
Re-biopsy in lupus nephritis
Lupus nephritis is a disease of mostly young females that puts them at high risk for endstage renal disease and the need for renal replacement therapies later in life (1,2). Rigorous control of the first episode and preventing the patient from any further episodes are essential to minimize nephron losses beyond the age-related nephron atrophy to maximize kidney life span (3). Treat-to-target induction therapy of lupus nephritis aims to suppress systemic autoimmunity as well as intrarenal inflammation. Maintenance therapy aims to minimize persistent systemic autoimmunity and to prevent flares of lupus nephritis. For how long maintenance treatment must be continued is unknown. Reliable predictors allowing personalized decision making are lacking (4). A recent article by De Rosa et al. published in Kidney International provides first prospective data on whether or not to continue maintenance immunosuppression in patients in complete clinical renal remission (5).
In this prospective study the authors studied 44 patients with class III/IV ± V lupus nephritis on the initial diagnostic kidney biopsy that had received induction therapy with steroids and cyclophosphamide for 6 months and maintenance therapy with mycophenolate mofetil or mycophenolic acid for at least 30 months. All patients had responded well to this treatment and were in complete clinical renal remission for at least 12 months, so a second kidney biopsy was performed to test for histological remission of immune complex disease. Two years later complete data on the relationship of lupus nephritis flare rates to histology of the second biopsy was available from 36 patients, of which 11 developed a renal flare, while 25 remained in complete clinical renal remission. The analysis revealed that among all the clinical, laboratory, and histological parameters only the second biopsy`s activity index, namely endocapillary proliferation, subendothelial immune complex deposits, and the presence pf glomerular leukocytes predicted the subsequent renal flare. Other parameters such as proteinuria, serum complement levels, presence of anti-dsDNA IgG or the chronicity index did not predict future flares of lupus nephritis (5). Indeed, of the 11 patients that flared 10 had persistent lupus nephritis activity on the second biopsy and all patients with an activity index of 2 or more flared. The authors concluded a repeat kidney biopsy to be useful in managing maintenance immunosuppression and that withdrawal of therapy may be safe only in patients with complete histologic remission.
This study is important in many ways. First, it documents that all traditional parameters that are regularly assessed in lupus nephritis clinics may not reliably predict future flares and in guiding decision making regarding the withdrawal of maintenance immunosuppression. Second, this study confirms that histological analysis is able to guide risk-benefit assessment in this context, although De Rosa et al. did not report the complication rate of their repeat biopsies (5). Third, the study defines a clear threshold of the activity index as well as a new formular that can predict future flares at high sensitivity and specificity. This approach will help to personalize treatments as an important element to minimize unnecessary exposure to immunosuppressive drugs and to avoid inappropriate treatment withdrawal in patients at risk for a future flare. Again, avoiding a second flare of lupus nephritis is absolutely essential to maximize the dialysis-free life span of the patient.
