
Left lower lobe sleeve resection for endobronchial schwannoma
Introduction
Schwannoma is a mesenchymal neoplasm originating from Schwann cells of the nerve sheath. Primary pulmonary schwannoma is an extremely rare tumor, which accounts for less than 0.2% of all lung tumors. The diagnosis of endobronchial schwannoma is difficult due to the fact that most patients are asymptomatic. The main differential diagnoses include neurofibroma, neurilemmoma and neurogenic sarcoma. Surgery is the preferred treatment of schwannoma. We present a rare case of a schwannoma arising from left main bronchus.
Case presentation
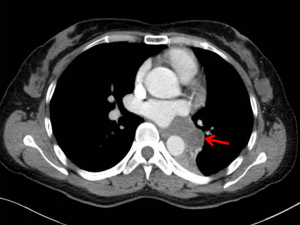
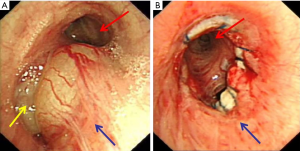
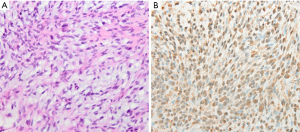
A 42-year-old female presented to our hospital with a 1-month history of hemoptysis. She denied family history and past medical history. Physical examination and routine laboratory analyses were unremarkable. A computed tomography (CT) of chest with contrast revealed a 2.4 cm × 4.3 cm, soft-tissue tumor mass with irregular enhancement located in the left hilar and paraspinal sulcus. The left lower lobe bronchus was embedded in the mass (Figure 1). Subsequently, a bronchoscopy was performed and showed that neoformation protruded into the lower part of left main bronchus and the left lower lobe bronchus was almost completely blocked (Figure 2A). With the results presented above, we hypothesized that the tumor may be carcinoid tumour. The endobronchial biopsy showed that a submucosal spindle cell proliferation and a chronic mucosal inflammation accompanied with squamous metaplasia in the bronchial epithelium. It was suspected to be peripheral nerve tumors. However, it does not rule out the possibility of malignant tumors. The patient underwent the left lower lobectomy and end-to-end anastomosis between the left main bronchus and the upper left bronchus after systemic evaluation (Figure 2B). Benign nature of the endobronchial tumor was verified via fast frozen section examination. The postoperative pathology study confirmed endobronchial schwannoma (Figure 3A), and immunohistochemistry with S-100 protein was positive (Figure 3B), but negative for SMA, TTF1, CK7, MART-1 and desmin. The patient underwent an uneventful post-operative course without complications. On the seventh day after surgery, bronchoscopy showed a good end-to-end anastomosis. At one-year follow-up, there was no evidence of tumor recurrence.
Discussion
Schwannomas are mesenchymal neoplasms originating from Schwann cells of the nerve sheath. They may appear anywhere on the body, while they have a predilection for the extremities, trunk, retroperitoneum, head and neck (1). Primary pulmonary schwannoma is an extremely rare tumor, accounting for less than 0.2% of all lung tumors (2). Endobronchial schwannoma was first described by Feldhaus in 1989 (3), and there have been no more than 30 cases reported in the English literature up to now. Some endobronchial schwannomas are asymptomatic and discovered incidentally on radiographs. Common signs and symptoms include fever, cough, hemoptysis, dyspnea, and post-obstructive pneumonia in symptomatic patients. It is difficult to diagnose schwannoma based on clinical manifestations. Bronchoscopy is often used to further confirm the location, size, shape, and obstruction of the lesion in the bronchus. The differential diagnosis for endobronchial schwannomas includes neurofibroma, neurilemmoma and neurogenic sarcoma. Pathological biopsy and immunohistochemistry are the gold standard for diagnosis of this tumor.
Treatment options of endobronchial schwannomas are usually determined by the size and location of the tumor. In most cases, surgery is the preferred treatment option (4). Among that, lobectomy is considered the standard treatment for some central pulmonary schwannomas. In our case, although the tumors located in a troublesome position of the lower part of left main bronchus and left lower lobe bronchus, sleeve lobectomy of the left lower lobe not only completely remove the tumor, but also retain the patient’s upper lobe. Recently, bronchoscopic treatment has been proved to be a safe and efficient tool for benign tracheobronchial tumors (5). However, there are few reports on bronchoscopic removal of endobronchial schwannoma (6,7).
As schwannomas are benign tumors, there are rarely reports of schwannoma with malignant transformation, and the prognosis of schwannomas usually is optimistic (8). However, long follow-up is needed for monitoring the tumor growth and reducing the risk of recurrence after resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Murphy J, Giunta JL. Atypical central neurilemmoma of the mandible. Oral Surg Oral Med Oral Pathol 1985;59:275-8. [Crossref] [PubMed]
- Roviaro G, Montorsi M, Varoli F, et al. Primary pulmonary tumours of neurogenic origin. Thorax 1983;38:942-5. [Crossref] [PubMed]
- Feldhaus RJ, Anene C, Bogard P. A rare endobronchial neurilemmoma (Schwannoma). Chest 1989;95:461-2. [Crossref] [PubMed]
- Bosch X, Ramirez J, Font J, et al. Primary intrapulmonary benign schwannoma. A case with ultrastructural and immunohistochemical confirmation. Eur Respir J 1990;3:234-7. [PubMed]
- Pandey K, Vaidya PJ, Kate AH, et al. Bronchoscopic and surgical management of rare endobronchial tumors. J Cancer Res Ther 2016;12:1093-7. [Crossref] [PubMed]
- Madan K, Agarwal R, Bal A, et al. Bronchoscopic management of a rare benign endobronchial tumor. Rev Port Pneumol 2012;18:251-4. [Crossref] [PubMed]
- Jung YY, Hong ME, Han J, et al. Bronchial schwannomas: clinicopathologic analysis of 7 cases. Korean J Pathol 2013;47:326-31. [Crossref] [PubMed]
- Rowlands D, Edwards C, Collins F. Malignant melanotic schwannoma of the bronchus. J Clin Pathol 1987;40:1449-55. [Crossref] [PubMed]


