Technical aspects of bedside respiratory monitoring of transpulmonary pressure
Introduction
Transpulmonary pressure corresponds to the pressure distending the lung—i.e., the difference between airway pressure (Paw) and pleural pressure—and is considered one of the most important parameters to know in order to set a safe mechanical ventilation, and to guide therapeutic strategies, above all in acute respiratory distress syndrome (ARDS) patients (1-3). In such complex and heterogeneous pathology, knowing the actual pressure distending the lung tissue may help avoiding lung injury due to lung overdistention or to cyclic opening and closing of alveoli and small airways (3,4). Chest wall mechanics, and therefore pleural pressure, may be impaired not only in ARDS patients but also in critically ill obese patients, in abdominal pathologies or in pathologies affecting the chest wall itself (5). Because of the variability of chest wall mechanics, transpulmonary pressure cannot be inferred by looking only at airways pressure but should rely on the assessment of intrathoracic pleural pressure.
Esophageal pressure (Pes) is considered the best non-invasive surrogate of pleural pressure available at bedside in critically ill patients. Measuring of transpulmonary pressure is one of the possible clinical applications of Pes; it can also be used to assess respiratory efforts in spontaneous breathing patients (for instance to evaluate work of breathing and patient-ventilator asynchronies) or to compute transmural vascular pressure (1,2).
As it is an indirect estimate of pleural pressure, affected by some artifacts (6), concern about the correct interpretation and reliability of results of Pes manometry has been expressed. Probably this is one of the reasons why Pes is rarely used in monitoring the critically ill patient, even recently (7).
The aim of this article is to describe the technique of Pes measurement in mechanically ventilated patients: the catheter insertion, the proper balloon placement and filling, the validation test and specific procedures to remove the main artifacts will be described.
Catheter insertion and proper balloon positioning
Nowadays, several types of esophageal balloons are commercially available. Some balloons are applied on traditional nasogastric feeding tubes; others are not and are carried by a thin dedicated catheter (8). The integrity of the esophageal balloon should always be checked before insertion. A guide-wire is often available in modern esophageal balloon catheters to help the insertion procedure.
After the insertion of the catheter from the nostril, the balloon is driven to the stomach; correct positioning of the catheter can be checked with standard methods: aspiration of gastric content, auscultation or ultrasound visualization during air insufflation (9). The catheter is then inflated with the recommended volume (usually half of the esophageal balloon nominal volume): an intra-gastric position of the balloon can be confirmed by the visualization of positive deflections of balloon pressure during gentle external compressions of the left upper abdominal quadrant. The catheter should then be withdrawn into the mid-lower third of the intrathoracic esophagus. Catheters have depth markers to aid in positioning the balloon: the depth at which the balloon should be placed can be grossly estimated by the distance from nostril to ear tragus to xyphoid. In almost all cases, the correct distance between the nostril and the distal end of the balloon ranges from 35 to 45 cm. If the patient has a spontaneous breathing activity, a negative deflection will appear at the beginning of inspiration on the Pes waveform, as soon as the proximal part of the balloon reaches an intrathoracic position. A sudden change of the baseline value of the balloon pressure may also help detecting the transition from the abdomen to the thorax. Moreover, cardiac artifacts usually appear as the balloon moves to the esophageal portion lying beneath the heart; sometimes heartbeats are already recognizable when the balloon is in the stomach and are magnified when the balloon is pulled back in the esophagus.
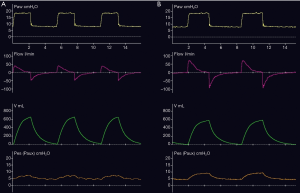
Cardiac artifact may affect Pes waveform by attenuating tidal swings (10). If excessive cardiac oscillations prevent reliable measurements, the catheter should be slightly pulled back and moved to the mid esophagus to effectively reduce the artifacts (Figure 1) (11). Upper esophagus should be avoided because the balloon can be here exposed to tracheal pressure.
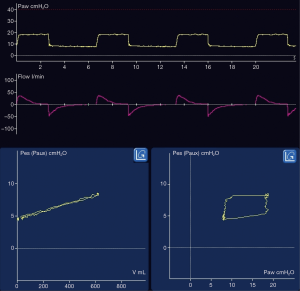
An additional check on correct positioning should be performed looking at waveforms. Chest wall has mainly a linear elastic behavior, thus a linear relationship between volume and pleural pressure is expected. Therefore, if the esophageal balloon is surrounded by the pleural pressure (i.e., it is in the correct position), esophageal balloon pressure and volume curves should be very similar on the ventilator screen; in some ventilators it is possible to visualize the Pes-volume and Pes-Paw loops: Pes-volume relationship should be linear and with no or minimal hysteresis, whereas Pes-Paw loop should be nonlinear with a clear hysteresis due to the resistive pressure in the airways (Figure 2).
