The clinical value of routinely obtained postoperative chest radiographs in post-anaesthesia care unit patients seems poor—a prospective observational study
Introduction
Postoperative chest radiographs (CXRs) are frequently obtained in post-anaesthesia care unit (PACU) patients (1,2). These CXRs are either obtained routinely, i.e., without a specific reason other than standard care, or because of a change in the clinical condition. It may be helpful in the early recognition of postoperative complications, like pneumothorax, large atelectasis, pulmonary infiltrates or pleural effusions, and malposition of invasive devices such as central venous catheters (3-5) gastric and chest tubes (2), and/or endotracheal tubes if mechanical ventilation is continued after surgery. CXRs have high diagnostic accuracy for detecting these abnormalities (6,7).
Obtaining a CXR in postoperative patients, however, could cause discomfort and may even cause harm, e.g., through accidental malpositioning of central venous lines and/or tubes. Furthermore, most postoperative abnormalities resolve spontaneously without any specific intervention (8), and endotracheal tubes, if still present on arrival in the PACU are usually removed within hours after arrival in the unit. Finally, most chest tubes are inserted under direct vision by surgeons, and these may not require CXR evaluation. Finally, any routinely performed diagnostic measure carries the risk of getting false-positive or unimportant findings that may be acted upon.
Substantial savings can be achieved by limiting the number of CXRs. Numerous investigations have demonstrated the low diagnostic and treatment impact of routinely obtained CXRs in intensive care unit patients (9-12), and several randomized controlled trials (13-15) and two meta-analyses (16,17) suggest that abandoning routinely obtained CXRs from daily ICU practice is safe. Consequently, the American College of Radiology recommends against routine CXRs (18). We hypothesized that the clinical value of routinely obtained postoperative CXRs in PACU patients is also low. To test this hypothesis, we performed an observational study in the PACU of a university hospital in The Netherlands.
Methods
Ethical approval and informed consent
The Institutional Review Board of the Academic Medical Center, Amsterdam, The Netherlands (Chairwoman Dr. M.D. Trip), reviewed and approved the study protocol and analysis plan, and waived the need for individual patient informed consent seen the observational nature of this study (W12_201 # 12.17.0222; 29 August 2012, correspondence address Academic Medical Center, PO box 1100 DD, Amsterdam, The Netherlands).
Setting
The study was performed in a 22-bed PACU that mainly serves postoperative patients. It was local policy to routinely obtain CXRs in PACU patients that continued to receive invasive mechanical ventilation in the PACU, those that were given a central venous catheter in the peri-operative period, and in patients after thoracic surgery. Half of the beds were equipped with a patient data management system (MetaVision; iMDsoft, Sassenheim, The Netherlands); a written record was kept at the other beds.
Inclusion and exclusion criteria
We included consecutive patients admitted to the PACU in whom a CXR was obtained. Patients in whom a CXR was made on a clinical indication (i.e., when presence of a specific finding needed to be confirmed or denounced) were excluded, as were patients that were admitted because of another reason than postoperative observation.
Endpoints
The primary endpoint was the percentage of CXRs with unexpected predefined new abnormalities, the diagnostic efficacy. The secondary endpoint was the percentage of CXRs with unexpected new abnormalities that led to a predefined change in therapy, the treatment impact.
Collection of radiology data
Data were collected during a 9-month period. In this period, before a CXR could be made by the radiology workers, attending surgeons or PACU physicians had to complete a study-specific data sheet, which was printed on the back of the normal CXR request form. Radiology workers were instructed to obtain CXR only when these data were provided. Collection of data started after a 1-month pilot phase, during which the feasibility of completing the back of the normal CXR request form before making the CXR was tested, and to ensure that surgeons, attending PACU physicians and radiology workers used the forms exclusively and appropriately.
Attending surgeons or PACU physicians had to score whether the CXR was to be considered a ‘routine test’, i.e., whether it was obtained without any specific reason, or whether it was performed ‘non-routinely’, i.e., because of a specific clinical reason, and other than the surgical procedures. Surgeons or PACU physicians then ticked whether an expected predefined abnormality was ‘already known’, i.e., known from preceding CXRs, or ‘newly expected’. Independent responsible chest radiologists read CXRs on the day it was obtained, and also had to tick whether a predefined abnormality was ‘already known’ or ‘new’. Of note, in case an already known abnormality had worsened, then the radiologist had to score it as ‘new’.
Independent observers determined whether an action was taken in response to findings on the routinely obtained CXRs. These observers were not involved in daily PACU care, and attending surgeons and PACU physicians were not aware of this part of the study. The observers read the medical records, checked the patient data management system and searched the hospital information system for the following information: orders for sputum cultures, or start of or a change in antimicrobial therapy in cases of pneumonia; repositioning of tubes and central venous catheters in cases of malposition of indwelling devices; the performance of a chest ultrasound studies in cases of pleural effusions, the start or change in medication, in particular diuretic drugs, and insertions of pleural drains.
