
Validity and reliability of patient section of evidence-based medical records about doctor-patient building through integrated therapy of traditional Chinese and Western medicine (DPEBMR-P) in patients with gastrointestinal diseases
Introduction
The definition of health-related quality of life (HRQoL) is a multidimensional concept, which includes physical, mental, and social dimensions (1-4). The assessment of patients’ HRQoL could assist clinicians in evaluating the efficacy of the interventions. In the field of gastrointestinal diseases, there are many disease-specific HRQoL instruments; however, they all have limitations. For instance, GERD-HRQL assessed the symptom’s severity rather than HRQoL (5). The Reflux questionnaire mixed HRQoL and symptoms (6). GERD-QOL was a pure HRQoL instrument (7), but its social domain was vague, and it only recruited patients with GERD who had received esomeprazole.
To overcome these limitations, we developed a new instrument titled the evidence-based medical record about doctor-patient building through integrated therapy of traditional Chinese and Western medicine (DPEBMR) which could be applied in patients with gastrointestinal diseases who received any of the possible therapies. The instrument was categorized as into a doctor section and a patient section. In this article, our main goal was to test the validity and reliability of patients section for DPEBMR (DPEBMR-P).
Methods
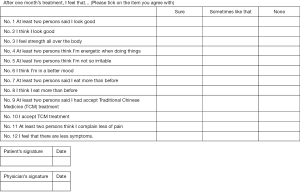
The study measured the reliability and validity of the DPEBMR-P among 98 patients with gastrointestinal diseases. DPEBMR-P contains 12 items, and the details of these items are in Figure 1.
Participants
The inclusion criteria were the following: adults with functional dyspepsia, gastroesophageal reflux disease, chronic non-atrophic gastritis, precancerous lesions of gastric carcinoma, peptic ulcers, irritable bowel syndrome, ulcerative colitis or chronic constipation which were diagnosed through gastroscopy, enteroscopy or biopsy. The exclusion criteria were the following: a diagnosis was made at least 6 months before, any co-morbidity with 2 or more systems, patients with major mental illness.
Interventions
The study did not restrict the treatment regimens of included patients. However, our hospital had standard therapies for the relevant diseases. For patients who had Helicobacter pylori infections, they received quadruple therapy if they were allergic to amoxicillin. Otherwise, they were treated with a sequential therapy. More detailed information can be found in supplementary. For patients without Helicobacter pylori infection, Chinese traditional medicine (lianzhuliyi pill and huaganjian) was prescribed if they had no heartburn or regurgitation, or we chose step-down therapy—initial two weeks: proton pump inhibitor; following two weeks: Chinese traditional medicine (lianzhuliyi pill and huaganjian). For patients with precancerous lesions of gastric carcinoma, another Chinese traditional medicine (sijunzi soup, banxiaxiexin soup, xiaoyao powder, xiangsu drink and zhishu pill) was used.
Statistical analysis
All data were analyzed using the SAS software, version 9.2. All statistical inferences were made of two-sided test, and a value of P<0.05 was considered to be statistically significant. For missing data, the Last Observation Carried Forward method was used to impute. The inter-item correlation matrix was performed to evaluate the repeatability of the item. Principal components factor analysis and Cronbach’s alpha were used to calculate the construct validity and internal consistency, respectively. If the initial eigenvalue of the item was larger than 1, it was regarded as a factor (8). If the value of Cronbach’s alpha was larger than 0.7, it meant internal consistency was high (9).
Results
Of the 100 patients recruited, 98 completed the fourth follow-up. The mean age of these patients was 48.6 (SD: 14.7). More than half of them were female (57.1%). Most of them (79.6%) received only traditional Chinese medicine (TCM), some (18.4%) accepted both TCM and western drugs, and the rest (2%) were treated by only western drugs. The results of the inter-item correlation matrix failed to find any large correlation coefficients among the different items, which indicated the repeatability of the item was low.
Construct validity
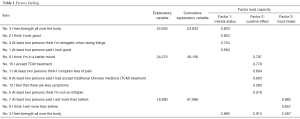
The score of the Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.811 (more than 0.5), which indicated sufficient common factors among variables. Meanwhile, the Bartlett’s test of sphericity had a significant result (P<0.05). Thus, it was appropriate to conduct a principal component factor analysis test. A total of 3 items were identified as factors, and they accounted for 68% of the total variance. Then, we conducted a principle component analysis test with a varimax rotation to test the 3 factors.
The results (Table 1) indicate that each item had a high loading: items of mental status (0.584 to 0.833), items of therapeutic effect (0.518 to 0.797), and items of appetite (0.857 to 0.882).
Full table
Internal consistency
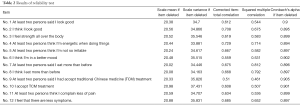
Table 2 displays the results of the reliability test. The Cronbach’s alpha for overall scale was 0.906 and sub-scales ranged from 0.894 to 0.905. Thus, DPEBMR-P had a high internal consistency.
Full table
Discussion
Our study developed a new 12-item instrument to assess the efficacy of therapies in patients with gastrointestinal diseases. The patient section has a high degree of internal consistency and construct validity.
