Insulin autoimmune syndrome: from diagnosis to clinical management
Introduction
Autoimmune forms of hypoglycemia are the third leading cause of hypoglycemia in Japanese people, but this condition is rare among other ethnicities. As a consequence, it is often misdiagnosed or identified late, after numerous expensive and unnecessary biochemical and radiological examinations have proved fruitless. This review covers all aspects of the autoimmune forms of hypoglycemia, from diagnosis to treatment. New knowledge gained on the issue and published in the literature will be discussed. The review is divided into two parts: the first describes the hypoglycemic syndrome due to insulin autoantibodies (IAS), or Hirata’s disease; the second concerns the form of hypoglycemia caused by antibodies directed against the insulin receptor (type B insulin resistance), or Flier’s disease.
Insulin autoimmune syndrome
Definition
Insulin autoimmune syndrome (IAS) is characterized by: (I) hyperinsulinemic hypoglycemia; (II) elevated insulin autoantibody (IAA) titers; (III) no prior exposure to exogenous insulin; (IV) no pathological abnormalities of the pancreatic islets. This condition is also known as Hirata’s disease (HD), after Yukimasa Hirata, the author who first described the syndrome in 1970 (1).
Epidemiology
In Japan, IAS is the third leading cause of hypoglycemia, after insulinoma and extrapancreatic neoplasias. From when it was first described up until 2009, at least 380 cases of IAS were identified in Japan (2), in a population of around 128 million (3). IAS is more common in Asian people than in Western countries, where the condition is rare, though its incidence is increasing. A retrospective survey of cases of endogenous hyperinsulinemic hypoglycemia (EHH) seen at a Korean tertiary-level hospital calculated the prevalence of IAS at 6%, much higher than in the West (4). This study was also interesting because it mentioned the decline in the incidence of nesidioblastosis since IAA assays were introduced as a routine test in cases of EHH. The authors also presented a case of IAS misdiagnosed as nesidioblastosis after surgical biopsy (4). So, IAS still risks being misdiagnosed if IAA titers are not measured promptly in cases of EHH. This might also explain the increased incidence of IAS, due to a greater awareness of the problem. From 1985 to 2014, only 84 cases of IAS were reported in China (5), a nation with a population of 1.4 billion (6). Only two case have been described in India so far (7,8). The first case of IAS in a Caucasian patient was reported in Norway in 1970 (9). By 2009, at least 58 new cases had been described in non-Asian populations (10), and more cases have been reported since. In most cases identified outside Asian countries, patients with IAS are white (10). IAS affects both sexes equally (10), and occurs more frequently in patients over 40 years of age. The condition is rare among children: to the best of our knowledge, as at 2017 only 25 pediatric patients had been reported worldwide (11-13). An individual’s predisposition to IAS is significantly influenced by their ethnic and genetic background.
Trigger factors and diseases associated with IAS
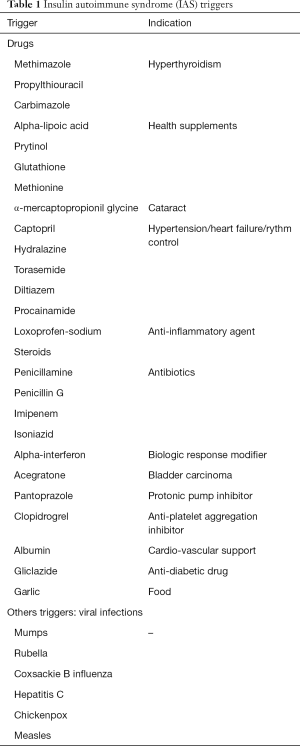
IAA may be triggered by exposure to drugs or viruses, or they may manifest spontaneously (14). Table 1 shows a list of the drugs and viral infections capable of inducing IAS. Nearly one in two Japanese patients with IAS had prior exposure to drugs (15). Among Caucasian patients too, half of the cases were related to drug exposure (10). Unlike the Japanese patient population, however, in which spontaneous cases are common (10), nearly one in two Caucasian patients have other autoimmune diseases or hematological disorders [monoclonal gammopathy of undetermined significance (MGUS)], or multiple myeloma (10). Viral infections, acting as super-antigens, may also trigger the production of IAA, and thereby cause IAS (16). The syndrome has been associated with mumps, rubella, Coxsackie B influenza, hepatitis C, chickenpox and measles (14). It is noteworthy that only a minority of non-Asian patients developed IAS spontaneously, without any related drug exposure, infections or autoimmune/hematological diseases.
Full table
Generally speaking, medications or drugs containing sulfhydryl groups are associated with IAS. It has been argued that sulfhydryl groups may be able to bind and reduce the sulfhydryl bonds connecting insulin chains A and B, making endogenous insulin more immunogenic (17).
The prevalence of IAS induced by anti-thyroid drugs (ATD) is high in Japan and in Asian countries, while any role of Graves’ disease (GD) per se as a risk factor has been ruled out (18). The drug most frequently described as a trigger of IAS in GD is methimazole, but there have also been reports of cases caused by propylthiouracil and carbimazole. It is worth noting that IAS is a very rare phenomenon in non-Japanese GD patients on ATD, with only a handful of cases reported in the literature (19-23). This strikingly different prevalence might be explained by the different HLA setting in Japanese and Caucasian people with GD (see the section on Genetics). As mentioned earlier, the prevalence of IAS is increasing, and this is partly due to the widespread use of dietary supplements containing α-lipoic (also called thioctic) acid (ALA) (24). ALA is extensively used to treat diabetic neuropathy, or as an anti-aging health supplement (25,26). In the presence of reduced nicotinamide adenine dinucleotide (NADH) or reduced nicotinamide adenine dinucleotide phosphate (NADPH), ALA is reduced to dihydrolipoic acid, a complex that includes a sulfhydryl group with a strong reducing activity (26). To date, 27 cases of IAS induced by ALA have been described in the literature, 18 from Japan, and 9 from other countries. It is also worth mentioning the description of 3 cases of IAS induced by clopidogrel, a widely-used anti-platelet drug (27,28), in both Japanese and Caucasian individuals. Clopidogrel does not have a sulfhydryl group of its own, but the drug’s active metabolite has a triggering chemical structure. Physicians should be warned about the drug’s metabolite being a possible cause of IAS, and consider withdrawing it to achieve a clinical improvement. Another widely-used compound is albumin. It has recently been demonstrated that albumin has a cysteine residue (Cys34) with a strong reducing capacity, like ALA. Kamei et al. described a case of IAS occurring in a patient who was taking no drugs containing a sulfhydryl group, but who was taking albumin (29). Loxoprofen-sodium is capable of inducing IAS even when administered through adhesive skin patches (30). It is fundamentally important to obtain a patient’s detailed clinical history in this context.
Genetic background
In 1992, a strong association was observed in the Japanese population between IAS and the presence of the human leukocyte antigen (HLA)-DR4 (48 out of 50 patients vs. controls; odds ratio 39.6) (31,32). The predisposition to IAS among Japanese people was subsequently found strongly associated with DRB1*0406 (42 out of 48 DR4-positive patients; odds ratio 56.6). The odds ratio was lower for DRB1*0403 1.6 (5 out of 48 DR4-positive patients), and for DRB1*0407 1.1 (1 out of 48 DR4-positive patients). Such an association indicates that glutamine at position 74 in the DRB1 molecule (shared by all three alleles) is essential to the development of IAS, and serine at position 37 (unique to DRB1*0406) greatly increases an individual’s predisposition to the disease (33). The different distributions of HLA-DR4 alleles around the world was investigated in an effort to explain the high prevalence of IAS in Japan, and its low prevalence elsewhere (34). It emerged that HLA-DRB1*0406 is quite prevalent among Eastern Asian patients, whereas Caucasian IAS patients mainly express HLA-DRB1*0403, and have a low prevalence of DRB1*0406. Populations with a high prevalence of DRB1*0406 are therefore at higher risk of developing IAS than populations with a low prevalence of this genetic marker. This is a clear example of the association between a genetic susceptibility to class II HLA genes and the risk of developing certain autoimmune diseases. The most common condition associated with IAS in Japan is GD treated with ATD, since all the patients with GD who developed IAS in Japan expressed DRB1*0406, while the GD patients without the syndrome did not (34,35). Outside Japan, IAS is very rare among GD patients taking ATD (19-21,36) and this is probably due to the low frequency of DRB1*0406 among patients with GD in these populations. In Korean people, the HLAs conferring susceptibility to GD are more frequently linked to DRB1*0803 and DRB1*1602, while DRB1*0406 is only present in 9% of Korea’s GD patients (37). Confirmation of the strict correlation between HLA status and drug-induced susceptibility comes from the fact that one of the two patients with ATD-treated GD who developed IAS in Korea carried the DRB1*0406 (36). In China, only three patients with GD reportedly developed IAS while on ATD: two of them revealed DRB1*0406; the third, a 26-year-old pregnant woman (38), was not HLA-typed. To our knowledge, there have been no cases of IAS developing in GD patients taking ATD in Italy, probably because GD in Italy is usually associated with DRB1*03 (39), while cases with DRB1*0406 are very rare. Another clear association between drugs and genetic backgrounds is between ALA and HLA-DRB1*0406. In fact, all the 20 Asian patients who developed IAS after taking ALA carried HLA-DRB1*0406, while only nearly half of the Caucasian patients carried HLA-DRB1*0406, and the others had HLA-DRB1*0403 (25,26,40).