Predefined abnormalities
The predefined abnormalities were similar as those used previously in studies in intensive care unit patients (9,19,20) and are summarized in Table 1.

Full table
Definitions
We used the following definitions for expected and/or found predefined abnormalities:
- New, expected but not found—a new abnormality that was expected by the attending physician but that was not found by the radiologist;
- New, expected and found—a new abnormality that was expected by the attending physician, and that indeed was found by the radiologist;
- New, not expected but found—a new abnormality that was not expected by the attending physician but that was found by the radiologist.
We used the following definitions for diagnostic efficacy and therapeutic efficacy:
- Diagnostic efficacy—the percentage of CXRs with one or more new predefined abnormalities;
- Therapeutic impact—the percentage of CXRs that resulted in a change in clinical management.
For the purpose of this study we defined efficacy <10% as poor, 10–50% as fair, 50–90% as good, and >90% as excellent.
Study duration
Previous investigations showed that ~10% of routine CXRs reveal unexpected findings, and ~5% of causing a change in patient management (9). We wanted an absolute minimum of unexpected findings of 50 or 25 findings resulting in a treatment impact. Based on the experience that at least 55 CXRs per month were obtained in the PACU, we decided to run the study for 9 months.
Statistical analysis
CXRs with incomplete data sheets were excluded from the analysis, as were the follow-up CXRs obtained during one single PACU admission. All data were entered in a computerized database (Microsoft Access 2003; Microsoft Inc., Richmond, WA, USA). Patient and clinical characteristics were summarized using descriptive statistics.
Results
Patients and CXRs
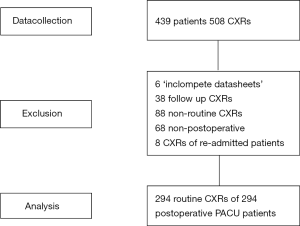
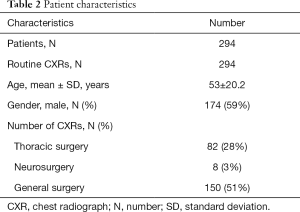
Figure 1 shows a CONSORT diagram. Baseline characteristics of the patients are shown in Table 2. In total, 508 CXRs were obtained during 439 PACU admissions (27 patients were admitted more than once). After exclusion of CXRs obtained because of a reported clinical indication, CXRs that were obtained in patients admitted to the unit for reasons other than postoperative observation, and CXRs obtained during repeated PACU admissions, we were left with 294 routine CXRs from 294 patients in the final analysis.
Full table
CXR, chest radiograph; N, number; SD, standard deviation.
New and expected abnormalities
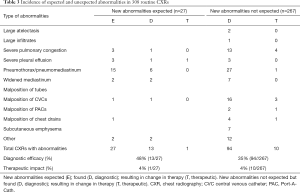
In 27 out of the 294 routinely obtained CXRs a new abnormality was expected, which was actually found in 13 CXRs (Table 3): 16 expected abnormalities (8 found) after thoracic surgery (82 CXRs), 0 expected abnormalities in patients who continued with invasive mechanical ventilation in the PACU (4 CXRs), 11 expected abnormalities (5 found) in patients who received an indwelling tube, line or catheter during surgery (186 CXRs).
Full table
Unexpected abnormalities
In 267 of the 294 routinely obtained CXRs no abnormalities were expected. In 94 CXRs an unexpected abnormality was found (Table 3): 29 unexpected abnormalities after thoracic surgery (82 CXRs), 0 unexpected abnormalities in patients who continued with invasive mechanical ventilation (4 CXRs), and 38 unexpected abnormalities in patients who received an indwelling tube, line or catheter during surgery (208 CXRs) (Table 4).

Full table
Diagnostic efficacy and treatment impact
The diagnostic efficacy was 32% (94/294). The treatment impact was 4% (11/294) (Table 4). These results were not different for the diverse patient categories.
Discussion
The results of this observational study can be summarized as follows: (I) the majority of routinely obtained CXRs in PACU patients are obtained with the expectation to find no abnormalities but to exclude pathology; (II) the diagnostic efficacy of routinely obtained postoperative CXRs is fair; (III) the treatment impact of routinely obtained postoperative CXRs is poor.