Some esophageal catheters have radiopaque markers in order to check correct positioning of the balloon at chest X-ray.
Esophageal balloon catheter filling
Physical characteristics of balloons—i.e., length, diameter, material and compliance—may affect the Pes measurement (12). An in vitro study tested new generation esophageal balloon catheters and provided data about the behavior at different surrounding pressures (8).
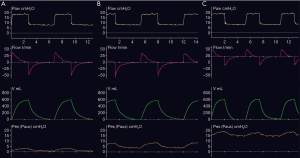
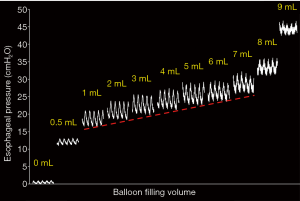
A properly filled balloon transmits the surrounding pressure precisely; an underinflated balloon leads to underestimation, whereas an overinflated-overstretched balloon generates some recoil pressure leading to overestimation of the real value (Figure 3). The range of adequate filling volumes depends on both the physical properties of the esophageal balloon catheter (size and shape of the balloon, inner volume of tube connections) and on the level of the external surrounding pressure (8). Large balloons have wider ranges of adequate filling volumes and are therefore easier to correctly inflate at the bedside. For the same catheter, the adequate filling volumes tend to increase with the progressive rise of the surrounding pressure.
At the bedside, a simple procedure to optimize the esophageal balloon volume is to progressively fill the catheter with steps of 0.5–1.0 mL (lower in case of small balloons with nominal volumes <3 mL) looking at the Pes tracing. After a short period of 5–10 s for pressure stabilization (longer in case the balloon filling elicits some swallowing in the patient), the cyclic tidal swing of Pes should be measured and marked. The optimal filling volume is the lowest volume associated with the largest tidal swing of Pes during mechanical ventilation with constant tidal volumes (13). In case of a spontaneous breathing patient under assisted mechanical ventilation, a brief sedation may be required to reduce strength and variability of respiratory muscles’ activity. Balloon overfilling should always be avoided, thus balloon filling is to be stopped as soon as a sudden and important increase of the baseline pressure (>3–5 cmH2O) is detected while approaching the nominal volume of the balloon. Optimal filling volume should be checked periodically, at least whenever the intrathoracic pressure is likely to be significantly changed because of different PEEP setting, patient position, intra-abdominal pressure, etc.
The esophageal balloon catheter is usually connected by a three-way stopcock with a syringe and a tube line connected to the auxiliary port of the ventilator (or to a pressure monitoring system). Before starting the filling of the catheter, in order to be sure that the balloon will be inflated at the desired volume, it is mandatory to completely remove the volume of air that is eventually in the system. During the deflation of the balloon with the syringe, a negative pressure on the Pes tracing will assure that the balloon is completely deflated; at this point, a brief de-connection of the syringe will allow equilibration of the system with ambient pressure, to avoid a negative and highly variable pressure in the catheter, precluding a precise control of the balloon volume at the next inflation. In case of spontaneous breathing patients, syringe de-connection should be performed during the expiratory phase, eventually asking the patient an active and prolonged expiration. Finally, to pre-distend the balloon and avoid folds, a volume close to its nominal volume should be injected in the catheter and then the balloon deflated to the desired level. Because esophageal balloons tend to slowly but progressively deflate, a periodic refilling is suggested; this is mandatory at each assessment of respiratory mechanics.