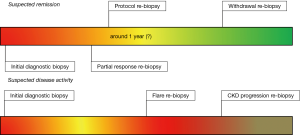
Whether or not repeat kidney biopsies should be endorsed in lupus patients remains debated among nephrologists and rheumatologists and local preferences predominate. The current published evidence is dominated by single center retrospective analyses of repeat biopsy cohorts performed on the occasion of lupus nephritis flares and the analysis remains mostly limited on the comparison of lupus nephritis classes between the first and second episode (6-8). Performing a repeat biopsy on the occasion a proteinuric or nephritic flare is only one of many possible rebiopsy scenarios and it is important when discussing about the pros and cons of repeat kidney biopsy in lupus nephritis to dissect those (Figure 1, Table 1). Another frequent scenario is the partial response to treatment usually with some persistent proteinuria leaving the clinician unsure whether to increase or switch immunosuppression for persistent disease activity or to go on tapering immunosuppression and enforce blockade of the renin-angiotensin system during delayed healing of the injured glomerular filtration barrier (9). Indeed, the uncertainty about sufficient control of immunological remission is very common because the current criteria to assess treatment response are based on parameters that by definition are unable to reliably inform about intrarenal inflammation versus persistent damage and scaring, i.e., hematuria, proteinuria, and serum creatinine levels (10). Few studies based on protocol biopsies or also refered to as post-induction biopsies, i.e., repeat biopsies performed after a fixed time point after concluding induction therapy or biopsies performed for partial remissions, document a disappointing discrepancy between clinical response and immunological response (11-13). The authors of these studies enforce the need for such post-induction or partial remission biopsies to guide drug therapy. It is of note that immunological remission assessed on protocol biopsies may be also an important endpoint for future clinical trials, as the analysis and interpretation of many of the recent lupus nephritis trials may be compromized by primary endpoints such as proteinuria, urinary sediment, and serum creatinine, that do not at all directly relate to the mechanism-of-action of immunosuppresive drugs (4). In addition, the expanding field of biomarker research in lupus nephritis will remain without progress also in the future unless protocol biopsies become available as the gold standard for validating novel biomarkers of post-induction lupus nephritis disease activity (4). Finally, repeat kidney biopsy can be useful in patients with a progressive increase in serum creatinine to dissect persistent immunological disease activity from non-immunological mechanisms of chronic kidney disease (CKD) progression (3,9) (Figure 1).
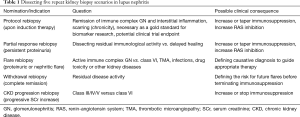
Full table
Much progress has been made since the last management recommendations for adult lupus nephritis have been released by leading bodies in the field (14-16), none of them providing a comprehensive, specific and proactive guidance on the use of repeat kidney biopsy in the management of patients with lupus nephritis. Experts in non-renal lupus are searching new ways to better define patients at low or high risk for disease progression, e.g., by employing criteria such as the Lupus Low Disease Activity State or in defining disease remission (17). More evidence is needed to move this topic forward from opinion-based to evidence-based recommendations in the future. The article by De Rosa et al. is important in this context as it provides first clinical evidence that a “Withdrawal rebiopsy” can be useful to guide drug therapy in patients with long term complete clinical renal remission (5). It will be important to generate also more evidence for the use of “Protocol biopsies”, “Partial response rebiopsies”, “Flare rebiopsies”, and “CKD progression rebiopsies” to generate solid data for future recommendations. In this context, it will be important to critically review the risks of such repeat biopsies, that seem generally low except for lupus patients under 18 years old or with elevated serum creatinine levels, prolonged prothrombin time, or thrombocytopenia (18,19). It is of note that repeat biopsy is not the only diagnostic tool in patients with suspected persistent lupus nephritis. Drug non-adherence and genetic causes of proteinuria or CKD progression require other diagnostic approaches, e.g., genetic testing for podocyte and CKD risk genes (20).
In summary, this prospective study at first provides supportive data for the use of a “Withdrawal rebiopsy” in guiding drug therapy in patients with lupus nephritis and long-lasting complete clinical renal remission. Other potential indications for a repeat biopsy exist in lupus patients and should receive similar attention to further improve the long term outcomes of patients with lupus nephritis.
Acknowledgements
Funding: HJ Anders was supported by the Deutsche Forschungsgemeinschaft (AN372/24-1) and by the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 668036 (project RELENT).
Footnote
Conflicts of Interest: The author and the last author of the discussed paper are both board members of the Lupus Nephritis Trials Network that has an academic interest in exploring the diagnostic potential of re-biopsies in the management of patients with lupus nephritis.