Clinical presentation, mechanisms, and related pathophysiology
Clinical presentation
Hypoglycemia in IAS may occur postprandially or on fasting, and its severity can vary. Although symptoms are usually mild and transient, very severe cases have also been described, with prolonged hypoglycemia and life-threatening consequences (41,42). The first step in the diagnosis of IAS is to identify hypoglycemia, the signs and symptoms of which are non-specific, and there is no single glucose level cut-off for defining it categorically. So, to avoid conducting unnecessary, expensive and potentially harmful tests, the Endocrine Society Clinical Practice Guideline recommends that a patient should be assessed for hypoglycemia if Whipple’s triad (signs and/or symptoms of hypoglycemia, and their resolution after glucose/food intake) is documented (17). The symptoms of hypoglycemia may be: neuroglycopenic (due to brain glucose deficiency), with behavioral changes, confusion, fatigue, seizures, and loss of consciousness; or neurogenic (due to a physiological reaction to hypoglycemia), such as palpitations, tremor, anxiety (an adrenergic response); or cholinergic (sweating, hunger, paresthesia). In healthy individuals, symptoms of hypoglycemia generally appear when glucose levels drop below 3 mmol/L (55 mg/dL), but in individuals with recurrent hypoglycemia, and in children and women, symptoms may only appear when glucose levels are lower. That is why it is impossible to establish a particular glucose level for defining hypoglycemia (17). Many hypoglycemic patients may also have a paradoxical hyperglycemia occurring shortly after meals or oral glucose challenge.
Features of IAA in IAS
Physicians should be aware of many possible pitfalls when they consider ruling out any presence of IAA. For a start, IAA are heterogeneous because they can belong to different immunoglobulin (Ig) classes, although the most common is IgG. Commercially-available kits for detecting IAA can generally only identify the IgG class of IAA. To avoid false results, it is therefore important to start with a test capable of ruling out any presence of all IAA, irrespective of their Ig class. Polyethylene glycol (PEG) is an inexpensive method within the capabilities of any laboratory, and can precipitate any form of IAA Ig. PEG should always be used in suspect cases, following up with a more specific test to identify the class of IAA involved, where necessary (14,39).
To provide a thorough presentation of the syndrome, it is worth spending a few words on the IAA related to other conditions. Although the immunogenicity of insulin analogs is low (compared with human insulin), administering exogenous insulin may induce insulin-binding antibodies. These IAA are usually weak, and tend to disappear when insulin administration is stopped or switched to another formulation (43). In rare cases, however, insulin-induced IAA can behave as in IAS, combining with free insulin, delaying insulin clearance, and causing late post-prandial hypoglycemia episodes (44,45) or, in some cases, inducing insulin resistance. Indeed, many cases of unexplained unstable glycemic control in the literature have been attributed to insulin-induced IAA—including cases of severe hypoglycemia due to IAA interference requiring immunosuppressant treatment and plasmapheresis (46). The possibility of IAA formation and interference in DM-1 patients with unexplained labile glycemic control and hypoglycemia must therefore be taken seriously. Although the classical definition IAS requires that patients have not been exposed to exogenous insulin, IAA-related IAS has rarely been described in diabetic patients given exogenous insulin whose hypoglycemia resolved even without discontinuing their insulin treatment or switching to another insulin formulation (47). It is also important to remember that, in 1983, IAA were frequently demonstrated in young patients newly-diagnosed with DM-1 before they received any insulin therapy, and they were interpreted as an autoimmune marker of B cell damage (48). IAA are associated with other markers of pancreatic autoimmunity, and inversely correlate with patients’ age: they are found in 48% of patients of pediatric age with DM-1 as opposed to 3.8% of those developing the disease as adults (49).
IAA can also be seen as a risk marker of pancreatic autoimmunity in school-age children, or in the first-degree relatives of patients with DM-1. Seroconversion to IAA occurred earlier (P<0.01) than for other autoantibodies against glutamic acid decarboxylase (GAD), insulinoma-associated protein 2 (IA-2), or zinc transporter 8 (ZnT8). The incidence of early peak seroconversion was highest in children with the high-risk HLA DR3/4-DQ8 or DR4/4-DQ8 genotypes. The time of life between 9 months to 2 years old is associated with a high incidence of activation of the autoimmunity associated with type 1 diabetes in children genetically at risk, and this period should be targeted for effective primary prevention strategies (50). IAA have also been described in up to 2% of blood samples taken from healthy blood donors (51), but at low titers they have no pathological effects.
Mechanisms
IAS is an autoimmune disease that fits the bill for the novel type VII hypersensitivity, defined as an immunological disease caused by an autoantibody against circulating target proteins or hormones (52). IAS is caused by the presence of large amounts of IAA, an autoantibody against insulin in the circulation. IAA can be found in some individuals with an established autoimmunity (53), and in patients with DM-1, especially those who develop the disease at a younger age (54).
In patients carrying IAA with a critical quantity and affinity during fasting, insulin concentrations are low and IAA are not occupied. After food intake and a rise in blood glucose levels, pancreatic β-cells produce insulin, which is bound by IAA, thus making the insulin ineffective and causing post-prandial hyperglycemia. This situation then prompts the production of larger amounts of insulin and C-peptide to cope with the IAA-induced hyperglycemic effects. When the binding capacity of the IAA is exceeded, pancreatic insulin secretion stops, the IAA-insulin complexes create a reserve of insulin, and its release from the IAA gives rise to hypoglycemia (39,55). Sustained levels of insulin also inhibit counter-regulatory mechanisms of glucose homeostasis, thus contributing to making the hypoglycemia last longer. The severity and duration of the hypoglycemia, and the swing from a hyper- to a hypoglycemic state depend on the intrinsic dissociation rate constant (K-1), titer and intrinsic affinity/avidity to insulin (Ka) of the IAA (14). Although the presence of insulin-binding antibodies is the feature common to all cases of IAS, it may be that the binding of proinsulin antibodies is predominant and, if they cross-react with assay kits, they can contribute to raising insulin levels too. Since proinsulin has only a tenth of the bioactivity of insulin, symptoms in such cases are usually milder (14). In Japanese people, most patients with IAS have polyclonal IgG autoantibodies (25), whereas IAA are monoclonal in more than one in two non-Asian patients. Although the IgG class of IAA is the most common, cases of IAS caused by IAA in the IgA and IgM classes have also been described (56,57).
In the case of hematological diseases, the pathophysiology reported in many studies differs from the classical mechanism proposed for hypoglycemia in IAS. The first case of myeloma associated with IAS was described in 1972 (58). Since then, another 10 cases of MGUS/myeloma-related IAS have been reported (59,60). In such rare conditions—in the setting of the monoclonal diseases characterizing myeloma and MGUS—it may be that the monoclonal antibody produced by the clone of B lymphocyte interacts with a self-antigen. If the monoclonal antibody has sufficient affinity for the self-antigen, this can result in a clinical syndrome. This seems to be what happens in the setting of IAS due to MGUS/myeloma (59). These conditions are usually characterized by the presence of high-capacity/low affinity antibodies: in this setting IAA generally have a lower affinity for insulin than the insulin receptor. Immunocomplexes of IAA-insulin delay the clearance of insulin, which can dissociate from the IAA due to its weak binding constant, and bind instead to its receptor, thus causing hypoglycemia (56).