Validation tests for the Pes measurements
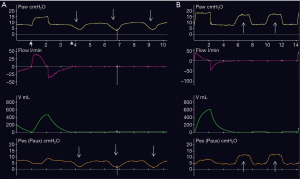
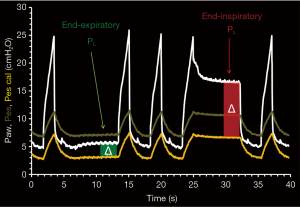
Once the esophageal balloon is properly placed in the mid-lower third of the esophagus and it is optimally filled, a validation test should be performed (14). This test is traditionally considered to control the correct placement of the balloon, but it actually aims at checking the transmission of the changes of intrathoracic pressure to the esophageal balloon. It can be performed both in active and in passive patients. An occlusion maneuver is started at end-expiration, to impede changes of the volume of the respiratory system during the test. In this condition, any change in intrathoracic pressure should be fully transmitted to airways. Thus, in case of a properly placed and filled catheter, Pes changes (ΔPes) are expected to be equal to Paw changes (ΔPaw) during spontaneous efforts of an active patient or alternatively during gentle chest compressions in a passive one (Figure 4). The test is passed if the ΔPes/ΔPaw ratio ranges from 0.9 to 1.1. If not, balloon filling and balloon positioning should be rechecked, in this order. The presence of esophageal balloon leaks is suggested by an unstable baseline level of Pes, slightly decreasing at each breath: the catheter should be removed and replaced in this case. As already stated, excessive heart noise may impede full transmission of intrathoracic pressure swings: a more proximal placement of the balloon in the mid-esophagus may solve this problem.
Calibration procedure for absolute values of Pes
A debate exists whether the absolute value of Pes is a reliable surrogate for absolute pleural pressure or we should rely on Pes variations only. In rest conditions (i.e., no swallowing) the lumen of the esophagus is virtual and its wall is flaccid. In the portion where the esophagus is in touch with the pleura, the pressure inside its lumen should therefore be equal to the intrathoracic one. To measure intra-luminal pressure, an air-filled balloon is placed in the mid-lower esophagus and connected to a pressure transducer. In such a system, two main factors may spuriously increase the absolute level of the pressure: the elastic recoil of the balloon and the esophageal elastance. As opposed to a properly filled one, an overstretched esophageal balloon can generate high recoil pressure; respiratory swings of Pes are usually attenuated in this case (Figure 3). Balloon overfilling can be easily avoided by checking the baseline pressure when the catheter is progressively inflated (Figures 3,5). The “esophageal elastance” corresponds to the reaction of the esophagus to an inflated balloon distending its wall (13). Actually, it is both a passive (recoil due to elastic and collagen fibers) and an active (tonic contraction of smooth muscles) phenomenon (15). To eliminate this artifact, the strategy originally proposed in the 1960s and adopted for many years was to use very low filling volumes. However, it was demonstrated that during positive-pressure mechanical ventilation very low filling volumes may be insufficient to accurately transmit both absolute values and tidal swings of Pes, thus higher filling volumes are now recommended in this setting (1,2,8,13). As a result, disproportionately high Pes values are often recorded, thus raising major concerns about the reliability of absolute values (16). An alternative approach based on the respiratory changes of Pes was therefore proposed to compute transpulmonary pressure (16,17). As expected being based on different assumptions, the direct “absolute” method and the indirect “elastance-derived” method actually give inconsistent results (16,18). This unsolved debate on Pes measurement and interpretation is probably the main reason why such a fundamental monitoring is not widely use in the clinical practice.
A calibration procedure was recently described (13) to solve both the issue of low Pes transmission due to insufficient balloon filling, and Pes overestimation due to the pressure generated by the esophageal wall as a reaction to balloon filling. This calibration can be performed contextually to the already described procedure to optimize balloon filling by progressive step inflation. Briefly, an esophageal balloon P-V curve (where P is the end-expiratory Pes and V is the filling volume) is obtained and its intermediate linear portion detected (Figure 5). This portion of the curve corresponds to the range of grossly adequate balloon filling volumes: with lower values the balloon is clearly underfilled and compressed by the surrounding pressure, whereas with higher values it is clearly overstretched. For a finer adjustment of balloon inflation within this range, the optimal filling volume can be selected as the smallest one associated with the largest tidal swing of Pes, as previously described. Finally, the slope of the linear portion of the balloon P-V curve corresponds to the esophageal elastance and can be used to deduct the esophageal artifact (i.e., the pressure generated by the esophagus wall) associated to the optimal filling volume. This procedure was applied in acute respiratory failure patients under invasive mechanical ventilation, thus suggesting that it is feasible to get a reliable estimate of the absolute value of pleural pressure in this setting (13). Accordingly, it was recently demonstrated that when esophageal elastance is taken into account, Pes reflects the absolute value of the intrathoracic pressure surrounding the balloon, corresponding to mid-level of the chest, intermediate between non-dependent and dependent lung regions (19). Therefore, the dilemma between the two current and opposed approaches, based on absolute values or alternatively on respiratory variations of Pes, could be hopefully solved by the use of a third approach, based on absolute calibrated Pes values (Figure 6).