To our best knowledge, this is the largest observational prospective study analysing the clinical value of CXRs in PACU patients. Its findings are in line with those from previous studies in mixed cohorts of postoperative patients (2), including patients after thoracic surgery (7,10,21,22) and patients after general surgery (1). We found central venous catheter misplacement to be a common finding on routinely obtained postoperative CXRs 9% (16/186), less than in a previous study showing an incidence of 14% (23). However, our study also shows that an abnormal position (most frequently dispositioning with the tip in the right atrium of the heart) almost never triggered the attending physician to relocate the catheter. Several studies suggest that the value of a routine CXRs after placement of a central venous catheter is poor, especially when the procedure was uncomplicated (3,5,24,25), and that a CXR should only be obtained when the patient reports unilateral chest pain with decreased breath sounds at the side of placement, if air was aspirated during the procedure, or in case of other difficulties occurred during the procedure (24). Notably, we did not score whether a central venous catheter was placed under ultrasound guidance, which is now a standard approach in the ICU.
The poor treatment impact, together with the risks of obtaining these CXRs may be reasonable arguments in the discussion whether we should stop abrogate the practice of routine CXRs. Several studies showed a low diagnostic efficacy and poor treatment impact of postoperative routinely obtained CXRs in ICU patients (9-12). Also randomized controlled trials (13-15) and one meta-analysis (16) suggest that daily routine CXRs could be safely deleted from daily intensive care unit practice (18). The results of our study are in line with these findings.
Although we are convinced that the low therapeutic efficacy of routinely obtained postoperative CXRs should be considered an argument to stop obtaining these CXRs, one could also postulate that a CXR showing no abnormalities is equally important for surgeons or PACU physicians. Surgeons and PACU physicians could even consider the admission CXRs as a good reference, in case a patients’ condition worsens during stay in the PACU or later on in the ward. One could also argue that the treatment impact of routinely obtained postoperative CXR is not poor, but that attending physicians reacted poorly, or maybe even insufficiently to findings on the CXRs. Indeed, if CXRs show that the tip of a central venous catheter is located too deep, but that those CXRs almost never triggered attending physicians to reposition those catheters, one could also say that the attending physicians need training, instead of ‘blaming’ the routinely obtained CXR to have a poor treatment impact. Of note, findings were similar in the ICU setting in previous studies (9,12,19,20). However, this discussion is rather subjective because physicians might disagree on whether a change in management is really necessary or not. Nevertheless, we focused on facts, i.e., whether routine CXRs in the PACU actually did change management, as it reflects what happens in daily practice. Our study was not designed to determine what would happen if ‘better educated physicians’ should have interpreted the CXRs.
Although we could not perform a cost-benefit analysis in this purely observational study, it is suggestive that a restrictive policy for routine CXRs may have the potential to have significant effects on cost. In line with this, abandoning routine CXRs may lead to less radiation exposure to patients and possibly also lower daily workloads of radiologists and radiology workers.
We consider the independent evaluation of the CXRs by radiologists, and the fact that the attending physicians were unaware of the evaluation of therapeutic actions in response to the CXRs strengths of our study. The purely descriptive and uncontrolled design of the present investigation limits the interpretation of our findings. Indeed, we could have missed changes in treatment purely because of inadequate administration of patient records, but more importantly, we could not score for actions that were omitted because the CXRs did not confirm the presence of an abnormality. The last, however, is probably of less concern since we evaluated routinely obtained CXRs, not CXRs on demand. Other important drawbacks of our study include the following. ‘Request behaviour’ by physicians might significantly have influenced the analysis of the diagnostic value of CXRs. This was not controlled for. In addition, we recognize that the results of this study might not simply be translated to other centres. Indeed, differences in staff and patient populations might affect the diagnostic and therapeutic efficacy of postoperative CXRs in PACU patients. Additional studies might be needed to determine whether abolishing routinely obtained postoperative CXR is a safe and acceptable strategy in PACU patients.
In conclusion, the clinical value of routinely obtained postoperative CXRs in PACU patients seems poor. Considering the costs and labour associated with obtaining these CXRs, we should consider abrogating these CXRs from daily practice, and consider only CXRs on indication.
Acknowledgements
We would like to thank all our colleagues for their help and support in conducting this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The Institutional Review Board of the Academic Medical Center, Amsterdam, The Netherlands reviewed and approved the study protocol and analysis plan, and waived the need for individual patient informed consent seen the observational nature of this study (W12_201 # 12.17.0222; 29 August 2012).