Pathology
There are some reports in the literature of patients with IAS being misdiagnosed as cases of insulinoma and consequently undergoing pancreas surgery, not only in the past, but even more recently (4,61). On histological examination, hyperplasia of the pancreatic islets was found in one case (61), while a case of nesidioblastosis was documented on the pancreas biopsy from the other IAS patient (4).
Diagnosis
When plasma glucose levels are below 3 mmol/L, then there will be physiologically suppressed levels of insulin (below 18 mol/L or 3 U/mL), C-peptide (below 0.2 nmol/L or 0.6 ng/mL), and proinsulin (below 5 pmol/L). When hyperinsulinemic hypoglycemia is detected, C-peptide and proinsulin levels are useful for orienting the differential diagnosis: if C-peptide and proinsulin levels are high or inappropriately normal, then the intake of exogenous hypoglycemic agents like sulfonylureas and insulinoma should be ruled out; conversely, exogenous insulin administration should be suspected in the event of low C-peptide and proinsulin levels.
In IAS, as a result of IAA bound to insulin, the insulin t1\2 increases from 5 minutes to hours (55), while the half-life of C-peptide usually remains unaffected (30–35 minutes). Patients with IAS thus typically have high serum insulin concentrations, while their C-peptide and proinsulin levels may or may not be raised, depending partly on the characteristics of the IAA produced (which may or may not be capable of binding endogenous proinsulin and C-peptide as well, and thus delaying their half-lives too), and partly on the type of laboratory assay used (and the variable ability of the IAA to interfere with the immunoassay used for the proinsulin and C-peptide measurements). The presence of IAA can thus mimic a number of pathological conditions, prompting expensive and potentially harmful diagnostic assessments, and even pancreatectomy to search for an insulinoma. The importance of testing for IAA in non-diabetic adults with hyperinsulinemic hypoglycemia has also been emphasized by the Endocrine Society, which has included IAA among the first-line tests to perform in such patients (17). Many authors advocate measuring the insulin to C-peptide ratio to diagnose IAS. In fact, insulin and C-peptide are co-secreted by the pancreatic β-cells in physiological conditions, then insulin is rapidly metabolized by the liver, while C-peptide is slowly eliminated by the kidneys. The half-life is 5–10 minutes for the former, and 30–35 minutes for the latter, so the normal insulin to C-peptide ratio is <1 (62,63). In IAS, as explained earlier, the half-life of insulin is delayed as a consequence of IAA binding, but the elimination time of C-peptide remains unchanged, so the ratio is reversed to >1. That said, IAA are very heterogeneous and can sometimes bind C-peptide too, so they may or may not interfere with C-peptide measurements (also depending on the type of assay used), making this diagnostic parameter unreliable.
Finally, to arrive at a correct diagnosis, it is fundamentally important to obtain a patient’s detailed history, including age, sex, race, personal and family history of autoimmune and/or hematological disorders, use of drugs and any health supplements, concomitant viral or bacterial infections, time and mode of hypoglycemia onset (fasting or post-prandial), and its response to sugar. The diagnosis of IAS is often very difficult. Feng and colleagues (64) described a case of IAS occurring in a DM-2 patient treated with gliclazide who had no history of exogenous insulin administration. Being a sulfonylurea, gliclazide can induce hypoglycemia accompanied by high levels of insulin and C-peptide, so identifying the hypoglycemia as being caused by IAS and treating the patient accordingly was a challenge.
Treatment
In Japanese patients, IAS is generally self-limiting, and tends to regress within 3–6 months after withdrawal of the trigger drug (65). In non-Asian patients too, symptoms improve, resolving completely over time if patients stop taking the drug that caused the symptoms and follow a few recommendations. Patients are generally advised to eat frequent, small meals low in carbohydrates to prevent fasting, and to avoid the release of insulin associated with glucose overload of the pancreas. Cornstarch is a glucose polymer that is slowly absorbed by the gastrointestinal tract, and consequently able to avoid a sharp rise in glucose after meals and prevent fasting hypoglycemia episodes. In fact, uncooked cornstarch and hydrothermally modified cornstarch (its more effective and better tolerated evolution) are generally used in patients with glycogen storage disease, and in endurance athletes’ diets. There are reports of their successful use in IAS to keep glucose levels stable (66,67). If oral nutrition is impossible, or during longer fasting periods (i.e., at night), then continuous enteral feeding may be required (65). Patients with more severe IAS may also benefit from continuous glucose monitoring to help predict and promptly respond to falling blood glucose levels (68,69).
A specific treatment is required for the few patients whose hypoglycemia is more severe (65). Acarbose is an α-glucosidase inhibitor used to treat reactive idiopathic postprandial hyperinsulinemic hypoglycemia episodes as it is able to delay carbohydrate absorption (70). Acarbose can be used in IAS to dampen the postprandial rise in serum glucose and insulin, but it is poorly tolerated due to adverse gastrointestinal effects such as diarrhea and flatus. Since severe refractory autoimmune hypoglycemia is an autoimmune-based condition, it has also been treated with high-dose corticosteroids, such as prednisone, with good results in terms of both glycemic control and IAA titers (26,65). Plasmapheresis has also been widely used, alone or in combination with corticosteroids in more severe cases, to control hypoglycemic symptoms and lower IAA titers more rapidly (26,71). Plasmapheresis alone is especially useful when glucocorticoids are contraindicated (72).
Rituximab has recently been introduced for the treatment of many patients with life-threatening hypoglycemia and refractory to high-dose corticosteroids (69,73-75). The rationale is that this anti-CD20 monoclonal antibody was found capable (in the TrialNet) of suppressing IAA in 40% of DM-1 patients (76). It also improved the outcome of a patient with DM-1 who developed IAA to exogenous insulin (75). Used in the setting of IAS, rituximab was successful in reducing, but not suppressing patients’ IAA titers, thus improving their hypoglycemia control, and enabling the use of lower steroid doses as a consequence (69).
The treatment of IAS in the context of a myeloma and MGUS is particularly challenging. There can be no spontaneous remission in such cases if the myeloma/MGUS is still active. Patients need to take numerous small meals and keep to a diet low in simple sugars, probably for life, and they must learn how to recognize and treat their hypoglycemia episodes. In some cases, hypoglycemic crises are severe enough to necessitate plasmapheresis, glucocorticoids, and even chemotherapy, in an effort to reduce the levels of anti-insulin-binding monoclonal immunoglobulins (59). The levels of IAA and the severity of the symptoms sometimes parallel the remission-relapse phases of myeloma.
Type B insulin resistance syndrome
Definition
Insulin resistance syndromes include a broad array of disorders characterized by insulin resistance and a consequently increased β-cell insulin secretion. Among the different types of insulin resistance syndrome, the genetically-determined forms comprise numerous syndromes related to an insulin receptor or insulin receptor signal impairment [type A insulin resistance syndrome (OMIM147670), Rabson-Mendehall syndrome (OMIM262190), leprechaunism (OMIM246200), lipodystrophy (OMIM 608594)] (77,78). These syndromes generally manifest at birth or in infancy and early childhood (with extreme insulin resistance, growth retardation, acanthosis nigricans, hirsutism, and polycystic ovarian disease in patients who are not usually obese). Hyperandrogenism (HA), insulin resistance (IR), and acanthosis nigricans (AN) characterize HAIR-AN syndrome, which becomes manifest in obese, anovulatory women, and is considered a form of polycystic ovary syndrome (PCOS) (78). Insulin type-B resistance syndrome (TBIRS) was first reported by Kahn et al. in 1976 (77), and the same authors subsequently demonstrated that it is due to circulating antibodies that block the membrane receptors for insulin (79,80). TBIRS is a rare autoimmune disorder resulting in a variety of abnormalities in glucose homeostasis, from hypoglycemia to extremely insulin-resistant hyperglycemia, caused by the presence of insulin receptor autoantibodies (IRAbs) (81-83).
