
Not all primary total hip arthroplasties are equal—so is there a difference in reimbursement?
Introduction
Relative value units (RVUs) were first implemented in 1992 based on a 1988 Harvard study by Hsiao et al. (1) as part of the resource-based relative value system (RVBRS) to determine physician compensation. The study was commissioned by the federal government in response to concerns regarding Medicare spending and low reimbursement in primary care (2). The reimbursement model originally proposed by Hsaio et al. (1) described three factors that should determine physician compensation: (I) time or work associated with providing a service, (II) cost of operating a practice, and (III) the opportunity cost of physician training (1-3). On average, the physician work component (work RVU) represents about half of the total RVU (2) and is intended to be proportional to physician time, effort, and technical skill in providing the service; and therefore, appropriately reflect physician reimbursement (2,4,5).
Multiple factors are used to determine reimbursement within the RVU model. For instance, the given RVU for a service provided is multiplied by a set dollar amount as well as other factors such as geographic practics costs like regional wage variations, costs of living, and malpractice premiums (6). Hence the RVU designation determines the Medicare fee for service. Some potential flaws with the RVU-based compensation system have, however, been identified. For example, studies suggest that cognitive care continues to be undervalued relative to surgical procedures (7,8). Additionally, although the RVBRS intention was to provide higher compensation for the physician services that require more work, there is limited evidence of this in the literature. Furthermore, while a few studies have found a correlation between measures of physician effort and RVUs (9,10), many others have challenged the model (11-13).
Few studies have assessed the ability of RVU-based reimbursement to accurately reflect procedural complexity in different fields of medicine (6,14) with limited data regarding the RVU model performance in orthopedics. In fact, to the best of our knowledge, there are no studies analyzing the use of the RVU model with respect to various types of hip arthroplasty, specifically conversion hip arthroplasty [conversion of a previous hip surgery to THA, with or without autograft or allograft (15)]. Therefore, the purpose of this study was to determine whether RVUs adequately capture the complexity, technical skill, and aftercare in primary versus conversion THA. Specifically, we compared: (I) mean operative times; (II) mean RVUs; (III) RVU per unit of time between primary and conversion THAs; and (IV) performed an individualized surgeon annual cost difference analysis.
Methods
Database
The American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) database was used to identify patients who underwent primary and conversion THA between 2008 and 2015. The ACS-NSQIP is a nationally validated database that collects preoperative through 30-day postoperative data based on 135 variables for hundreds-of-thousands of cases (16). Data is collected at each contributing hospital by trained surgical clinical reviewers who are audited annually to ensure accuracy (16). This study was exempted from review by the Institutional Review Board as the database is publically available and contains de-identified data.
Current Procedural Terminology (CPT) codes
CPT codes, maintained by the American Medical Association, represent discrete physician services and are used as universal identifiers in order to determine reimbursement across all payers. We used category 1 CPT codes which directly link to procedures or services performed. Category 2 CPT codes are used for supplemental tracking and are optional, while category 3 CPT codes are provisional codes for new technologies, procedures, or services (17). For this study, CPT 27130 was used to identify primary THA, while CPT 27132 was used to identify conversion THA.
THA procedure selection
Primary and conversion hip arthroplasty were chosen for this study, since hip arthroplasties make up a large part of the overall expenditure of CMS (18). In fact, some estimates report CMS programs to pay for roughly 65% of all hip replacements in the United States, totaling nearly $40 billion (19). Furthermore, because conversion THA is the first time a prosthesis is implanted in a patient, it can fall under the realm of a primary case. However, recent reports have found that compared to primary THAs, conversion THAs require more intra- and post-operative resources, and are more similar to a revision THAs than primary THAs (20-22). Therefore, it is important to make the distinction between primary and conversion total hip arthroplasties both operatively and financially.
Primary THA patient selection
Using CPT code 27130, a total of 104,209 primary THA cases were identified from the NSQIP database. Of this total number of cases, 441 (0.4%) cases which had recorded operative times of less than 30 minutes were excluded (very unlikely value, most likely a data entry error), yielding 103,768 (99.6%). Sixty-six cases (0.06%) out of the 103,768 cases that had a recorded operative time greater than 480 minutes were also excluded (also, outliers values, most likely due to inaccuracy in data entry). This resulted in a total of 103,702 primary THA cases, with operative times between 30 to 480 minutes that were included for final analysis in the current study. Women made up 57,451 (55%) of cases, while men made up 46,172 (45%) of cases. Seventy-nine cases (0.08%) did not have gender recorded.
