New technique: practical procedure of robotic arm-assisted (MAKO) total hip arthroplasty
Introduction
Proper prosthesis size selection and precise intraoperative prosthesis installation are key steps for a successful total hip arthroplasty. In traditional manual operation, prosthesis size selection was determined by presurgical templating and intraoperative adjustment. The templating procedure was performed on plain films. Therefore, it could be largely affected by the position of patients when taking radiography. Besides this, the intraoperative selection of prosthesis size and the accuracy of prosthesis installation largely relied on the surgeon’s experience.
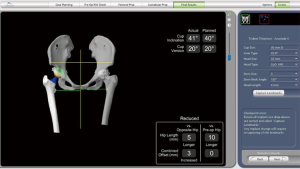
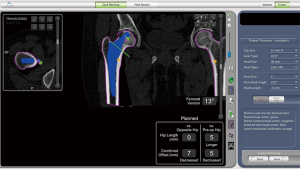
Recently, precise arthroplasty facilitated by computer software and robotic-arm technology has been introduced to clinical work and welcomed by both orthopaedic surgeons and patients. This evolutionary technique has provided a real sense of patient-specific presurgical planning and extremely precise intraoperative control. Robotic-arm assisted THA has been reported to have higher accuracy in cup positioning, leg length and hip offset control (1), and is associated with improved patient satisfaction and reduced complications (2). Mock surgery can be performed on the 3-dimentional models established by CT images of each patient. The optimal orientation, depth and coverage of the acetabular component can be planned and checked by surgeons with the 3D model. Crucial information such as proper selected femoral component size, estimated leg length and offset of the hip joint compared with ipsilateral and contralateral lower extremity, is also provided by the scan (Figure 1). Further adjustments can be made based on this important information. Specifically, in surgery, procedures like the preparation of the bony interface and installation of the acetabular component, could be highly coordinated with pre-surgery planning. The post-operative management was not differed to the manual total hip arthroplasty.
Operative techniques
Patient selection
Most patients are suitable for MAKO robotic arm-assisted THA. However, patients with large bony defects will cause difficulties in prosthesis installation. Fused hip joints will also cause difficulties in establishing a surgical model. Patients with large periarticular osteophytes will also affect the precision of intraoperative ‘Registration’. These patients should be excluded very carefully.
Workup
Presurgical CT scans of both lower extremities should be acquired. The scanning procedure will be facilitated by MAKO product specialists (MPO). Essential blood tests, cardiac and pulmonary functional tests should also be performed.
Pre-operative preparation
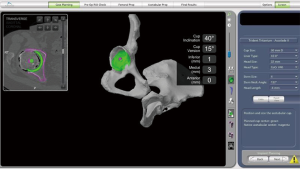
The digital 3D bony models will be established by the manufacturer and imported into the software. The acetabular component should be selected according to the patients’ original size. The orientation and depth of cup should be carefully adjusted. Computer simulated results should be checked on the coronal, sagittal and transverse sections to ensure adequate coverage (Figure 2). Surgeons need to select the most appropriate prosthesis to restore leg length and offset the hip joint as needed. The distance between the neck cutting line to the lesser trochanter should be measured on the software to facilitate determining the neck height for the duration of the surgery.
Equipment preference card
Beyond the instruments set for robotic-arm assisted THA and routine instruments for manual THA, a deep flange thoracic retractor should also be prepared.
Surgical procedure
Before surgery, patients should take the same position as manual surgery according to the surgeon’s preference. The robotic arm should always be placed at the abdominal side of the patient when a lateral position been adopted. An EKG dot should be pasted on the inferior pole of patella and secured by adhesive tape. The entire lower limb of surgical side together with the anterior superior iliac spine (ASIS) should be disinfected. When wrapping the distal part of lower limb, the EKG dot should be wrapped but remain touchable. The ASIS should well exposed when placing the drape.
The base array should first be installed on the ASIS and adjusted carefully to deviate the extended line of incision to avoid shielding of the registration probe during surgery. The fixation must be stable and surgeons should not touch the base array any more than necessary in order to avoid shifting.
After usual exposure, a pin should be fixed on the bony surface of the greater trochanter before the section of joint capsule. Another pin should be installed above the rim of the acetabular component on the bony pelvic but not on the osteophytes at the position of 12 o’clock.
The pins position should be registered afterward, so the joint can be dislocated and the femoral head can be cut. The next acetabular registration procedure can be the most difficult and time-consuming part of this surgery. Surgeons should penetrate the registration pin into the remaining cartilage up to the bony surface of the acetabulum, being cautious to avoid penetrating too deep into an osteoporotic bone. Floating osteophytes should also be avoided to maintain the accuracy of registration.