Being the original calibration procedure quite complex and time consuming, it is mainly indicated for research purposes. A simplified procedure has been proposed (20) to obtain an acceptable estimate of the absolute pleural pressure at the bedside; however, an automatic procedure implemented in dedicated monitoring systems or in mechanical ventilators will probably be the ultimate solution (2).
Conclusions
An advanced respiratory monitoring of the acute respiratory failure patient is recommended every time there is the risk of an injurious (spontaneous, assisted or controlled) ventilation. Measurement of transpulmonary pressure can provide useful information on both inspiratory stress and expiratory risk of de-recruitment, thus helping the management of these patients. However, such a meaningful monitoring is not widely used in clinical practice mainly due to technical issues and concerns about reliability of the Pes measurements. Recent findings suggest that a systematic approach based on optimal placement and filling of the esophageal balloon, removal of the main artifacts and periodic check of the correct functioning makes this monitoring tool reliable. To make it more attractive and feasible in everyday clinical practice, an automated management of the esophageal balloon catheter by means of mechanical ventilators or dedicated monitoring systems is probably needed.
Acknowledgements
None.
Footnote
Conflicts of Interest: F Mojoli was involved in a university research spin-off for the development of NutriVent. The other authors have no conflicts of interest to declare.
References
- Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014;189:520-31. [Crossref] [PubMed]
- Mauri T, Yoshida T, Bellani G, et al. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med 2016;42:1360-73. [Crossref] [PubMed]
- Talmor D, Sarge T, Malhotra A. el al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095-104. [Crossref] [PubMed]
- Gattinoni L, Chiumello D, Carlesso E, et al. Bench-to-bedside review: Chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Critical Care 2004;8:350-5. [Crossref] [PubMed]
- Talmor D, Sarge T, O’Donnell CR, et al. Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med 2006;34:1389-94. [Crossref] [PubMed]
- Hedenstierna G. Esophageal pressure: benefit and limitations. Minerva Anestesiol 2012;78:959-66. [PubMed]
- Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016;315:788-800. [Crossref] [PubMed]
- Mojoli F, Chiumello D, Pozzi M, et al. Esophageal pressure measurements under different conditions of intrathoracic pressure. An in vitro study of second generation balloon catheters. Minerva Anestesiol 2015;81:855-64. [PubMed]
- Vigneau C, Baudel JL, Guidet B, et al. Sonography as an alternative to radiography for nasogastric feeding tube location. Intensive Care Med 2005;31:1570-2. [Crossref] [PubMed]
- Mead J, Gaensler EA. Esophageal and pleural pressures in man, upright and supine. J Appl Physiol 1959;14:81-3. [Crossref] [PubMed]
- Milic-Emili J, Mead J, Turner JM. Topography of esophageal pressure as a function of posture in man. J Appl Physiol 1964;19:212-6. [Crossref] [PubMed]
- Mead J, McIlroy MB, Selverstone NJ. el al. Measurement of intraesophageal pressure. J Appl Physiol 1955;7:491-5. [Crossref] [PubMed]
- Mojoli F, Iotti GA, Torriglia F, et al. In vivo calibration of esophageal pressure in the mechanically ventilated patient makes measurements reliable. Crit Care 2016;20:98. [Crossref] [PubMed]
- Baydur A, Behrakis PK, Zin WA, et al. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis 1982;126:788-91. [PubMed]
- Orvar KB, Gregersen H, Christensen J. Biomechanical characteristics of the human esophagus. Dig Dis Sci 1993;38:197-205. [Crossref] [PubMed]
- Chiumello D, Cressoni M, Colombo A, et al. The assessment of transpulmonary pressure in mechanically ventilated ARDS patients. Intensive Care Med 2014;40:1670-8. [Crossref] [PubMed]
- Chiumello D, Carlesso E, Cadringher P, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med 2008;178:346-55. [Crossref] [PubMed]
- Gulati G, Novero A, Loring SH, et al. Pleural pressure and optimal positive end-expiratory pressure based on esophageal pressure versus chest wall elastance: incompatible results. Crit Care Med 2013;41:1951-57. [Crossref] [PubMed]
- Yoshida T, Amato MBP, Grieco DL, et al. Esophageal manometry and regional transpulmonary pressure in lung injury. Am J Respir Crit Care Med 2018;197:1018-26. [Crossref] [PubMed]
- Mojoli F, Torriglia F, Giannantonio M, et al. In vivo calibration of the esophageal balloon catheter: a simplified procedure. Intensive Care Med Experimental 2016;4:534.