References
- Silverstein DS, Livingston DH, Elcavage J, et al. The utility of routine daily chest radiography in the surgical intensive care unit. J Trauma 1993;35:643-6. [Crossref] [PubMed]
- Barak M, Markovits R, Guralnik L, et al. The utility of routine postoperative chest radiography in the postanesthesia care unit. J Clin Anesth 1997;9:351-4. [Crossref] [PubMed]
- Lessnau KD. Is chest radiography necessary after uncomplicated insertion of a triple-lumen catheter in the right internal jugular vein, using the anterior approach? Chest 2005;127:220-3. [Crossref] [PubMed]
- Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intraartrial central venous catheter position? Chest 2008;134:527-33. [Crossref] [PubMed]
- Lucey B, Varghese JC, Haslam P, et al. Routine chest radiographs after central line insertion: mandatory postprocedural evaluation or unnecessary waste of resources? Cardiovasc Intervent Radiol 1999;22:381-4. [Crossref] [PubMed]
- Henschke CI, Yankelevitz DF, Wand A, et al. Accuracy and efficacy of chest radiography in the intensive care unit. Radiol Clin North Am 1996;34:21-31. [PubMed]
- Tolsma M, Bentala M, Rosseel PM, et al. The value of routine chest radiographs after minimally invasive cardiac surgery: an observational cohort study. J Cardiothorac Surg 2014;9:174. [Crossref] [PubMed]
- Rao PS, Abid Q, Khan KJ, et al. Evaluation of routine postoperative chest X-rays in the management of the cardiac surgical patient. Eur J Cardiothorac Surg 1997;12:724-9. [Crossref] [PubMed]
- Kröner A, Van Iperen E, Horn J, et al. The low therapeutic efficacy of postoperative chest radiographs for surgical intensive care unit patients. Minerva Anestesiol 2011;77:147-53. [PubMed]
- Hornick PI, Harris P, Cousins C, et al. Assessment of the value of the immediate postoperative chest radiograph after cardiac operation. Ann Thorac Surg 1995;59:1150-3. [Crossref] [PubMed]
- Tolsma M, Kroner A, van den Hombergh CL, et al. The clinical value of routine chest radiographs in the first 24 hours after cardiac surgery. Anesth Analg 2011;112:139-42. [Crossref] [PubMed]
- Hendrikse KA, Gratama JW, Hove W, et al. Low value of routine chest radiographs in a mixed medical-surgical ICU. Chest 2007;132:823-8. [Crossref] [PubMed]
- Krivopal M, Shlobin OA, Schwartzstein RM. Utility of daily routine portable chest radiographs in mechanically ventilated patients in the medical ICU. Chest 2003;123:1607-14. [Crossref] [PubMed]
- Hejblum G, Chalumeau-Lemoine L, Ioos V, et al. Comparison of routine and on-demand prescription of chest radiographs in mechanically ventilated adults: a multicentre, cluster-randomised, two-period crossover study. Lancet 2009;374:1687-93. [Crossref] [PubMed]
- Clec'h C, Simon P, Hamdi A, et al. Are daily routine chest radiographs useful in critically ill, mechanically ventilated patients? A randomized study. Intensive Care Med 2008;34:264-70. [Crossref] [PubMed]
- Oba Y, Zaza T. Abandoning daily routine chest radiography in the intensive care unit: meta-analysis. Radiology 2010;255:386-95. [Crossref] [PubMed]
- Ganapathy A, Adhikari NK, Spiegelman J, et al. Routine chest x-rays in intensive care units: a systematic review and meta-analysis. Crit Care 2012;16:R68. [Crossref] [PubMed]
- Amorosa JK, Bramwit MP, Mohammed TL, et al. ACR appropriateness criteria routine chest radiographs in intensive care unit patients. J Am Coll Radiol 2013;10:170-4. [Crossref] [PubMed]
- Graat ME, Choi G, Wolthuis EK, et al. The clinical value of daily routine chest radiographs in a mixed medical-surgical intensive care unit is low. Crit Care 2006;10:R11. [Crossref] [PubMed]
- Kager LM, Kroner A, Binnekade JM, et al. Review of a large clinical series: the value of routinely obtained chest radiographs on admission to a mixed medical--surgical intensive care unit. J Intensive Care Med 2010;25:227-32. [Crossref] [PubMed]
- Tolsma M, Rijpstra TA, Rosseel PM, et al. Defining indications for selective chest radiography in the first 24 hours after cardiac surgery. J Thorac Cardiovasc Surg 2015;150:225-9. [Crossref] [PubMed]
- Bello SO, Page A, Sadat U, et al. Chest X-ray and electrocardiogram in post-cardiac surgery follow-up clinics: should this be offered routinely or when clinically indicated? Interact Cardiovasc Thorac Surg 2013;16:725-30. [Crossref] [PubMed]
- Gladwin MT, Slonim A, Landucci DL, et al. Cannulation of the internal jugular vein: is postprocedural chest radiography always necessary? Crit Care Med 1999;27:1819-23. [Crossref] [PubMed]
- Guth AA. Routine chest X-rays after insertion of implantable long-term venous catheters: necessary or not? Am Surg 2001;67:26-9. [PubMed]
- Miccini M, Cassini D, Gregori M, et al. Ultrasound-guided placement of central venous port systems via the right internal jugular vein: Are chest X-ray and/or fluoroscopy needed to confirm the correct placement of the device? World J Surg 2016;40:2353-8. [Crossref] [PubMed]


