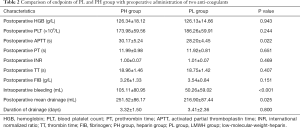
The endpoints including postoperative coagulation parameters, postoperative hematologic data, intraoperative bleeding volume, mean drainage volume and duration of drainage were demonstrated in Table 2. Postoperative PLT count [(173.98±59.56)×109/L and (186.26±59.91)×109/L, respectively; P=0.244], HGB value (126.34±18.12 and 126.13±14.66 g/L, respectively; P=0.943) were similar between PH and PL group. What’s more, there were no significant differences on PT (11.99±0.98 and 11.92±0.81 s, respectively; P=0.651), INR (1.00±0.07 and 1.01±0.07, respectively; P=0.469), TT (18.96±1.46 and 18.75±1.42 s, respectively; P=0.407), and FIB (3.26±1.33 and 3.54±0.84 g/L, respectively; P=0.151) for PH and PL group. However, the postoperative APTT value (30.17±5.24 and 28.20±4.45 s, respectively; P=0.022) of PH group was significantly longer than PL group. Compared with PL group, the study revealed that intraoperative bleeding volume (105.11±80.95 and 50.26±59.02 mL, respectively; P<0.001) of PH group was significant more.
Full table
No major bleeding related events occurred in PH group, while one 61-year-old male patient of this group suffered from mild PE at postoperative day 2, who diagnosed with lung cancer and hyperlipidemia. The major symptom was transient syncope, and the following computed tomography pulmonary angiography confirmed small embolisms in the pulmonary artery. Then with administration of continuous heparin plus warfarin, the patient recovered quickly. And the risk factors including age (61 years old), comorbidity (diagnosed hyperlipidemia), and the major thoracic surgery (video-assisted major thoracic surgery lobectomy) caused the complication. The symptom was not severe, the reason was possibly preoperative administration of anti-coagulants. As for PL group, no patients suffered VTE, but there was a 62-year-old female patient diagnosed with lung adenocarcinoma of left upper lobe, encountered second surgery owing to bleeding in pleural cavity at postoperative day 3. We did hemostasis and cleared out about 1,800 mL blood in the left pleural cavity intraoperatively, with VATS. Owing to the major bleeding volume, the patient received transfusion of 3.5 U red cell suspension intraoperatively. Then the patient recovered successfully and discharged at postoperative day 10. The result of this study indeed was administration of LMWH resulted in a lower intraoperative bleeding volume. However, the re-operative patient was from the PL group. It is heterogeneous, the reason may be that the patient suffered bleeding postoperatively possibly was being a no hypercoagulable state, and the bleeding event occurred after the continuous duration of anti-coagulant. Or maybe some intraoperative bleeding sites was re-bleeding owing to fluctuation of blood pressure. But it did not influence that we reach the conclusion of the total study.
Discussion
At present, many studies have investigated the influence of postoperative administration of unfractionated heparin or LMWH on coagulation profile, aiming to study efficacy and safety of postoperative administration of anticoagulants for the patients receiving thoracic cancer surgery, however, a worldwide consensus was still not reached (2,16-19). The proper timing and dosage of administration of anti-coagulants was still unknown. What was only prevalently accepted by thoracic surgeons was that thoracic cancer patients who undergone major thoracic surgery were at a high risk of DVT, while the patients were always accompanied with many thromboembolism risk factors, such as older, immobilization, chemotherapy, radiotherapy, and so on (6). We conducted the study preoperative administration of different anti-coagulants for lung cancer patients who undergone VATS lobectomy, demonstrating that preoperative use of LMWH decreased bleeding related risk and effect coagulation profile less with sufficient thromboprophylaxis. Intraoperative bleeding volume and postoperative mean drainage volume of PH group were both significantly more than PL group and APTT value of PH group was longer obviously. It was a little interesting about comparison of preoperative TT, the statistical significantly difference could result from the relatively small sample size. However, the fact was that the mean value of TT of both groups were in normal range clinically. Therefore, there was no clinical difference between the two groups actually. In our study, one patient of PH group suffered mild PE at postoperative day 2, continuous administration of heparin plus warfarin promoted the patient to recover soon. Moreover, one case received secondary VATS to do hemostasis in PL group, she also recovered successfully after second surgery and discharged. Christensen et al. found patients undergoing VATS lobectomy were normocoagulable preoperatively and VATS had no significant effect on the coagulation system (20). Attaran et al. also reported not all lung cancer patients were in hypercoagulable state, meanwhile administration of LMWH once or twice one day even could not provide sufficient thromboprophylaxis for lung cancer patients who were indeed in hypercoagulable status, suggesting the critical need of careful screening of coagulation state of patients before administration of anti-coagulation agents (19). The two patients maybe in the state described above or due to different sensitivity and tolerance to anti-coagulants.
