
Short-term outcomes after anatomic total shoulder arthroplasty in patients with osteoarthritis versus osteonecrosis
Introduction
Osteonecrosis (ON) of the shoulder is a slow progressive disease process with a poorly understood pathophysiology and an insidious initial presentation (1). Its pathogenesis may be rooted in both traumatic and non-traumatic injury, with corticosteroid use being the most common precipitating factor (2-5). This condition progresses to end stage disease with humeral head collapse, for which anatomic total shoulder arthroplasty (TSA) has become the mainstay of treatment (6,7). A previous study by Jain et al. evaluating 12,758 patients estimated that ON was the primary diagnosis in 3.3% to 4.7% of all TSA cases in the United States from 1990 to 2000 (8). While less prevalent, it remains necessary to understand what post-operative differences exist in this population when compared to osteoarthritis (OA) patients.
Primary OA is the most common indication for TSA, with several factors vital to determining short-term outcomes—including consideration of potential functional gains, quality of soft-tissue, and the risk of revision (9). Loosening of the glenoid has been shown to be the most common indication for TSA revision (10). The outcomes of TSA for glenohumeral OA have been extensively reported in the literature, however, there is a paucity of studies describing the procedure and outcomes in patients with glenohumeral ON. Therefore, to gain a better understanding of the TSA outcomes for shoulder ON, it becomes necessary to compare this group of patients to a shoulder OA cohort.
Currently, there are no studies that compare and evaluate trends of TSA in the glenohumeral OA population to those with ON. Therefore, the purpose of this study was to evaluate the short-term outcomes of TSA performed on patients with glenohumeral OA compared to those with ON. Specifically, we compared: (I) demographics; (II) length-of-stay (LOS); and (III) 30-day postoperative complication rates between TSA recipients who had OA versus ON.
Methods
Database
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database was retrospectively evaluated for this study. This database is a prospectively collected national database that collects patient’s perioperative information from over 700 hospitals (11). The data is collected by American College of Surgeons (ACS)-trained surgical clinical reviewers. Specifically, they concentrate on demographics, comorbidities, laboratory and intraoperative data, and discharge disposition. Additionally, it contains data regarding readmissions, reoperations, and morbidity and mortality for up to 30-day postoperatively (12,13). Furthermore, this is a validated database, which has a reported disagreement rate of less than 2% in inter-rater reliability audits (14).
Patient selection
There were 7,066 patients in the NSQIP database from 2008 and 2015 who had a diagnosis of glenohumeral OA or ON and received a TSA. OA patients were identified using the International Classification of Diseases, Ninth Revision (ICD-9) codes in the 715.xx range, including 715, 715.11, 715.21, 715.31, 715.36, 715.89, 715.9, and 715.91. The corresponding codes for ON used for case selection were in the 733.xx range, including 733.4, 733.41, and 733.49. The Current Procedural Terminology (CPT) treatment code used for TSA was 23472. To control for potential confounders, patients who had OA were matched (3:1) to patients who had ON using propensity score matching based on age, sex, race, and body mass index (BMI). There were 129 ON TSA patients and 387 OA TSA patients included in the analysis. Perioperative information including ASA scores, anesthesia types, operative times, LOS, and 30-day complication rates were compared between the groups using univariate analyses.
Statistical analysis
Statistical analyses, including matching analysis, were performed using SPSS v.23 for Mac (IBM Corp. Armonk, New York, USA). Regression analyses were performed to evaluate the LOS and 30-day postoperative complications (any, major, and minor). A P value of less than 0.05 was used to determine statistical significance.
Results
Demographics
Univariate analysis demonstrated that compared to the OA group, the ON group was different in terms of race (P=0.004), had higher Charlson/Deyo comorbidity index P=0.003), and higher American Society of Anesthesiologists (ASA) scores (55.0% vs. 45.0%, P=0.039) (Table 1). Additionally, the ON group was more likely to be on chronic corticosteroids, although this did not reach statistical significance (8.5% vs. 4.1%, P=0.052).
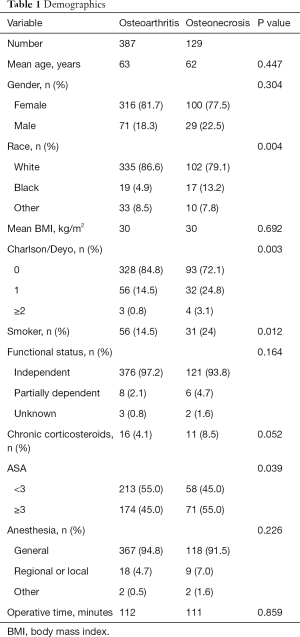
Full table
LOS
Compared to the OA group, the ON group had a 21.1% longer mean LOS (P=0.05), from an average LOS of 1.96 days to an average LOS of 2.37 days. Compared to the OA group, the total number of days from operation to discharge (DOTD) in the ON group were 14.0% longer, from an average DOTD of 1.92 days to an average DOTD of 2.19 days.