Epidemiology
The exact prevalence of TBIRS is not known, but it is quite rare (82). As at 2014, only 67 cases had been reported worldwide (82,84). Arioglu and colleagues studied 24 patients with this syndrome and found a higher prevalence in females (20/24 patients, 84%), and people of Afro-American ethnicity (21/24, 88%), consistently with previous and subsequent case reports (85). Other cases have since been described in Asian people too (84), and 20% of all published cases involved Asian patients, while white people seem to be less prone to the syndrome (84). The median clinical age at onset is 39 years (range, 15–64 years) in females, and 56 years in males (range, 37–68 years), but TBIRS has also been reported in adolescents, in a 1-year-old baby, and in the elderly (10,82,86).
TBIRS has a strong association with other autoimmune conditions (82,85), and IRAbs may be a paraneoplastic manifestation of hematological disorders like multiple myeloma and Hodgkin’s disease (85).
Clinical presentation, mechanisms, triggers and related pathophysiology
Clinical presentation
The most common presenting sign of TBIRS is severe diabetes mellitus, which responds poorly to treatment with exogenous insulin. Hypoglycemia may follow, or more rarely, it may be the first, or even the only (13%) sign of the syndrome (82). TBIRS can also manifest with other typical symptoms of insulin resistance, one of the more evident being acanthosis nigricans which consists in areas of skin thickening and hyperpigmentation. This symptom is found in up to 88% of patients (82). Peculiar to this form of insulin resistance is acanthosis nigricans of the periocular, perioral, and labial regions, which results in typical facies (82). Trunks and buttocks, and mucocutaneous tissues such as the lips or vulva may be involved (82). Most female patients present with enlarged and inhomogeneous multi-cystic ovaries, and one in two female patients of reproductive age have biochemical hyperandrogenism, with high testosterone levels.
TBIRS is often associated with other autoimmune diseases, but the strongest association reported in the literature is with systemic lupus erythematosus (SLE) (82). In a 28-year follow-up review (82), 11/24 (46%) patients with TBIRS also had SLE, while 6 other patients met 3 of the 4 criteria for a diagnosis of SLE, and 1 patient had primary biliary cirrhosis, 1 had myeloma, and no other associated diseases were found in just 5 cases. TBIRS has also been found associated with autoimmune hepatitis (87), hypothyroidism, and vitiligo (88). As in IAS due to insulin autoantibodies, hypoglycemia induced by IRAbs can develop in the context of hematological diseases, like myeloma (82) or Hodgkin’s disease (HD) (89-92). TBIRS has been described as a paraneoplastic symptom in patients with HD and multiple myeloma. In fact, monoclonal paraneoplastic form of IRAbs is a possibility, as in the mechanism described for IAS. The metabolic manifestations may also anticipate the diagnosis of the hematological disorder, which may be suspected when a monoclonal peak is found on electrophoresis (82). In fact, IRAbs are typically polyclonal.
The ten-year mortality rate for TBIRS is reportedly as high as 54%, due largely to the severity of the underlying systemic disease (82), while the proven disease-related deaths are associated with hypoglycemia (10,82).
Mechanisms
TBIRS is caused by circulating polyclonal autoantibodies to insulin receptor, generally immunoglobulins in the IgG class (77,79). IRAbs have a biphasic action, and this can explain the clinical course of the disease, which involves severe hyperglycemia but also hypoglycemia. In 3T3-L1 adipocyte cultures, there was a rapid-onset, short-term insulin-mimetic effect (93,94), then this response fades and adipocytes become insulin-resistant. A parallel biphasic response was observed in vivo too, in rats injected with IRAbs (95): in a first phase the antibodies caused hypoglycemia (occurring within 2–4 hours and lasting 8–24 hours), but chronic administration induced insulin resistance and hyperglycemia. When the antibodies were given in high titers, the antagonistic effect (insulin resistance) prevailed, whereas with low titers the agonistic effect (insulin-mimetic action) gained the upper hand (95).
The first rapid phase seems to relate to activation of the tyrosine kinase receptor (96,97), which is then followed by a gradual down-regulation of the receptor, a greater degradation and a diminished exposition on the cell surface, with consequent insulin resistance (98).
Another proposed mechanism for the fluctuating course of the disease involves the simultaneous presence of agonistic and antagonistic anti-insulin receptor autoantibodies, in variable titers and ratios (10,14,99).
Autoantibodies are also capable of increasing hepatic glucose release, and impairing muscle glucose uptake, and these mechanisms can contribute to hyperglycemia (100).
It is impossible to predict whether the presence of IRAbs will result in hypo- or hyperglycemia, but there are a few issues to consider. In the National Institutes of Health (NIH) series, hypoglycemia was more prevalent in patients with low autoantibody titers, and the switch from hyperglycemia to hypoglycemia was preceded by a drop in antibody titers (82). So, the insulin-mimetic effect may be dominant in patients with low anti-insulin antibody titers. The course of the disease is unfortunately not always predictable on the basis of antibody titers, however. When Flier et al. charted the course of the syndrome during a 3-year follow-up, 2 of their patients experienced a first hyperglycemic phase, characterized by high autoantibody titers, followed by refractory hypoglycemia despite no change in their antibody titers. This behavior was caused by the patients’ autonomous proliferation of membrane insulin receptors (99). The possibility of two populations of antibodies coexisting, with agonistic and antagonistic effects, further complicates the picture and makes the clinical course of TBIRS unpredictable.
Triggers
Pegylated interferon and ribavirin are the cornerstone of treatment for HCV infections, but many reports have associated interferon with the onset of various autoimmune disorders (101), including TBIRS (102). Three such cases have been reported in the literature (102-104). Mohammedi et al. described a case of severe insulin resistance in a diabetic African woman with HIV after she initiated a course of highly-active antiretroviral therapy (HAART). The setting for the TBIRS was part of an immune reconstitution inflammatory syndrome (IRIS), which involves a number of manifestations of a restored autoimmune response after the patient started HIV treatment and her CD4+ count rose. TBIRS presenting with severe hypoglycemia was also described in a child who had undergone bone marrow transplantation for severe combined immunodeficiency a few months earlier. Nagayama et al. described a case of TBIRS presenting with hypoglycemia in a patient with SLE due to the disease becoming more active after hemodialysis treatment (105).
In conclusion, there are no established triggers for the development of IRAbs, but drugs and situations capable of inducing autoimmunity reactivation may be contributors.
Diagnosis
The clinical hallmarks of severe insulin resistance can suggest the diagnosis. Hypoglycemia or hyperglycemia resistant to high-dose insulin therapy are typical of TBIRS. Circulating insulin levels are high, even in the hypoglycemic phase (10,82), possibly leading to insulinoma being suspected (85). The high insulin levels have been attributed to an increased insulin secretion from the pancreas in an attempt to overcome peripheral insulin resistance and contain insulin clearance (14). High serum insulin levels can be accompanied by low proinsulin and C-peptide levels, thus mimicking the pattern of injectable insulin administration, and this can be misleading for diagnostic purposes until the presence of IRAbs is ruled out (14).
Unlike the case of many other insulin resistance syndromes, in TBIRS patients have low triglyceride levels, averaging 54 mg/dL in the NIH series (82), and 49 mg/dL in a later single-center study (10). Another biochemical peculiarity of TBIRS is a paradoxical hyperadiponectinemia, reaching very high levels despite the extreme insulin resistance (106). There are no clinical features that can help to establish this diagnosis. TBIRS may be suspected in patients with extreme insulin resistance associated with high basal insulin levels, or requiring very high doses of insulin for metabolic control, with acanthosis nigricans, low triglyceride levels, or high adiponectin levels, and with other autoimmune or hematological diseases. Female gender, African-American ethnicity and hyperandrogenism can reinforce the clinical suspicion. The method used to detect IRAbs by measuring immunoprecipitation of recombinant human insulin receptors (82) is not commercially available, and can be performed at few laboratories worldwide (96), so serological confirmation based on IRAbs assay is not very feasible.