Hypercoagulable status associated with malignancies was described first by Trousseau about 150 years ago, the theory malignant cancer patients were at a high risk of thromboembolism was accepted by most clinicians later, hypercoagulable status could be activated by neoplastic cells, related therapies (chemotherapy or surgical procedures) and other risks (6,21). Then many thromboprophylactic agents were used to prevent thrombosis. The inhibition of coagulation function of heparin was prohibiting the activation of thrombin, factor Xa and other clotting enzymes, the anticoagulant function of heparin deeply depended on antithrombin III, binding it and developing an anticoagulant complex, and the complex could increase the anticoagulant function more than one thousand times. However, it seems LMWH has become more popular and replaced heparin in many clinical indications due to the more predictable pharmacokinetic and pharmacodynamic properties (13,22). These findings were also pro our results that administration of LMWH was prior to heparin regarding bleeding related events.
Our study found preoperative administration of LMWH for thromboprophylaxis tended to decrease bleeding related events compared with heparin in video-assisted thoracoscopic lobectomy. Compared with postoperative heparin group, previous study of the series trial had showed preoperative use of heparin for Chinese patients undergoing thoracoscopic major thoracic surgery was safe and feasible, providing more sufficient thromboprophylaxis (14). Besides, another prospective study of the trial demonstrated preoperative administration of heparin affect the postoperative coagulation parameters compared with preoperative coagulation function, while both pre- and post-operative coagulation parameters were located in clinical normal range that the study came to the conclusion preoperative use of heparin did not actually influence the postoperative coagulation function clinically. Papageorgiou et al. reported postoperative administration of enoxaparin could improve blood hypercoagulability in patients diagnosed with localized primary lung adenocarcinoma (23). For patients undergoing thoracoscopic lobectomy, a prospective study found administration of LMWH did not alter the coagulation parameters compared to non-LMWH group, without bleeding events and thromboembolism occurring (17). What’s more, studies showed administration of LMWH could significantly decrease the hypercoagulable status of the lung cancer patients and prevent significantly the incidence of thromboembolism, without obviously increasing the bleeding related events, what was interesting was that administration of LMWH clearly deliver the overall survival benefit by inducing tissue factor pathway inhibitor (TFPI) or other materials release to inhibit migration of tumor cells (24-27). Akl et al. also demonstrated that administration of heparin brought benefit to overall survival of cancer patients, especially for lung cancer patients (26). On the contrary, some findings revealed whether administration of anti-coagulants could improve the overall survival of lung cancer patients was still undefined or even not, only resulting in a significant reduction in VTE incidence (4,18,28,29).