Conversion THA cases
CPT 27132 was used to identify 3,004 conversion THA cases. Conversion THA was defined as: conversion of a previous hip surgery to THA, with or without autograft or allograft (15). Of the 3,004 cases, 11 cases (0.4%) had operative times recorded as less than 30 minutes and were excluded from analysis. Of the remaining 2,993 cases, 7 cases (0.2%) had operative times greater than 480 minutes, and were also excluded from the analysis. This resulted in 2,986 conversion THA cases with operative times between 30 and 480 minutes, which were included in the analysis. Of the 2,986 cases, 1,656 (55%) were women, while 1,330 (45%) were men.
Annual cost difference analysis
An annualized cost difference analysis was performed at an individual surgeon level performing primary or conversion THAs. We used 8 hours of operative time per day and an estimated 160 operative days per year (365 days/year, less 104 weekend days, less 14 days for vacation, less 5 federal holidays, less 1/3 of remaining days for non-operative days). Based on the mean operative times found, in 1 day a surgeon could either complete 5 primary THA or 3 revision THAs in one operating room. The Centers for Medicare and Medicaid Services reports an RVU conversion factor of $35.8887/RVU. The RVU/minute for each cohort was calculated by dividing the RVU assigned to each case by the operative time, in minutes, for that particular case. From the RVU conversion factor and the RVU/minute, a dollar amount per minute for both primary and conversion total hip arthroplasties was calculated. Dollar amounts per case were calculated by multiplying the dollar amount per minute and mean operative time. A daily reimbursement was calculated by multiplying the per-case reimbursement by the number of cases completed each day (5 primary or 3 conversion). From these values, a daily reimbursement difference was calculated and multiplied by 160 operative days, resulting in the annual dollar amount difference an adult reconstructive surgeon can be reimbursed for only performing primary THAs.
RVUs analysis
Work RVUs were identified from the NSQIP database using the variable name “WORKRVU.” RVUs were defined as work RVUs in this study. Because congress requires CMS to continuously update the RVU system no less than every 5 years, the same CPT code can have different RVUs assigned to it for different years. During the review, CMS can update any RVUs assigned to a procedure if it is determined to be incorrectly valued. In order for the updates to occur, The American Medical Association/Specialty Society Relative Value Scale Update Committee (RUC) compares surveys sent to physicians in the field, focusing on their time, effort, and practice expenses for providing particular procedures or services, to reference services in order to create new RVU recommendations. Based on these recommendations, CMS can then choose to update RVUs. In 2014, 76% of RUC recommendations were accepted by CMS (23).
Operative time analysis
Operative times were identified from the NSQIP database using variable name “OPTIME”. Operative times that were recorded to be less than 30 minutes or greater than 480 minutes were not included for analysis. We felt these data points were potential errors in data collection, as some of these cases had negative or zero recorded operative times. Only a few cases (approximately 0.5%) were excluded. Nevertheless, the up-to-date and accurate NSQIP database, and over 100,000 cases were used for analysis.
Data analysis
Mean RVUs, mean operative times, and RVU/minute were calculated using a Microsoft Excel spreadsheet (2013 Microsoft Office Professional Plus; Redmond, WA). These values were then compared between primary and revision THA cohorts. A cutoff P value of <0.05 was set to determine statistical significance of results. All Statistical analyses were performed using SPSS version 24 (International Business Machine Corporation, Armonk, New York, USA).
Results
Mean operative times
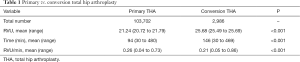
The mean operative times were 94 minutes (range, 30 to 480 minutes) for primary THA, and 146 minutes for conversion THA (range, 30 to 469 minutes). The mean operative times for primary THA were significantly lower than conversion THA (P<0.001) (Table 1).
Full table
Mean RVUs
The mean RVUs for the primary THA cases were 21.24 (range, 20.72 to 21.79). The mean RVUs for the conversion THA cases were 25.68 (range, 25.49 to 25.69). The 21.24 mean RVUs for primary THA were found to be significantly lower than the 25.68 mean RVUs for conversion THA cases (P<0.001) (Table 1).
Mean RVU/minute
The mean RVU/minute for the primary THA cases was 0.26 (range, 0.04 to 0.73), while the mean RVU/minute for the conversion THA cases was 0.21 (range, 0.05 to 0.86). The 0.26 mean RVU/minute for primary THA cases was found to be significantly greater than the 0.21 RVU/minute for conversion THA cases (P<0.001) (Table 1).