Thirty-day postoperative complication rates
Overall complication rates were low in both groups, at 6.1% and 5.4% for the ON and OA cohorts respectively. Univariate analysis indicated that compared to the OA group, the ON group had a 107% increased risk for developing any complication, although this did not reach significance [odds ratio (OR) =2.07; 95% CI, 0.94 to 4.57; P=0.07] (Table 2). There was no notable difference observed for increased risk of pulmonary embolism, acute renal failure, stroke, cardiac arrest, myocardial infarction, sepsis, septic shock, or reoperation. Moreover, the ON group had a 134% higher risk for developing a minor complication compared to the OA group (OR =2.34; 95% CI, 1.01 to 5.42; P=0.047). Of the minor complications, there was an increased risk of developing urinary tract infection (OR 1.97; 95% CI, 0.17 to 22.05; P=0.582) and receiving a transfusion in the OR (OR =2.15; 95% CI, 0.86 to 5.38; P=0.102) in the ON group with no minor complications achieving statistical significance.
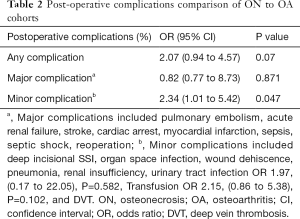
Full table
Discussion
TSA is often successful in treating end-stage degenerative shoulder disease (15,16). While OA is the most common etiology of degenerative shoulder disease, ON of the glenoid and humeral head is also a known factor of pathogenesis (17,18). Unlike OA, the management of ON of the humeral head can be difficult as a result of the different etiologies and controversies regarding the optimal type and timing of surgery (19-21). Published literature indicates that ON may play a role in anywhere from 3% to 5% of all TSAs performed, and while OA and ON are two common reasons for undergoing TSA, their short-term outcomes have not been directly compared (8). In the present study, we used the American College of Surgeons National Surgical Quality Improvement Program database to compare the perioperative and post-operative characteristics of TSA performed for OA and ON from 2008 to 2015. The present study demonstrated that the ON patients undergoing TSA have more comorbidities than patients undergoing OA, with increased LOS, but no statistically significant difference in post-operative complication rates.
The present study had several limitations. This study used a large national database as its data source, which may be subject to data collection errors. However, the American College of Surgeons performs quality assessments of the data with inter-rater reliability audits, which has a reported disagreement rate of less than 2% (14). Although the number of hospitals that participate in NSQIP has grown each year, with over 700 hospitals currently participating, a higher number of patients likely underwent TSA for both OA and ON but were not captured by this database. Additionally, the specific etiologies and stage of ON could not be determined from the database. Also, the surgical approaches for TSA could not be extracted. Even though the sample size may not capture all patients undergoing TSA for OA or ON, the geographically widespread involvement of various hospitals across the country may allow for our results to be extrapolated and generalized.
This is the first known comparison of short-term outcomes for OA with ON in TSA, providing informative analysis regarding the similarities and differences between these groups. The findings in this study are broadly consistent with prior studies on the reported course of post-operative long- and short-term outcomes from TSA in patients with ON (6,22,23). In study of 36 patients with ON receiving TSA, Hattrup et al. reported symptomatic improvement in nearly 90% of patients (6). In a cohort of 71 TSA procedures for atraumatic ON, Schoch et al. reported a complication rate 14% and a reoperation rate of 15% (23). Contrastingly, a study of 46 patients with post-traumatic ON receiving TSA, demonstrated a complication rate of approximately 35% and a reoperation rate of 10%, suggesting that the mechanism of ON is important in predicting the rate of complications (22).
In contrast, others have reported associations between ON and postoperative complications that were not demonstrated in the present study as significantly different from those found in OA patients undergoing TSA. In a large database study of 4,030 patients who underwent TSA, Bernstein et al. examined and modeled the key risk factors leading to increased post-operative complications, finding no significant risk factors outside of total operating time (hours) (OR =1.26; 1.04 to 1.53) and hypertension requiring medications (OR =1.95; 95% CI, 1.01 to 3.76) (24). The present study differs from these findings, as it analyzed both patients with ON and OA undergoing TSA and did not exclude any patients by ASA score and did not include reverse TSA. The impact of ON on postoperative complication rates may further vary with the TSA approach that is performed, which should be considered in preoperative management of such patients.