In summary, at present, it is widely recognized cancer patients are at a high risk of thromboembolism, while controversy do exist about the specific timing and dosage of anti-coagulants, our study explored effect of preoperative administration of LMWH and heparin for thromboprophylaxis on Chinese patients undergoing video-assisted thoracoscopic lobectomy. To our best knowledge, this is the first study to compare the influence of preoperative administration of heparin and LMWH in VATS enlightening new perspectives about thromboprophylaxis in this controversial field. Besides, this is a retrospective study but patients were collected from a randomized clinical trial that could decrease some bias in some degree owing to the complete data of patients. The limitations of this study are as follows: first, the sample size of two groups are relatively small, limiting our data analytical power. Besides, it is a retrospective study that could not provide very high evidence grade. Moreover, postoperative coagulation profile comparison was from the data of blood which was extracted in the morning of postoperative day 1 for all patients instead of at a particular time related to the administration point of anti-coagulants or after surgery. At last, this study was performed with Chinese which would be unknown whether it could be applicable to other race. Randomized controlled trials are badly needed to validate our results in the future.
Conclusions
In conclusion, compared with preoperative administration of heparin 5,000 IU twice a day, our study demonstrated preoperative thromboprophylactic administration of LMWH 4,000 IU once a day significantly decreased intraoperative bleeding volume and show less influence on coagulation profile for Chinese patients undergone VATS lobectomy. However, more multi-center, prospective studies are badly needed to provide evidence in future.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (No. 81672291, 31071210) (to YD Lin).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Committee of West China Hospital, Sichuan University (approval number: 20160601). Since the study was a retrospective analysis and analyzed anonymously, the ethics committee waived the need for consent.
References
- Kakkar AK, Haas S, Wolf H, et al. Evaluation of perioperative fatal pulmonary embolism and death in cancer surgical patients: the MC-4 cancer substudy. Thromb Haemost 2005;94:867-71. [PubMed]
- Song JQ, Xuan LZ, Wu W, et al. Low molecular weight heparin once versus twice for thromboprophylaxis following esophagectomy: a randomised, double-blind and placebo-controlled trial. J Thorac Dis 2015;7:1158-64. [PubMed]
- Zwicker JI, Bauer KA. How long is long enough? Extended anticoagulation for the treatment of cancer-associated deep vein thrombosis. J Clin Oncol 2014;32:3596-9. [Crossref] [PubMed]
- Macbeth F, Noble S, Evans J, et al. Randomized Phase III Trial of Standard Therapy Plus Low Molecular Weight Heparin in Patients With Lung Cancer: FRAGMATIC Trial. J Clin Oncol 2016;34:488-94. [Crossref] [PubMed]
- Salla E, Dimakakos EP, Tsagkouli S, et al. Venous Thromboembolism in Patients Diagnosed With Lung Cancer. Angiology 2016;67:709-24. [Crossref] [PubMed]
- Marinho FC, Takagaki TY. Hypercoagulability and lung cancer. J Bras Pneumol 2008;34:312-22. [Crossref] [PubMed]
- Scorza M, Liguori R, Elce A, et al. Biological role of mannose binding lectin: From newborns to centenarians. Clin Chim Acta 2015;451:78-81. [Crossref] [PubMed]
- Smith JA. Malignancies, Prothrombotic Mutations, and the Risk of Venous Thrombosis. J Urol 2005;174:1300. [Crossref] [PubMed]
- Noble S, Pasi J. Epidemiology and pathophysiology of cancer-associated thrombosis. Br J Cancer 2010;102 Suppl 1:S2-9. [Crossref] [PubMed]
- Di Nisio M, Peinemann F, Porreca E, et al. Primary prophylaxis for venous thromboembolism in patients undergoing cardiac or thoracic surgery. Cochrane Database Syst Rev 2015.CD009658. [PubMed]
- Hall IE, Andersen MS, Krumholz HM, et al. Predictors of venous thromboembolism in patients with advanced common solid cancers. J Cancer Epidemiol 2009;2009:182521. [Crossref] [PubMed]
- van Es N, Louzada M, Carrier M, et al. Predicting the risk of recurrent venous thromboembolism in patients with cancer: A prospective cohort study. Thromb Res 2018;163:41-6. [Crossref] [PubMed]
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e419S-96S.