Treatment
Patients with TBIRS require two types of treatment: one for glycemic control, and one for immunomodulation. As regards their metabolic control, in the hyperglycemic phase these patients may require very large doses of exogenous insulin to try to control their catabolic state. Daily doses may be 5,100 U (82), or even as high as 30,000 U in some reports (88). It may be easier to administer such doses of insulin intravenously in hospital, or by opting for concentrated U-500 regular human insulin formulations over standard insulin formulations (85,107). Once fasting euglycemia has been achieved, the insulin doses can be reduced, since fasting euglycemia may be evidence of a decline in antibody titer, or of the switch to an agonist action on the insulin receptor (85).
Since IRAbs also impair liver and muscle insulin sensitivity, drugs acting as insulin sensitizers can have a role in the treatment of TBIRS. Metformin and thiazolidinedione can help to reduce the doses of exogenous insulin needed for glycemic control (82,85,108). Liraglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has been used effectively in many reports, even in a patient with TBIRS and insulin allergy (85,109,110).
Insulin growth factor 1 (IGF-1) can exert a hypoglycemic effect similar to that of insulin, but far less powerful, with a potency approximately 8% of that of insulin (111,112). IGF-1 is able to stimulate glucose transport and glycogen synthesis in the muscles, via insulin and IGF-1 receptor (113). IGF-1 has been used in the treatment of many syndromes characterized by extreme insulin resistance, and numerous reports testify to its efficacy in the treatment of TBIRS too, when patients are refractory to other therapies (114,115). Whatever the treatment, it is important to control patients’ diet: it has been demonstrated that hyperalimentation impairs glucose control and raises the insulin doses needed to achieve euglycemia (116). Hyperglycemia can be difficult to manage, but controlling hypoglycemia can be even harder, and it carries a higher mortality risk (82,85). Frequent meals, even during the night, or continuous glucose infusions are the basis of treatment.
In the largest single-center series in the literature, among the patients with complete data on their long-term follow-up, 33% of patients with TBIRS had a spontaneous remission. In other words, their IRAbs disappeared spontaneously over a period of 11–48 months (82). The majority of patients require an immunosuppressant therapy, which can also help euglycemia to be achieved more quickly.
Glucocorticoids are generally part of empirical treatments, with oral pulse doses preferred over continuous administration, as the latter can have a worse effect on hyperglycemia (85). High-dose corticosteroids can reverse hypoglycemia acutely (within 24 hours), though the mechanism behind this therapeutic effect has yet to be clarified (82).
Plasmapheresis has been used in approximately 10 cases, especially when acute control was required (84). The main drawback of this therapy is the lack of any long-term efficacy, so it has to be combined with immunosuppressant agents (82,84). Intravenous immunoglobulins have been less extensively used, but they proved effective in reducing insulin resistance in the few cases in which they were administered (84,117). Cyclophosphamide (118-121), mycophenolate mofetil (119,121), cyclosporine A (122), and azathioprine have been used, achieving an improvement in patients’ symptoms (85). Rituximab, an anti-CD20 monoclonal antibody, proved particularly efficient in reducing anti-insulin receptor autoantibodies. Since its use was first described by Coll et al. (123), several cases of TBIRS have reportedly been successfully treated with rituximab (124). Very often, these agents were used in combination, however, making it very difficult to establish which therapeutic agent induced the remission. Clinical response to these agents is unpredictable, so there are no specific guidelines available on the choice of treatment, and the type of immunosuppressant therapy should be customized, depending on the underlying autoimmune disorder or specific clinical setting. The NIH group recently proposed a standardized therapeutic regimen, however, that they had used in 7 of their patients, all of whom achieved remission, with no serious adverse effects (121). Their treatment protocol aimed to control the pathogenic autoantibody production, and consisted in a combination of rituximab, cyclophosphamide and pulse corticosteroids. Remission was defined as an amelioration of the hyperglycemia and discontinuation of insulin therapy. The average time to remission in the patients following this scheme was 5 months (range, 2.5–9 months), but most patients had a reduction in their insulin doses already after the first cycle of treatment (121). This timeline is far shorter than previously reported in the literature, using an empirical treatment scheme (82). More importantly, none of the patients treated with the proposed protocol experienced hypoglycemic phases (121), unlike the previous empirically-treated case series described by the NIH group (82). Randomized, placebo-controlled trials are unlikely, owing to the rarity of the disorder, so—given the striking results obtained with this approach—rituximab with pulsed glucocorticoids and cyclophosphamide, followed by azathioprine, can currently be considered the best choice for TBIRS patient management.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hirata Y, Ishizu H, Ouchi N, et al. Insulin autoimmunity in a case of spontaneous hypoglycemia. J Jpn Diabet Soc 1970;13:312-20.
- Uchigata Y, Hirata Y, Iwamoto Y. Drug-induced insulin autoimmune syndrome. Diabetes Res Clin Pract 2009;83:e19-20. [Crossref] [PubMed]
- Uchigata Y, Hirata Y. Insulin Autoimmune Syndrome (Hirata Disease). In: Immunoendocrinology: Scientific and Clinical Aspects. Totowa, NJ: Humana Press, 2011:343-67.
- Woo CY, Jeong JY, Jang JE, et al. Clinical features and causes of endogenous hyperinsulinemic hypoglycemia in Korea. Diabetes Metab J 2015;39:126-31. [Crossref] [PubMed]
- Wang YL, Yao PW, Zhang XT, et al. Insulin Autoimmune Syndrome: 73 Cases of Clinical Analysis. Chin Med J (Engl) 2015;128:2408-9. [Crossref] [PubMed]
- Zhang Y, Zhao T. Hypoglycemic coma due to insulin autoimmune syndrome induced by methimazole: A rare case report. Exp Ther Med 2014;8:1581-4. [Crossref] [PubMed]
- Gopal K, Priya G, Gupta N, et al. A case of autoimmune hypoglycemia outside Japan: Rare, but in the era of expanding drug-list, important to suspect. Indian J Endocrinol Metab 2013;17:1117-9. [Crossref] [PubMed]
- Gite J, Shrivastav R, Bhasin N, et al. Recurrent Hypoglycaemia due to Insulin Autoimmune Disease (Hirata Disease) Associated with Monoclonal Gammopathy of Unknown Significance. J Assoc Physicians India 2015;63:68-9. [PubMed]
- Folling I, Norman N. Hyperglycemia, hypoglycemic attacks, and production of anti-insulin antibodies without previous known immunization. Immunological and functional studies in a patient. Diabetes 1972;21:814-26. [Crossref] [PubMed]
- Lupsa BC, Chong AY, Cochran EK, et al. Autoimmune Forms of Hypoglycemia. Medicine (Baltimore) 2009;88:141-53. [Crossref] [PubMed]
- Alves C, Constança J, De León DD, et al. A novel atypical presentation of insulin autoimmune syndrome (Hirata’s disease) in a child. J Pediatr Endocrinol Metab 2013;26:1163-6. [Crossref] [PubMed]
- Savas-Erdeve S, Yılmaz Agladioglu S, Onder A, et al. An Uncommon Cause of Hypoglycemia: Insulin Autoimmune Syndrome. Horm Res Paediatr 2014;82:278-82. [Crossref] [PubMed]
- Lee SH, Oh SH, Chung WY. Insulin autoimmune syndrome induced by methimazole in a Korean girl with Graves’ disease. Ann Pediatr Endocrinol Metab 2013;18:32-5. [Crossref] [PubMed]
- Ismail AAA. The insulin autoimmune syndrome (IAS) as a cause of hypoglycaemia: an update on the pathophysiology, biochemical investigations and diagnosis. Clin Chem Lab Med 2016;54:1715-24. [Crossref] [PubMed]
- Uchigata Y, Eguchi Y, Takayama-Hasumi S, et al. Insulin autoimmune syndrome (Hirata disease): clinical features and epidemiology in Japan. Diabetes Res Clin Pract 1994;22:89-94. [Crossref] [PubMed]
- Bodansky HJ, Grant PJ, Dean BM, et al. Islet-cell antibodies and insulin autoantibodies in association with common viral infections. Lancet 1986;2:1351-3. [Crossref] [PubMed]
- Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2009;94:709-28. [Crossref] [PubMed]
- Takei M. Insulin auto-antibodies produced by methimazole treatment in the patients with Graves’ disease. J Tokyo Women’s Med Coll 1980;50:54.