In our study, there were no statistically significant differences in LOS and complication rates in patients undergoing TSA with glenohumeral ON compared with those with OA. This information may allow orthopaedists to educate ON patients on these potential risks and benefits associated with TSA. Future studies should compare differences between traumatic and atraumatic ON, as well as between reverse and anatomic total shoulder arthroplasties. Nevertheless, these results indicate the need to establish better management strategies for patients with ON after TSA in order to mitigate their increased risk.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- L'Insalata JC, Pagnani MJ, Warren RF, et al. Humeral head osteonecrosis: clinical course and radiographic predictors of outcome. J Shoulder Elbow Surg 1996;5:355-61. [Crossref] [PubMed]
- Hasan SS, Romeo AA. Nontraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg 2002;11:281-98. [Crossref] [PubMed]
- Gerber C, Hersche O, Berberat C. The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elbow Surg 1998;7:586-90. [Crossref] [PubMed]
- Mont MA, Payman RK, Laporte DM, Petri M, Jones LC, Hungerford DS. Atraumatic osteonecrosis of the humeral head. J Rheumatol 2000;27:1766-73. [PubMed]
- Gruson KI, Kwon YW. Atraumatic osteonecrosis of the humeral head. Bull NYU Hosp Jt Dis 2009;67:6-14. [PubMed]
- Hattrup SJ, Cofield RH. Osteonecrosis of the humeral head: results of replacement. J Shoulder Elbow Surg 2000;9:177-82. [Crossref] [PubMed]
- Parsch D, Lehner B, Loew M. Shoulder arthroplasty in nontraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg 2003;12:226-30. [Crossref] [PubMed]
- Jain NB, Higgins LD, Guller U, et al. Trends in the epidemiology of total shoulder arthroplasty in the United States from 1990-2000. Arthritis Rheum 2006;55:591-7. [Crossref] [PubMed]
- Foruria AM, Sperling JW, Ankem HK, et al. Total shoulder replacement for osteoarthritis in patients 80 years of age and older. J Bone Joint Surg Br 2010;92:970-4. [Crossref] [PubMed]
- Haines JF, Trail IA, Nuttall D, et al. The results of arthroplasty in osteoarthritis of the shoulder. J Bone Joint Surg Br 2006;88:496-501. [Crossref] [PubMed]
- Molina CS, Thakore RV, Blumer A, et al. Use of the National Surgical Quality Improvement Program in orthopaedic surgery. Clin Orthop Relat Res 2015;473:1574-81. [Crossref] [PubMed]
- Sathiyakumar V, Molina CS, Thakore RV, et al. ASA score as a predictor of 30-day perioperative readmission in patients with orthopaedic trauma injuries: an NSQIP analysis. J Orthop Trauma 2015;29:e127-32. [Crossref] [PubMed]
- Cohen ME, Ko CY, Bilimoria KY, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 2013;217:336-46.e1. [Crossref] [PubMed]
- Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 2010;210:6-16. [Crossref] [PubMed]
- Matsen FA 3rd. Early effectiveness of shoulder arthroplasty for patients who have primary glenohumeral degenerative joint disease. J Bone Joint Surg Am 1996;78:260-4. [Crossref] [PubMed]
- Menge TJ, Boykin RE, Byram IR, et al. A comprehensive approach to glenohumeral arthritis. South Med J 2014;107:567-73. [Crossref] [PubMed]
- Wiater JM, Fabing MH. Shoulder arthroplasty: prosthetic options and indications. J Am Acad Orthop Surg 2009;17:415-25. [Crossref] [PubMed]
- Boileau P, Sinnerton RJ, Chuinard C, et al. Arthroplasty of the shoulder. J Bone Joint Surg Br 2006;88:562-75. [Crossref] [PubMed]
- Barlow JD, Abboud J. Surgical options for the young patient with glenohumeral arthritis. Int J Shoulder Surg 2016;10:28-36. [Crossref] [PubMed]
- Mont MA, Maar DC, Urquhart MW, et al. Avascular necrosis of the humeral head treated by core decompression. A retrospective review. J Bone Joint Surg Br 1993;75:785-8. [Crossref] [PubMed]
- Harreld KL, Marker DR, Wiesler ER, et al. Osteonecrosis of the humeral head. J Am Acad Orthop Surg 2009;17:345-55. [Crossref] [PubMed]
- Schoch BS, Barlow JD, Schleck C, et al. Shoulder arthroplasty for post-traumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg 2016;25:406-12. [Crossref] [PubMed]
- Schoch BS, Barlow JD, Schleck C, et al. Shoulder arthroplasty for atraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg 2016;25:238-45. [Crossref] [PubMed]
- Bernstein DN, Keswani A, Ring D. Perioperative Risk Adjustment for Total Shoulder Arthroplasty: Are Simple Clinically Driven Models Sufficient?. Clin Orthop Relat Res 2017;475:2867-74. [Crossref] [PubMed]