- Deng HY, Shi CL, Li G, et al. The safety profile of preoperative administration of heparin for thromboprophylaxis in Chinese patients intended for thoracoscopic major thoracic surgery: a pilot randomized controlled study. J Thorac Dis 2017;9:1065-72. [Crossref] [PubMed]
- Alai GH, Deng HY, Li G, et al. The influence of heparin on coagulation function of patients undergoing video-assisted major thoracic surgery. J Thorac Dis 2018;10:2288-94. [Crossref] [PubMed]
- Larsen JB, Troldborg A, Christensen TD, et al. The lectin pathway and coagulation in lung cancer patients undergoing lobectomy - A randomised controlled trial. Thromb Res 2018;163:92-9. [Crossref] [PubMed]
- Christensen TD, Vad H, Pedersen S, et al. Coagulation profile in patients undergoing video-assisted thoracoscopic lobectomy: A randomized, controlled trial. PLoS One 2017;12:e0171809. [Crossref] [PubMed]
- Ek L, Gezelius E, Bergman B, et al. Randomized phase III trial of low-molecular-weight heparin enoxaparin in addition to standard treatment in small-cell lung cancer: the RASTEN trial. Ann Oncol 2018;29:398-404. [Crossref] [PubMed]
- Attaran S, Somov P, Awad WI. Randomised high- and low-dose heparin prophylaxis in patients undergoing thoracotomy for benign and malignant disease: effect on thrombo-elastography. Eur J Cardiothorac Surg 2010;37:1384-90. [Crossref] [PubMed]
- Christensen TD, Vad H, Pedersen S, et al. Video-assisted Thoracoscopic surgery (VATS) lobectomy for lung cancer does not induce a procoagulant state. Thromb J 2017;15:29. [Crossref] [PubMed]
- Hachey KJ, Sterbling H, Choi DS, et al. Prevention of Postoperative Venous Thromboembolism in Thoracic Surgical Patients: Implementation and Evaluation of a Caprini Risk Assessment Protocol. J Am Coll Surg 2016;222:1019-27. [Crossref] [PubMed]
- Abi Ghanem M, Saliba E, Irani J, et al. Effects of preoperative enoxaparin on bleeding after coronary artery bypass surgery. J Med Liban 2015;63:185-90. [Crossref] [PubMed]
- Papageorgiou C, Vandreden P, Marret E, et al. Lobectomy and postoperative thromboprophylaxis with enoxaparin improve blood hypercoagulability in patients with localized primary lung adenocarcinoma. Thromb Res 2013;132:584-91. [Crossref] [PubMed]
- Noble S. Low-molecular-weight heparin and survival in lung cancer. Thrombosis Research 2012;129:S114-8. [Crossref] [PubMed]
- Gamperl H, Plattfaut C, Freund A, et al. Extracellular vesicles from malignant effusions induce tumor cell migration: inhibitory effect of LMWH tinzaparin. Cell Biol Int 2016;40:1050-61. [Crossref] [PubMed]
- Akl EA, van Doormaal FF, Barba M, et al. Parenteral anticoagulation may prolong the survival of patients with limited small cell lung cancer: a Cochrane systematic review. J Exp Clin Cancer Res 2008;27:4. [Crossref] [PubMed]
- Zhuang X, Qiao T, Xu G, et al. Combination of nadroparin with radiotherapy results in powerful synergistic antitumor effects in lung adenocarcinoma A549 cells. Oncol Rep 2016;36:2200-6. [Crossref] [PubMed]
- van Doormaal FF, Di Nisio M, Otten HM, et al. Randomized trial of the effect of the low molecular weight heparin nadroparin on survival in patients with cancer. J Clin Oncol 2011;29:2071-6. [Crossref] [PubMed]
- Kucukoner M, Isikdogan A, Kaplan MA, et al. Can LMWH improve the outcome of patients with inoperable stage III non-small cell lung cancer? Contemp Oncol (Pozn) 2012;16:416-9. [Crossref] [PubMed]