- Sklenar I, Wilkin TJ, Diaz JL, et al. Spontaneous hypoglycemia associated with autoimmunity specific to human insulin. Diabetes Care 1987;10:152-9. [Crossref] [PubMed]
- Virally ML, Timsit J, Chanson P, et al. Insulin autoimmune syndrome: a rare cause of hypoglycaemia not to be overlooked. Diabetes Metab 1999;25:429-31. [PubMed]
- Gomez Cruz MJ, Jabbar M, Saini N, et al. Severe hypoglycemia secondary to methimazole-induced insulin autoimmune syndrome in a 16 year old African-American male. Pediatr Diabetes 2012;13:652-5. [Crossref] [PubMed]
- Zhang Y, Zhao T. Hypoglycemic coma due to insulin autoimmune syndrome induced by methimazole: A rare case report. Exp Ther Med 2014;8:1581-4. [Crossref] [PubMed]
- Basu A, Service FJ, Yu L, et al. Insulin autoimmunity and hypoglycemia in seven white patients. Endocr Pract 2005;11:97-103. [Crossref] [PubMed]
- Furukawa N, Miyamura N, Nishida K, et al. Possible relevance of alpha lipoic acid contained in a health supplement in a case of insulin autoimmune syndrome. Diabetes Res Clin Pract 2007;75:366-7. [Crossref] [PubMed]
- Uchigata Y. The novel agent, alpha lipoic acid, can cause the development of insulin autoimmune syndrome. Intern Med 2007;46:1321-2. [Crossref] [PubMed]
- Gullo D, Evans JL, Sortino G, et al. Insulin autoimmune syndrome (Hirata Disease) in European Caucasians taking α-lipoic acid. Clin Endocrinol (Oxf) 2014;81:204-9. [Crossref] [PubMed]
- Yamada E, Okada S, Saito T, et al. Insulin autoimmune syndrome during the administration of clopidogrel. J Diabetes 2016;8:588-9. [Crossref] [PubMed]
- Rajpal A, Kassem LS, Moscoso-Cordero M, et al. Clopidogrel-Induced Insulin Autoimmune Syndrome: A Newly Recognized Cause of Hypoglycemia in a Patient Without Diabetes. J Endocr Soc 2017;1:1217-23. [Crossref] [PubMed]
- Kamei S, Kaneto H, Shigemoto R, et al. Human serum albumin: Possible cause of insulin autoimmune syndrome. J Diabetes Investig 2016;7:919-20. [Crossref] [PubMed]
- Okazaki-Sakai S, Yoshimoto S, Yagi K, et al. Insulin autoimmune syndrome caused by an adhesive skin patch containing loxoprofen-sodium. Intern Med 2013;52:2447-51. [Crossref] [PubMed]
- Uchigata Y, Omori Y, Nieda M, et al. HLA-DR4 genotype and insulin-processing in insulin autoimmune syndrome. Lancet 1992;340:1467. [Crossref] [PubMed]
- Uchigata Y, Kuwata S, Tokunaga K, et al. Strong association of insulin autoimmune syndrome with HLA-DR4. Lancet 1992;339:393-4. [Crossref] [PubMed]
- Uchigata Y, Tokunaga K, Nepom G, et al. Differential immunogenetic determinants of polyclonal insulin autoimmune syndrome (Hirata’s disease) and monoclonal insulin autoimmune syndrome. Diabetes 1995;44:1227-32. [Crossref] [PubMed]
- Uchigata Y, Hirata Y, Omori Y, et al. Worldwide differences in the incidence of insulin autoimmune syndrome (Hirata disease) with respect to the evolution of HLA-DR4 alleles. Hum Immunol 2000;61:154-7. [Crossref] [PubMed]
- Uchigata Y, Kuwata S, Tsushima T, et al. Patients with Graves’ disease who developed insulin autoimmune syndrome (Hirata disease) possess HLA-Bw62/Cw4/DR4 carrying DRB1*0406. J Clin Endocrinol Metab 1993;77:249-54. [PubMed]
- Roh E, Kim YA, Ku EJ, et al. Two cases of methimazole-induced insulin autoimmune syndrome in graves’ disease. Endocrinol Metab (Seoul) 2013;28:55-60. [Crossref] [PubMed]
- Park MH, Park YJ, Song EY, et al. Association of HLA-DR and -DQ genes with Graves disease in Koreans. Hum Immunol 2005;66:741-7. [Crossref] [PubMed]
- Zeng XX, Tang YL, Hu KX, et al. Insulin autoimmune syndrome in a pregnant female. Medicine (Baltimore) 2017;96. [Crossref] [PubMed]
- Censi S, Albergoni MP, Gallo N, et al. Insulin autoimmune syndrome (Hirata’s disease) in an Italian patient: a case report and review of the literature. Clin Chem Lab Med 2018;56:889-95. [Crossref] [PubMed]
- Takeuchi Y, Miyamoto T, Kakizawa T, et al. Insulin Autoimmune Syndrome possibly caused by alpha lipoic acid. Intern Med 2007;46:237-9. [Crossref] [PubMed]
- Ismail AAA. Testing for insulin antibodies is mandatory in the differential diagnosis of hypoglycaemia in nondiabetic subjects. Clin Endocrinol (Oxf) 2012;76:603-4. [Crossref] [PubMed]
- Vogeser M, Parhofer KG, Fürst H, et al. Autoimmune hypoglycemia presenting as seizure one week after surgery. Clin Chem 2001;47:795-6. [PubMed]
- Lamy PJ, Sault C, Renard E. High fasting serum insulin level due to autoantibody interference in insulin immunoassay discloses autoimmune insulin syndrome: a case report. Ann Biol Clin (Paris) 2016;74:490-4. [PubMed]
- Li R, Mao J, Yu K, et al. Medical Nutrition Therapy Is Effective in the Management of Hypoglycemia Caused by Insulin Antibodies: A Case Report and Literature Review. J Am Coll Nutr 2016;35:86-90. [Crossref] [PubMed]
- Matsuyoshi A, Shimoda S, Tsuruzoe K, et al. A case of slowly progressive type 1 diabetes with unstable glycemic control caused by unusual insulin antibody and successfully treated with steroid therapy. Diabetes Res Clin Pract 2006;72:238-43. [Crossref] [PubMed]
- Sharwood EF, Hughes IP, Pretorius CJ, et al. Therapeutic plasma exchange normalizes insulin-mediated response in a child with type 1 diabetes and insulin autoimmune syndrome. Pediatr Diabetes 2018;19:171-9. [Crossref] [PubMed]
- Wang X, Xu X, Zhao X, et al. Hypoglycemia due to insulin binding antibodies in a patient with insulin-treated type 2 diabetes and Graves’ disease. Endocrine 2013;43:236-7. [Crossref] [PubMed]
- Palmer JP, Asplin CM, Clemons P, et al. Insulin antibodies in insulin-dependent diabetics before insulin treatment. Science 1983;222:1337-9. [Crossref] [PubMed]
- Karjalainen J, Salmela P, Ilonen J, et al. A comparison of childhood and adult type I diabetes mellitus. N Engl J Med 1989;320:881-6. [Crossref] [PubMed]
- Ziegler A-G, Bonifacio E. BABYDIAB-BABYDIET Study Group. Age-related islet autoantibody incidence in offspring of patients with type 1 diabetes. Diabetologia 2012;55:1937-43. [Crossref] [PubMed]
- Sodoyez JC, Sodoyez-Goffaux F, Koch M, et al. Clonally restricted insulin autoantibodies in a cohort of 2200 healthy blood donors. Diabetologia 1990;33:719-25. [Crossref] [PubMed]
- Uchigata Y, Hirata Y, Omori Y. A novel concept of type VII hypersensitivity introduced by insulin autoimmune syndrome (Hirata’s disease). Autoimmunity 1995;20:207-8. [Crossref] [PubMed]
- Wilkin TJ, Nicholson S. Autoantibodies against human insulin. Br Med J (Clin Res Ed) 1984;288:349-52. [Crossref] [PubMed]
- Fineberg SE, Biegel AA, Durr KL, et al. Presence of insulin autoantibodies as regular feature of nondiabetic repertoire of immunity. Diabetes 1991;40:1187-93. [Crossref] [PubMed]
- Ismail AAA. The double whammy of endogenous insulin antibodies in non-diabetic subjects. Clin Chem Lab Med 2008;46:153-6. [Crossref] [PubMed]
