Biochemical markers of acute intestinal ischemia: possibilities and limitations
Introduction
Although acute intestinal ischemia is a relative rare abdominal emergency, this condition may be associated with high morbidity and mortality due to inadequate arterial or venous blood flow resulting from embolism, thrombosis or a non-occlusive low-flow state in the splanchnic circulation (1). Acute intestinal ischemia can involve the small or large intestine, and usually presents with sudden severe non-specific abdominal pain (1). The mortality usually ranges between 60–80% depending on etiology, age and diagnostic delay (2,3).
Overall, this condition represents less than 1% of all acute admissions to emergency departments, but a rapid diagnosis and therapeutic management are compelling for adequately restoring blood flow and preventing intestine necrosis, up to patient death (4). The pathophysiology is complex and multifaceted. The intestinal acute vascular insufficiency leads to renin-angiotensin activation, sympathic stimulation, vasospasm and consequently hypoxia (5). These events may cause cell death by apoptosis, with consequent cellular desquamation of the mucosal intestinal villi (5,6). The impairment of the epithelial barrier also promotes contact with microorganisms or endotoxins, with ensuing development of an inflammatory condition. The persistence of ischemia may then lead to an evolvement of transmural infarction towards irreversible injury and necrosis, intestinal perforation and release of bacteria and toxins into the systemic circulation (6).
Clinical signs and symptoms of acute intestinal ischemia are typically non-specific and, combined with the fact that the condition is relatively rare a rapid and accurate diagnosis remains challenging. Despite ample research in this field, early, sensitive and specific biomarkers of acute intestinal ischemia have not been identified so far (7-11). Along with clinical history taking, physical examination and imaging investigations, the classic diagnostic approach to patients with suspected acute intestinal ischemia encompasses a conventional panel of laboratory tests, including complete blood count (CBC), D-dimer and blood gas analysis. In the effort to ameliorate the diagnosis, other biomarkers have been proposed over the past few years, the most widely used of which is total lactic acid (12,13). Among some other more innovative biomarkers, recent evidence has been provided that the concentrations of D-lactate, intestinal fatty acid-binding protein (I-FABP), ischemia modified albumin (IMA), α-glutathione S-transferase (α-GST) and citrulline may be frequently abnormal in association with gut barrier dysfunction, so that they seem the more promising candidates for the diagnosis of acute intestinal diseases (5). The aim of this narrative review is hence to provide an overview on traditional laboratory biomarkers of acute intestinal ischemia and summarize current evidence regarding some emerging and potentially useful biomarkers.
Biomarkers of hypoxia and oxidative stress
The most clinically interesting oxidative stress-related biomarkers appear indeed lactate, IMA and α-GST. Lactic acid is prevalently generated from, and metabolized to, pyruvate by the lactate dehydrogenase (LDH). This compound is present in nature in two separate isomers. L-lactate is the end product of anaerobic glycolysis, whilst D-lactate is mainly generated by intestinal bacteria metabolism. Since mammalian cells only contain L-LDH, the isomer endogenously synthesized in humans is almost exclusively L-lactate, which considerably increases during tissue hypoperfusion and cellular hypoxia (14).
Several clinical studies reported increased L-lactate blood values in the vast majority of patients with acute mesenteric ischemia (12,15). More specifically, Janda et al. (16) showed a 10-fold increase of lactic acid in patients who developed postoperative occlusion of intestinal arteries. Experimental studies have also confirmed that blood lactate significantly increases after mesenteric ischemia (17). Aydin et al. also observed that mean L-lactate values began to increase 4 hours after with mesenteric ischemia induced by ligating the superior mesenteric artery in rats, and this increase lasted up to the 6th hour (18). Irrespective of this promising finding, L-lactate remains a poorly specific biomarkers of intestinal ischemia, since its blood values tend to increase in many other intestinal and non-intestinal diseases, such as stomach perforation, pancreatitis, perforated appendicitis, diabetic keto-acidosis and malignancy (19,20).