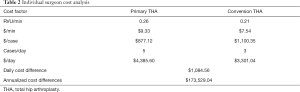
Annual cost difference analysis
The reimbursement rate for primary THA was found to be $9.33 per minute (0.26 RVU/minute × $35.8887/RVU), while for conversion THA, it was found to be $7.54 (0.21 RVU/minute × $35.8887/RVU). Each primary THA was found to be reimbursed at $877.12 per case, yielding a daily net of $4,385.60 for performing 5 primary THAs in 8 hours. Conversion THAs are reimbursed at $1,100.35 per case, or $3,301.04 per day for performing 3 conversions cases. The daily difference for performing primary vs. conversion cases amounts to $1,084.56. Thus, the annualized cost difference for an individual surgeon performing primary THAs instead of conversion THAs is $173,529.04 (Table 2).
Full table
Discussion
The Health Care Financing Administration (now CMS) implemented the RVBRS in 1992 in response to concerns for the increasing health care spending and low reimbursement for cognitive clinical encounters (1,2). The physician work component of the RVU is maintained by panels of physician societies and intends to allocate reimbursement that is in accordance with the time, physical and mental effort, psychological stress, and technical skill necessary to provide the service (1-3,6). It, therefore, follows that physicians should receive a higher rate of compensation for more complex procedures. There is evidence that conversion THA is a relatively frequent procedure that has longer operative times, more intraoperative blood loss, longer lengths of hospital stay, and higher costs than primary THA (24-27). Surgeons should therefore receive a higher rate of compensation for conversion THA. In the present study, we found that this is not necessarily the case. Although mean RVUs were higher for conversion than primary THAs the mean operative times for conversion THA were also higher. Therefore, when correcting the RVUs for the time spent in surgery, the mean RVU/minute for primary THA was higher than for conversion THA (0.26 vs. 0.21, P<0.001). These data show that surgeons can earn a higher rate of reimbursement, and potentially almost $200,000 annualized difference, by preferentially performing primary THAs rather than the more complex conversion THAs. The main driving forces to such a large reimbursement differences are both the reimbursement rate as well as the number of cases which can be performed in a single day.
Like this study, others have shown evidence that RVUs do not correlate well with measures of physician work. Schwartz et al. (11) used the NSQIP database to show that emergent colectomy, total hernia repair, and biliary procedures were associated with significantly higher mortality risk, longer lengths of stay, and rate of complication than the corresponding elective procedures, despite their identical RVU designations. Similarly, Shah et al. (12) found that RVUs were poorly correlated with operative time, lengths of stay, and mortality. A study by Balasubramanian et al. (28) showed that work RVUs were poorly correlated with complexity of diagnosis and interpretation time in pediatric echocardiography. Additionally, Resnick et al. (13) demonstrated significant discrepancies between RVUs and hospital revenue generated between surgical specialties, which indicates that surgeons in some fields are not compensated in accordance with their value to the hospital.
Nguyen et al. (9) used the NSQIP database to show that that RVUs were correlated with overall complications and surgical site complications in plastic surgery procedures. However, their study included patients undergoing multiple concomitant procedures, making the results difficult to generalize to orthopaedics. In addition, it was not clear that the rate of complications alone was a sufficient measure of physician work. Another study by Little et al. (10) found that RVUs were correlated with operative time in pediatric surgical procedures. However, the study only included outpatient procedures and those that required less than one inpatient day of surgeon follow-up. The results are thus difficult to generalize to other, more complex procedures and those performed on adult populations.
There were several limitations to this study. Due to the retrospective nature and design, we were limited to data that was collected previously. There may be some unavoidable selection bias associated with the NSQIP database, as not all cases are included in it. Nonetheless, the NSQIP database contains prospectively collected data from a wide range of surgical centers, which improves its generalizability. Additionally, operative times less than 30 minutes or greater than 480 minutes operative times were excluded in our analysis. However, these were only a very few number of cases (approximately 0.5%), and were likely incorrectly coded. In addition, the NSQIP database does not account for variation in technical skill or work performed outside of the operating room, such as aftercare and clinic visits during the 90-day post-operative window. These are also important factors, which when considered, would likely further increase the RVU/minute discrepancy as conversion THAs tend to require greater overall care than primary THAs. Nevertheless, these factors should still be included for analysis in future studies.