Our study has several strengths: first, our study was a real-world study which means that the results can be applied more extensively in patients with gastrointestinal diseases. Moreover, previous studies only focused on specific patients: GERD (5-7,10,11), dyspepsia or irritable bowel syndrome (12), and esophagitis (13). Our tool was more practical than the previous ones. Furthermore, our study considered others’ sayings towards patients which previous studies had paid little attention to. Previous studies even with the generic instrument SF-36 and the EQ-5D did not include the items related to what the others said towards the patients (14,15). However, our feelings or thoughts might be influenced by others’ sayings (16). Thus, it is necessary to include items about what the others are saying because HRQoL as an instrument is a multidimensional tool which should include any factors which can influence the patients’ health status. Finally, to the best of our knowledge, our study was the first to recruit patients who received TCM treatment. TCM has been proven to be an effective intervention in treating patients with GERD (17,18), and so it was necessary to include patients who received TCM.
Still, some limitations should be discussed. First of all, the sample size of our study was limited which might make the results unstable. However, our research was continuously performed, and we will recruit more patients in the future to make the results more robust. Also, the age range in our study was from 33.9 to 63.3. Thus, our results may not be applicable to older or younger patients.
Conclusions
DPEBMR-P is a useful tool to assess the efficacy of therapies in patients with gastrointestinal diseases.
Details of therapies
H. pylori test: positive. Initially, patients received eradication (Table S1).
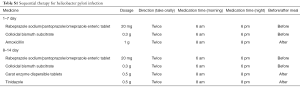
Full table
If patients are sensitive to amoxicillin: quadruple chemotherapy for Helicobacter pylori infection (Table S2).

Full table
Acknowledgements
Funding: This study was funded by the National Natural Science Funds of China (No. 81774146 and 81303151) and the Beijing NOVA Program (No. xxjh2015A093 and No. Z1511000003150125).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Ethics Committee from Xiyuan Hospital, China Academy of Traditional Chinese Medicine.
References
- Ebrahim S. Clinical and public health perspectives and applications of health-related quality of life measurement. Soc Sci Med 1995;41:1383-94. [Crossref] [PubMed]
- Japhet Killewo KH, Quah SR. Epidemiology and Demography in Public Health. 1 ed. Academic Press, 2010.
- Gold MR, Sigel JE, Russell LB, et al. Cost-Effectiveness in Health and Medicine. 1 ed. Oxford University Press, 1996.
- Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis 1987;40:593-603. [Crossref] [PubMed]
- Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 2007;20:130-4. [Crossref] [PubMed]
- Macran S, Wileman S, Barton G, et al. The development of a new measure of quality of life in the management of gastro-oesophageal reflux disease: the Reflux questionnaire. Qual Life Res 2007;16:331-43. [Crossref] [PubMed]
- Chan Y, Ching JY, Cheung CM, et al. Development and validation of a disease-specific quality of life questionnaire for gastro-oesophageal reflux disease: the GERD-QOL questionnaire. Aliment Pharmacol Ther 2010;31:452-60. [Crossref] [PubMed]
- Leandre R. Fabrigar DTW. Exploratory Factor Analysis (Understanding Statistics). 1 ed. Oxford University Press, 2011.
- Mesbah M, Cole BF, Lee ML. Statistical Methods for Quality of Life Studies: Design, Measurements and Analysis. 1 ed. Springer, 2002.
- Coyne KS, Wiklund I, Schmier J, et al. Development and validation of a disease-specific treatment satisfaction questionnaire for gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2003;18:907-15. [Crossref] [PubMed]
- Wiklund IK, Junghard O, Grace E, et al. Quality of Life in Reflux and Dyspepsia patients. Psychometric documentation of a new disease-specific questionnaire (QOLRAD). Eur J Surg Suppl 1998.41-9. [PubMed]
- Chassany O, Marquis P, Scherrer B, et al. Validation of a specific quality of life questionnaire for functional digestive disorders. Gut 1999;44:527-33. [Crossref] [PubMed]
- Holtmann G, Chassany O, Devault KR, et al. International validation of a health-related quality of life questionnaire in patients with erosive gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2009;29:615-25. [Crossref] [PubMed]
- Cunillera O, Tresserras R, Rajmil L, et al. Discriminative capacity of the EQ-5D, SF-6D, and SF-12 as measures of health status in population health survey. Qual Life Res 2010;19:853-64. [Crossref] [PubMed]
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83. [Crossref] [PubMed]
- Aronson E, Wilson TD, Akert RM. Social Psychology. 8 ed. Pearson, 2012.
- Gao LJ, Bai XH. Clinical Trial of Acupuncture Treatment of Gastro-esophageal Reflex Disease by Needling Dorsal Segment of the Governor Vessel. Zhen Ci Yan Jiu 2016;41:150-3. [PubMed]
- Zhu J, Guo Y, Liu S, et al. Acupuncture for the treatment of gastro-oesophageal reflux disease: a systematic review and meta-analysis. Acupunct Med 2017;35:316-23. [Crossref] [PubMed]