- Halsall DJ, Mangi M, Soos M, et al. Hypoglycemia due to an insulin binding antibody in a patient with an IgA-kappa myeloma. J Clin Endocrinol Metab 2007;92:2013-6. [Crossref] [PubMed]
- Elias D, Cohen IR, Schechter Y, et al. Antibodies to insulin receptor followed by anti-idiotype. Antibodies to insulin in child with hypoglycemia. Diabetes 1987;36:348-54. [Crossref] [PubMed]
- Heffernan AG. Unusual presentation of multiple myeloma. Postgrad Med J 1972;48:238-40. [Crossref] [PubMed]
- Lichtman MA, Balderman SR. Unusual Manifestations of Essential Monoclonal Gammopathy. II. Simulation of the Insulin Autoimmune Syndrome. Rambam Maimonides Med J 2015;6. [Crossref] [PubMed]
- Arzamendi AE, Rajamani U, Jialal I. Pseudoinsulinoma in a white man with autoimmune hypoglycemia due to anti-insulin antibodies: value of the free C-Peptide assay. Am J Clin Pathol 2014;142:689-93. [Crossref] [PubMed]
- Uchigata Y, Hirata Y. Insulin autoimmune syndrome (IAS, Hirata disease). Ann Med Interne (Paris) 1999;150:245-53. [PubMed]
- Lebowitz MR, Blumenthal SA. The molar ratio of insulin to C-peptide. An aid to the diagnosis of hypoglycemia due to surreptitious (or inadvertent) insulin administration. Arch Intern Med 1993;153:650-5. [Crossref] [PubMed]
- Wong SL, Priestman A, Holmes DT. Recurrent Hypoglycemia from Insulin Autoimmune Syndrome. J Gen Intern Med 2014;29:250-4. [Crossref] [PubMed]
- Feng X, Yuan L, Hu Y, et al. Gliclazide-Induced Insulin Autoimmune Syndrome: A Rare Case Report and Review on Literature. Endocr Metab Immune Disord Drug Targets 2016;16:230-4. [Crossref] [PubMed]
- Donegan DM, Vella A. 69-year-old man with recurrent episodes of confusion and diaphoresis. Mayo Clin Proc 2013;88:410-3. [Crossref] [PubMed]
- Deguchi A, Okauchi Y, Suehara S, et al. Insulin autoimmune syndrome in a health supplement user: the effectiveness of cornstarch therapy for treating hypoglycemia. Intern Med 2013;52:369-72. [Crossref] [PubMed]
- Lechner K, Aulinger B, Brand S, et al. Hydrothermally modified slow release corn starch: a potential new therapeutic option for treating hypoglycemia in autoimmune hypoglycemia (Hirata’s disease). Eur J Clin Nutr 2015;69:1369-70. [Crossref] [PubMed]
- Philippon M, Sejil S, Mugnier M, et al. Use of the continuous glucose monitoring system to treat insulin autoimmune syndrome: quantification of glucose excursions and evaluation of treatment efficacy. Diabet Med 2014;31:e20-4. [Crossref] [PubMed]
- Saxon DR, McDermott MT, Michels AW. Novel Management of Insulin Autoimmune Syndrome with Rituximab and Continuous Glucose Monitoring. J Clin Endocrinol Metab 2016;101:1931-4. [Crossref] [PubMed]
- Güemes M, Melikyan M, Senniappan S, et al. Idiopathic postprandial hyperinsulinaemic hypoglycaemia. J Pediatr Endocrinol Metab 2016;29:915-22. [Crossref] [PubMed]
- Dozio N, Scavini M, Beretta A, et al. Imaging of the Buffering Effect of Insulin Antibodies in the Autoimmune Hypoglycemic Syndrome. J Clin Endocrinol Metab 1998;83:643-8. [PubMed]
- Annese S, Fadini G, Maran A. Caso di ipoglicemia autoimmune trattata con plasmaferesi. G It Diabetol Metab 2008;28:162-4.
- Church D, Hunter RW, Lyall M, et al. Resolution of Hypoglycemia and Cardiovascular Dysfunction After Rituximab Treatment of Insulin Autoimmune Syndrome. Diabetes Care 2017;40:e80-2. [Crossref] [PubMed]
- Kroemer TM, Erler A, Tsourdi E, et al. Immunoadsorption Followed by Rituximab as a Definitive Treatment for Insulin Autoimmune Syndrome (Hirata Syndrome): A Case Report. Diabetes Care 2018;41:e23-4. [Crossref] [PubMed]
- Jassam N, Amin N, Holland P, et al. Analytical and clinical challenges in a patient with concurrent type 1 diabetes, subcutaneous insulin resistance and insulin autoimmune syndrome. Endocrinol Diabetes Metab Case Rep 2014;2014. [Crossref] [PubMed]
- Yu L, Herold K, Krause-Steinrauf H, et al. Rituximab selectively suppresses specific islet antibodies. Diabetes 2011;60:2560-5. [Crossref] [PubMed]
- Kahn CR, Flier JS, Bar RS, et al. The Syndromes of Insulin Resistance and Acanthosis Nigricans. N Engl J Med 1976;294:739-45. [Crossref] [PubMed]
- Musso C, Cochran E, Moran SA, et al. Clinical course of genetic diseases of the insulin receptor (type A and Rabson-Mendenhall syndromes): a 30-year prospective. Medicine (Baltimore) 2004;83:209-22. [Crossref] [PubMed]
- Flier JS, Kahn CR, Roth J, et al. Antibodies that impair insulin receptor binding in an unusual diabetic syndrome with severe insulin resistance. Science 1975;190:63-5. [Crossref] [PubMed]
- Flier JS, Kahn CR, Jarrett DB, et al. Characterization of antibodies to the insulin receptor: a cause of insulin-resistant diabetes in man. J Clin Invest 1976;58:1442-9. [Crossref] [PubMed]
- Arky RA. Antibodies and Disorders of Glucose Metabolism. N Engl J Med 1982;307:1445-7. [Crossref] [PubMed]
- Arioglu E, Andewelt A, Diabo C, et al. Clinical course of the syndrome of autoantibodies to the insulin receptor (type B insulin resistance): a 28-year perspective. Medicine (Baltimore) 2002;81:87-100. [Crossref] [PubMed]
- Taylor SI, Grunberger G, Marcus-Samuels B, et al. Hypoglycemia Associated with Antibodies to the Insulin Receptor. N Engl J Med 1982;307:1422-6. [Crossref] [PubMed]
- Zhang S, Wang G, Wang J. Type B insulin resistance syndrome induced by systemic lupus erythematosus and successfully treated with intravenous immunoglobulin: case report and systematic review. Clin Rheumatol 2013;32:181-8. [Crossref] [PubMed]
- Willard DL, Stevenson M, Steenkamp D. Type B insulin resistance syndrome. Curr Opin Endocrinol Diabetes Obes 2016;23:318-23. [Crossref] [PubMed]
- Cruz PD, Hud JA. Excess insulin binding to insulin-like growth factor receptors: proposed mechanism for acanthosis nigricans. J Invest Dermatol 1992;98:82S-5S. [Crossref] [PubMed]
- Fareau GG, Maldonado M, Oral E, et al. Regression of acanthosis nigricans correlates with disappearance of anti-insulin receptor autoantibodies and achievement of euglycemia in type B insulin resistance syndrome. Metabolism 2007;56:670-5. [Crossref] [PubMed]
- Page KA, Dejardin S, Kahn CR, et al. A patient with type B insulin resistance syndrome, responsive to immune therapy. Nat Clin Pract Endocrinol Metab 2007;3:835-40. [Crossref] [PubMed]
- Braund WJ, Naylor BA, Williamson DH, et al. Autoimmunity to insulin receptor and hypoglycaemia in patient with Hodgkin’s disease. Lancet 1987;1:237-40. [Crossref] [PubMed]
- Chan JC, Zhu SQ, Ho SK, et al. Hypoglycaemia and Hodgkin’s disease. Br J Haematol 1990;76:434-6. [Crossref] [PubMed]
- Khokher MA, Avasthy N, Taylor AM, et al. Insulin-receptor antibody and hypoglycaemia associated with Hodgkin’s disease. Lancet 1987;1:693-4. [Crossref] [PubMed]