While THA is a common treatment for end stage hip osteoarthritis, it is also often performed to treat failures or complications related to existing hardware due to previous fracture fixation or osteotomies (24,29,30). Numerous studies have found evidence that conversion THAs are a more complex procedure than primary THAs, and requires more physician work (31). Schwarzkopf et al. (25) found that, compared to primary THA, conversion THA had a significantly longer operative time and hospital stay (P<0.05). Additionally, conversion THA increased the likelihood of requiring revision-type components, and the likelihood of requiring metaphyseal/diaphyseal fixation. Chin et al. (26) demonstrated that conversion THA had several significantly higher cost variables than primary THA, including a 29.2% higher cost associated with services provided by healthcare providers. In addition, Newman et al. (27) demonstrated that conversion THA resulted in increased perioperative blood loss and transfusion requirement. The RVU model was designed to reflect physician time, work, costs and the opportunity costs of training. However, while conversion THA has been shown to be more technically demanding with increased patient risk, it does not appear to be reflected in per minute compensation.
Conclusions
Published RVUs indicate that higher physician reimbursement is assigned for conversion THA than for the less complex primary THA. However, our data show that the actual increase in RVUs did not offset the increased time requirement of conversion THA. The mean RVU/minute of primary THA was significantly greater than that of conversion THA (0.26 vs. 0.21, P<0.001) and the cost analysis reviled a potential $173,529 difference. These data challenge the actual RVU model, and potentially prompt for a review of relative-value based compensation of orthopaedic surgeons. Although RVUs were designed with the intention of providing appropriate and proportional compensation to a physician work and skill, this study showed that an orthopaedic surgeon would potentially receive a higher hourly reimbursement by selectively performing primary THA over more complex and demanding conversion THA.
Acknowledgements
None.
Footnote
Conflicts of Interest: M Chughtai: Cymedica; DJ Orthopaedics; Peerwell; Performance Dynamics Inc.; Refelection; Sage Products; Stryker. MA Mont: AAOS; Abbott; Cymedica; DJ Orthopaedics; Johnson & Johnson; Journal of Arthroplasty; Journal of Knee Surgery; Mallinckrodt Pharmaceuticals; Microport; National Institutes of Health (NIAMS & NICHD); Ongoing Care Solutions; Orthopedics; Orthosensor; Pacira; Peerwell; Performance Dynamics Inc.; Sage; Stryker; Surgical Technologies International; Kolon TissueGene. The other authors have no conflicts of interest to declare.
Ethical Statement: This study was exempted from review by the Institutional Review Board as the database is publically available and contains de-identified data.
References
- Hsiao WC, Braun P, Dunn D, Becker ER. Resource-based relative values. An overview. JAMA 1988;260:2347-53. [Crossref] [PubMed]
- Laugesen MJ. The resource-based relative value scale and physician reimbursement policy. Chest 2014;146:1413-9. [Crossref] [PubMed]
- Hsiao WC, Braun P, Dunn DL, et al. An overview of the development and refinement of the Resource-Based Relative Value Scale. The foundation for reform of U.S. physician payment. Med Care 1992;30:NS1. [PubMed]
- Maxwell S, Zuckerman S. Impact of Resource-Based Practice Expenses on the Medicare Physician Volume. Health Care Financ Rev. Health Care Financ Rev 2007-2008;29:65-79. [PubMed]
- Centers for Medicare & Medicaid Services (CMS). HHS. Medicare Program; Revisions to Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B for CY 2017; Medicare Advantage Bid Pricing Data Release; Medicare Advantage and Part D Medical Loss Ratio Data Release; Medicare Advantage Provider Network Requirements; Expansion of Medicare Diabetes Prevention Program Model; Medicare Shared Savings Program Requirements. Final rule. Fed Regist 2016;81:80170-562. [PubMed]
- Baadh A, Peterkin Y, Wegener M, et al. The Relative Value Unit: History, Current Use, and Controversies. Curr Probl Diagn Radiol 2016;45:128-32. [Crossref] [PubMed]
- Katz S, Melmed G. How Relative Value Units Undervalue the Cognitive Physician Visit: A Focus on Inflammatory Bowel Disease. Gastroenterol Hepatol (N Y) 2016;12:240-4. [PubMed]