References
- Kaul A, Gordon C, Crow MK, et al. Systemic lupus erythematosus. Nat Rev Dis Primers 2016;2:16039. [Crossref] [PubMed]
- Anders HJ, Rovin B. A pathophysiology-based approach to the diagnosis and treatment of lupus nephritis. Kidney Int 2016;90:493-501. [Crossref] [PubMed]
- Romagnani P, Remuzzi G, Glassock R, et al. Chronic kidney disease. Nat Rev Dis Primers 2017;3:17088. [Crossref] [PubMed]
- Anders HJ, Jayne DR, Rovin BH. Hurdles to the introduction of new therapies for immune-mediated kidney diseases. Nat Rev Nephrol 2016;12:205-16. [Crossref] [PubMed]
- De Rosa M, Azzato F, Toblli JE, et al. A prospective observational cohort study highlights kidney biopsy findings of lupus nephritis patients in remission who flare following withdrawal of maintenance therapy. Kidney Int 2018;94:788-94. [Crossref] [PubMed]
- Alsuwaida AO. The clinical significance of serial kidney biopsies in lupus nephritis. Mod Rheumatol 2014;24:453-6. [Crossref] [PubMed]
- Pagni F, Galimberti S, Goffredo P, et al. The value of repeat biopsy in the management of lupus nephritis: an international multicentre study in a large cohort of patients. Nephrol Dial Transplant 2013;28:3014-23. [Crossref] [PubMed]
- Narvaez J, Ricse M, Goma M, et al. The value of repeat biopsy in lupus nephritis flares. Medicine (Baltimore) 2017;96:e7099. [Crossref] [PubMed]
- Moroni G, Pasquali S, Quaglini S, et al. Clinical and prognostic value of serial renal biopsies in lupus nephritis. Am J Kidney Dis 1999;34:530-9. [Crossref] [PubMed]
- Gordon C, Jayne D, Pusey C, et al. European consensus statement on the terminology used in the management of lupus glomerulonephritis. Lupus 2009;18:257-63. [Crossref] [PubMed]
- Malvar A, Pirruccio P, Alberton V, et al. Histologic versus clinical remission in proliferative lupus nephritis. Nephrol Dial Transplant 2017;32:1338-44. [Crossref] [PubMed]
- Pineiro GJ, Arrizabalaga P, Sole M, et al. Repeated Renal Biopsy - A Predictive Tool to Assess the Probability of Renal Flare in Lupus Nephritis. Am J Nephrol 2016;44:439-46. [Crossref] [PubMed]
- Arends S, Grootscholten C, Derksen RH, et al. Long-term follow-up of a randomised controlled trial of azathioprine/methylprednisolone versus cyclophosphamide in patients with proliferative lupus nephritis. Ann Rheum Dis 2012;71:966-73. [Crossref] [PubMed]
- Bertsias GK, Tektonidou M, Amoura Z, et al. Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis 2012;71:1771-82. [Crossref] [PubMed]
- Glomerulonephritis KDIGOK. Group. W. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl 2012;2:221-32.
- Hahn BH, McMahon MA, Wilkinson A, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res (Hoboken) 2012;64:797-808. [Crossref] [PubMed]
- van Vollenhoven R, Voskuyl A, Bertsias G, et al. A framework for remission in SLE: consensus findings from a large international task force on definitions of remission in SLE (DORIS). Ann Rheum Dis 2017;76:554-61. [Crossref] [PubMed]
- Chen TK, Estrella MM, Fine DM. Predictors of kidney biopsy complication among patients with systemic lupus erythematosus. Lupus 2012;21:848-54. [Crossref] [PubMed]
- Sun YS, Sun IT, Wang HK, et al. Risk of complications of ultrasound-guided renal biopsy for adult and pediatric patients with systemic lupus erythematosus. Lupus 2018;27:828-36. [Crossref] [PubMed]
- Romagnani P, Giglio S, Angelotti ML, et al. Next generation sequencing and functional analysis of patient urine renal progenitor-derived podocytes to unravel the diagnosis underlying refractory lupus nephritis. Nephrol Dial Transplant 2016;31:1541-5. [Crossref] [PubMed]