- Walters EG, Tavaré JM, Denton RM, et al. Hypoglycaemia due to an insulin-receptor antibody in Hodgkin’s disease. Lancet 1987;1:241-3. [Crossref] [PubMed]
- Van Obberghen E, Spooner PM, Kahn CR, et al. Insulin-receptor antibodies mimic a late insulin effect. Nature 1979;280:500-2. [Crossref] [PubMed]
- Grunfeld C, Van Obberghen E, Karlsson FA, et al. Antibody-induced desensitization of the insulin receptor. Studies of the mechanism of desensitization in 3T3-L1 fatty fibroblasts. J Clin Invest 1980;66:1124-34. [Crossref] [PubMed]
- Dons RF, Havlik R, Taylor SI, et al. Clinical disorders associated with autoantibodies to the insulin receptor. Simulation by passive transfer of immunoglobulins to rats. J Clin Invest 1983;72:1072-80. [Crossref] [PubMed]
- Rodriguez O, Collier E, Arakaki R, et al. Characterization of purified autoantibodies to the insulin receptor from six patients with type B insulin resistance. Metabolism 1992;41:325-31. [Crossref] [PubMed]
- Zick Y, Rees-Jones RW, Taylor SI, et al. The role of antireceptor antibodies in stimulating phosphorylation of the insulin receptor. J Biol Chem 1984;259:4396-400. [PubMed]
- Taylor SI, Marcus-Samuels B. Anti-receptor antibodies mimic the effect of insulin to down-regulate insulin receptors in cultured human lymphoblastoid (IM-9) cells. J Clin Endocrinol Metab 1984;58:182-6. [Crossref] [PubMed]
- Flier JS, Bar RS, Muggeo M, et al. The evolving clinical course of patients with insulin receptor autoantibodies: spontaneous remission or receptor proliferation with hypoglycemia. J Clin Endocrinol Metab 1978;47:985-95. [Crossref] [PubMed]
- Pedersen O, Hjøllund E, Beck-Nielsen H, et al. Diabetes mellitus caused by insulin-receptor blockade and impaired sensitivity to insulin. N Engl J Med 1981;304:1085-8. [Crossref] [PubMed]
- Fujioka T, Honda M, Yoshizaki T, et al. A case of type 1 diabetes onset and recurrence of Graves’ disease during pegylated interferon-α plus ribavirin treatment for chronic hepatitis C Intern Med 2010;49:1987-90. [Crossref] [PubMed]
- Popescu C, Popescu G-A, Arama V. Type 1 diabetes mellitus with dual autoimmune mechanism related to pegylated interferon and ribavirin treatment for chronic HCV hepatitis. J Gastrointestin Liver Dis 2013;22:101-4. [PubMed]
- Daniel AL, Houlihan JL, Blum JS, et al. Type B insulin resistance developing during interferon-alpha therapy. Endocr Pract 2009;15:153-7. [Crossref] [PubMed]
- Uto H, Matsuoka H, Murata M, et al. A case of chronic hepatitis C developing insulin-dependent diabetes mellitus associated with various autoantibodies during interferon therapy. Diabetes Res Clin. Pract 2000;49:101-6. [Crossref] [PubMed]
- Nagayama Y, Morita H, Komukai D, et al. Type B insulin resistance syndrome induced by increased activity of systemic lupus erythematosus in a hemodialysis patient. Clin Nephrol 2008;69:130-4. [Crossref] [PubMed]
- Semple RK, Halberg NH, Burling K, et al. Paradoxical elevation of high-molecular weight adiponectin in acquired extreme insulin resistance due to insulin receptor antibodies. Diabetes 2007;56:1712-7. [Crossref] [PubMed]
- Cochran E, Musso C, Gorden P. The use of U-500 in patients with extreme insulin resistance. Diabetes Care 2005;28:1240-4. [Crossref] [PubMed]
- Di Paolo S. Metformin ameliorates extreme insulin resistance in a patient with anti-insulin receptor antibodies: description of insulin receptor and postreceptor effects in vivo and in vitro. Acta Endocrinol (Copenh) 1992;126:117-23. [Crossref] [PubMed]
- Matsumoto Y, Yamada H, Funazaki S, et al. Effect of Liraglutide on Type B Insulin Resistance Syndrome and Insulin Allergy in Type 2 Diabetes: A Case Report Diabetes Ther 2017;8:1191-4. [Crossref] [PubMed]
- Hirai H, Ogata E, Kikuchi N, et al. The effects of liraglutide on both hypereosinophilic insulin allergy and the characteristics of anti-insulin antibodies in type 2 diabetes mellitus: a case report. J Med Case Rep 2016;10:202. [Crossref] [PubMed]
- Guler HP, Zapf J, Froesch ER. Short-term metabolic effects of recombinant human insulin-like growth factor I in healthy adults. N Engl J Med 1987;317:137-40. [Crossref] [PubMed]
- Guler HP, Schmid C, Zapf J, et al. Effects of recombinant insulin-like growth factor I on insulin secretion and renal function in normal human subjects. Proc Natl Acad Sci U. S. A. 1989;86:2868-72. [Crossref] [PubMed]
- Froesch ER, Zapf J. Insulin-like growth factors and insulin: comparative aspects. Diabetologia 1985;28:485-93. [Crossref] [PubMed]
- Kawashiri S-Y, Kawakami A, Fujikawa K, et al. Type B insulin resistance complicated with systemic lupus erythematosus. Intern Med 2010;49:487-90. [Crossref] [PubMed]
- Hirano T, Adachi M. Insulin-like growth factor 1 therapy for type B insulin resistance. Ann Intern Med 1997;127:245-6. [Crossref] [PubMed]
- Vesely DL, Coleman MJ, Kohler PO, et al. Hyperalimentation as cause of markedly worsened metabolic control in a patient with autoantibodies to the insulin receptor. Am J Med 1985;79:504-8. [Crossref] [PubMed]
- Tran HA, Reeves GE. Treatment of type B insulin resistance with immunoglobulin: novel use of an old therapy. Med J Aust 2009;190:168. [PubMed]
- Mohammedi K, Roussel R, El Dbouni O, et al. Type B insulin resistance syndrome associated with an immune reconstitution inflammatory syndrome in an HIV-infected woman. J Clin Endocrinol Metab 2011;96:E653-7. [Crossref] [PubMed]
- Gehi A, Webb A, Nolte M, et al. Treatment of systemic lupus erythematosus-associated type B insulin resistance syndrome with cyclophosphamide and mycophenolate mofetil. Arthritis Rheum 2003;48:1067-70. [Crossref] [PubMed]
- Yang GQ, Li YJ, Dou JT, et al. Type B insulin resistance syndrome with Scleroderma successfully treated with multiple immune suppressants after eradication of Helicobacter pylori infection: a case report. BMC Endocr Disord 2016;16:20. [Crossref] [PubMed]
- Malek R, Chong AY, Lupsa BC, et al. Treatment of type B insulin resistance: a novel approach to reduce insulin receptor autoantibodies. J Clin Endocrinol Metab 2010;95:3641-7. [Crossref] [PubMed]
- Yamamoto T, Sato T, Mori T, et al. Clinical efficacy of insulin-like growth factor-1 in a patient with autoantibodies to insulin receptors: a case report. Diabetes Res Clin Pract 2000;49:65-9. [Crossref] [PubMed]
- Coll AP, Thomas S, Mufti GJ. Rituximab therapy for the type B syndrome of severe insulin resistance. N Engl J Med 2004;350:310-1. [Crossref] [PubMed]
- Iseri K, Iyoda M, Shikida Y, et al. Rituximab for the treatment of type B insulin resistance syndrome: a case report and review of the literature. Diabet Med 2017;34:1788-91. [Crossref] [PubMed]