Once the acetabulum has been registered successfully, it can be reamed by using the same size of reamer as the planned acetabular component. Intraoperative upsize adjustment is also acceptable if the bony interface was not prepared very well. The acetabular component can then be installed with the aid of the robotic arm.
The majority of surgeons worldwide install the femoral component manually. The MAKO system does provide robotic-assisted installation mode, but this mode is too time-consuming.
Role of team members
Typically, only 2 or 3 surgeons should participate in the surgery. Too many operators will occupy the space of the robotic arm and may block the registration probe. One instrument nurse and one itinerate nurse are in charge of instrument and content preparation. One MPO operates software and adjusts the probe detector as needed.
Post-operative management
The rehabilitation procedure of the robotic-arm assisted THA is the same as in manual operation.
Comments
Robotic-arm assisted total hip arthroplasty has significantly improved the accuracy of prosthesis orientation. However, some precautions should also be noted to facilitate the fluency and speed of surgery.
- The base array should not be installed in the direct anterior of the incision line.
- When the right hip has been operated on with lateral position, the robotic arm should be placed close to the table, on the level of the ASIS.
- When the left hip has been operated on with lateral position, the robotic arm should be placed 20 cm distance away from the table, at the rare side of the operator.
- Register the acetabulum on its stable bony surface, being careful to avoid penetrating the cartilage too deeply and steering clear of the floating osteophyte. In this situation, the solid iliac bony surface far above the rim of acetabulum might make a good site for accurate registration.
- The knee should be bent in the same angle (90°) when the registration probe touches the EKG dot placed on the patella surface.
Case demonstration
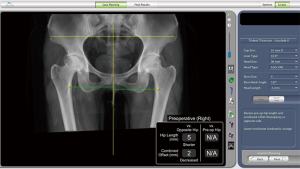
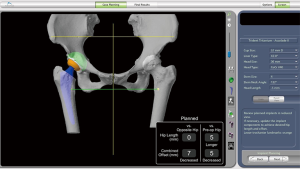
A 55-year-old lady complained about a pain which had bothered her for 10 years, occurring on of both sides of her hip when she walked. The right hip joint pain is much more severe now and she can only walk 50 meters. Plain X-ray of the hip joint showed bilateral acetabular dysplasia and right-side osteonecrosis of the femoral head. A preoperative 3D model showed 5 mm shorter length and 2 mm decreased combined offset of the right-side of the hip joint, when compared to the opposite hip joint (Figure 3).
Preoperative planning could be performed as informed by the 3D model. The size and orientation of the acetabular component was based on the skeletal shape of the patient’s original acetabular. The relative distance between centers of the acetabular component (green colour) and the original acetabulum (purple colour) is shown in Figure 4. Fine adjustment could be made according to the 3-dimensional cross section images (Figure 5). The estimated postoperative effect could be demonstrated directly on the software.

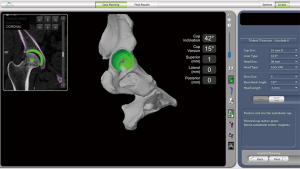
A similar operation could also be performed on the femoral side (Figure 6). However, due to the time-consuming registration procedure on the proximal femur, most surgeons use the software to facilitate the size selection of the femoral component (the express mode).
Once all of the prosthesis was selected, a real time hip length and combined offset change compared to opposite and original hip joint was shown in the lower right frame. Advanced adjustment could be made by selecting the proper head size and head length. (Figure 7) After the pre-surgery plan was finalized, the plan file was exported to a flash disk to be later imported to the MAKO system before surgery.
The surgery was performed according to the procedure mentioned above. Demonstration video record was uploaded (Figure S1).

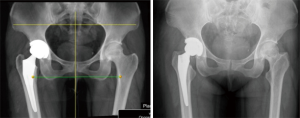
After surgery, a plain film of left hip joint was taken and showed extremely high consistency with the pre-surgical plan (Figure 8).
Acknowledgements
Funding: This work was supported by the Projects of International Cooperation and Exchanges NSFC (81420108021), Key Program of NSFC (81730067), Excellent Young Scholars NSFC (81622033), Jiangsu Provincial Key Medical Center Foundation, Jiangsu Provincial Medical Outstanding Talent Foundation, Jiangsu Provincial Medical Youth Talent Foundation and Jiangsu Provincial Key Medical Talent Foundation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Elson L, Dounchis J, Illgen R, et al. Precision of acetabular cup placement in robotic integrated total hip arthroplasty. Hip Int 2015;25:531-6. [Crossref] [PubMed]
- Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty 2016;31:2353-63. [Crossref] [PubMed]
- Qin J, Xu Z, Dai J, et al. MAKO demonstration surgery. Asvide 2018;5:766. Available online: http://www.asvide.com/article/view/27374
(English Language Editor: John Gray, AME Publishing Company)