- Sinsky CA, Dugdale DC. Medicare payment for cognitive vs procedural care: minding the gap. JAMA Intern Med 2013;173:1733-7. [PubMed]
- Nguyen KT, Gart MS, Smetona JT, et al. The relationship between relative value units and outcomes: a multivariate analysis of plastic surgery procedures. Eplasty 2012;12:e60. [PubMed]
- Little DC, St Peter SD, Calkins CM, et al. Relative value units correlate with pediatric surgeons’ operating time: when perceived myth becomes reality. J Pediatr Surg 2006;41:234-8. [Crossref] [PubMed]
- Schwartz DA, Hui X, Velopulos CG, et al. Does relative value unit-based compensation shortchange the acute care surgeon? J Trauma Acute Care Surg 2014;76:84-92; discussion 92-4. [Crossref] [PubMed]
- Shah DR, Bold RJ, Yang AD, et al. Relative value units poorly correlate with measures of surgical effort and complexity. J Surg Res 2014;190:465-70. [Crossref] [PubMed]
- Resnick AS, Corrigan D, Mullen JL, et al. Surgeon contribution to hospital bottom line: not all are created equal. Ann Surg 2005;242:530-7; discussion 537-9. [PubMed]
- Lorio M, Martinson M, Ferrara L. Paired Comparison Survey Analyses Utilizing Rasch Methodology of the Relative Difficulty and Estimated Work Relative Value Units of CPT(R) Code 27279. Int J Spine Surg 2016;10:40. [Crossref] [PubMed]
- Case Log Guidelines for Adult Reconstructive Orthopaedic Surgery Review Committee for Orthopaedic Surgery. Available online: https://www.acgme.org/Portals/0/PFAssets/ProgramResources/261_CaseLogGuidelines_AdultReconstructiveOrthopaedicSurgery.pdf
- Fuchshuber PR, Greif W, Tidwell CR, et al. The power of the National Surgical Quality Improvement Program--achieving a zero pneumonia rate in general surgery patients. Perm J 2012;16:39-45. [Crossref] [PubMed]
- CPT - Current Procedural Terminology Codes - AAPC. Available online: https://www.aapc.com/resources/medical-coding/cpt.aspx
- Bumpass DB, Nunley RM. Assessing the value of a total joint replacement. Curr Rev Musculoskelet Med 2012;5:274-82. [Crossref] [PubMed]
- Lavernia CJ, Villa JM. Rapid recovery programs in arthroplasty: the money side. J Arthroplasty 2015;30:533-4. [Crossref] [PubMed]
- Schwarzkopf R, Baghoolizadeh M. Conversion total hip arthroplasty: Primary or revision total hip arthroplasty. World J Orthop 2015;6:750-3. [Crossref] [PubMed]
- Panagiotopoulos KP, Robbins GM, Masri BA, et al. Conversion of hip arthrodesis to total hip arthroplasty. Instr Course Lect 2001;50:297-305. [PubMed]
- Schuh A, Zeiler G, Werber S. Results and experiences of conversion of hip arthrodesis. Orthopade 2005;34:218-220-4. [Crossref] [PubMed]
- Coberly S. Relative Value Units (RVUs). Washington, 2015. Available online: https://www.nhpf.org/library/the-basics/Basics_RVUs_01-12-15.pdf
- Oñativia IJ, Slulittel PAI, Diaz Dilernia F, et al. Outcomes of nondisplaced intracapsular femoral neck fractures with internal screw fixation in elderly patients: a systematic review. Hip Int 2018;28:18-28. [Crossref] [PubMed]
- Schwarzkopf R, Chin G, Kim K, et al. Do Conversion Total Hip Arthroplasty Yield Comparable Results to Primary Total Hip Arthroplasty? J Arthroplasty 2017;32:862-71. [Crossref] [PubMed]
- Chin G, Wright DJ, Snir N, et al. Primary vs Conversion Total Hip Arthroplasty: A Cost Analysis. J Arthroplasty 2016;31:362-7. [Crossref] [PubMed]
- Newman JM, Webb MR, Klika AK, et al. Quantifying Blood Loss and Transfusion Risk After Primary vs Conversion Total Hip Arthroplasty. J Arthroplasty 2017;32:1902-9. [Crossref] [PubMed]
- Balasubramanian S, Kipps AK, Smith SN, et al. Pediatric Echocardiography by Work Relative Value Units: Is Study Complexity Adequately Captured? J Am Soc Echocardiogr 2016;29:1084-91. [Crossref] [PubMed]
- Zhang B, Chiu KY, Wang M. Hip arthroplasty for failed internal fixation of intertrochanteric fractures. J Arthroplasty 2004;19:329-33. [Crossref] [PubMed]
- Haidukewych GJ, Berry DJ. Hip arthroplasty for salvage of failed treatment of intertrochanteric hip fractures. J Bone Joint Surg Am 2003;85-A:899-904. [Crossref] [PubMed]
- Kreitz TM, Deirmengian CA, Penny GS, et al. A Current Procedural Terminology Code for "Knee Conversion" Is Needed to Account for the Additional Surgical Time Required Compared to Total Knee Arthroplasty. J Arthroplasty 2017;32:20-3. [Crossref] [PubMed]