D-lactate is normally produced at very low concentrations in humans. The small amount of D-lactate normally present in blood mainly originates from cellular production thought the methylglyoxal pathway or from ingestion of foods containing D-lactate, such as yoghurts, soured cream and cheese (and, to a lesser extent, tomatoes, apple, beer and wine) (21). Since some bacterial species constitutively contain both L- and D-enzymes, and have therefore the capability to generate produce D-lactate, the bacteria normally resident in the large intestine are perhaps is the sources cause of D-lactate (22). On the other hand, an alteration of mucosal integrity due to intestinal ischemia may be a reasonable cause of increased D-lactate concentration in blood. In the meta-analysis of Treskes et al. (10), including six studies, the pooled sensitivity and specificity of D-lactate for diagnosing acute mesenteric ischemia were 0.72 (95% CI: 0.59–0.82) and 0.74 (95% CI: 0.69–0.79), respectively. Nevertheless, the included studies were characterized by a large heterogeneity for patients’ selection, methods used for measuring D-lactate and timing of blood sampling (10).
Although D-lactate seems hence to perform better than L-lactate because of its exclusively intestinal source, the results obtained in different studies are mostly inconsistent (23). Notably, increased values of D-lactate were observed in patients with short-bowel syndrome or jejunoileal bypass operation, as well as in subjects with high carbohydrate intake, decreased colon motility or in those using probiotics (20).
IMA is a biologic marker that can be easily and inexpensively measured in clinical laboratories by using the albumin cobalt binding (ACB) assay or with an enzyme-linked immunosorbent assay (ELISA) (24). Human serum albumin has a binding site at the N-terminus for transition metal ions, such as cobalt, copper and nickel. In acute hypoxic/ischemic conditions, including pulmonary embolism, deep venous thrombosis, acute coronary syndrome, cerebrovascular accidents, skeletal muscle ischemia and systemic sclerosis (25-28), the metal binding capacity of albumin decreases as a result of hypoxia, acidosis, oxidative injury, sodium and calcium pump impairment (29). The first preliminary investigation in patients with intestinal ischemia was published in 2008, and showed that IMA values were significantly higher in seven patients with acute mesenteric ischemia compared to seven healthy subjects (30). These results were then confirmed in another larger clinical study, including 26 patients, 12 with intestinal ischemia (31). The authors reported 1.00 sensitivity and 0.86 specificity for detecting preoperative intestinal ischemia (31). Notably, the peculiar IMA kinetics is characterized by an early increase in parallel with the onset of ischemia, with values then further increase for hours afterwards (32). Dundar et al. showed that rats with intestinal ischemia after superior mesenteric artery ligation had serum IMA levels significantly higher than those without ischemia at 3 and 6 hours after the intervention (33). However, different results were obtained in an experimental study carried out by Uygun and colleagues on 32 Wistar albino rats (34), since IMA levels were not significantly different between ischemia-induced and non-ischemic rats.
α-GST is another biomarker of oxidative stress potentially useful for diagnosing intestinal ischemia (35-37). In the recent meta-analysis of Treskes et al., including 3 studies, the pooled sensitivity and specificity for diagnosing acute intestinal ischemia were 0.68 (95% CI: 0.54–0.80) and 0.84 (95% CI: 0.75–0.91) (10). A relatively satisfactory area under the curve (AUC) could also be obtained (i.e., 0.88±0.05). Since α-GST is involved in intracellular detoxification present in both intestinal and liver cells, the values of this enzyme often increased also in patients with hepatic ischemia (38), thus potentially lowering the diagnostic specificity for acute intestinal ischemia. Moreover, the activity of α-GST can be only measured using ELISA kits so far, which are characterized by a relative long turnaround time and are hence mostly unsuitable for urgent diagnostics.
Inflammatory and/or infection biomarkers
Leukocytosis (i.e., leukocyte count >20×109/L) is commonplace in patients with intestinal ischemia, except in those who are immunocompromised or treated with corticosteroids (1). Due to the low diagnostic specificity for intestinal ischemia, however, leukocytosis is of little help for distinguishing intestinal ischemia from other intestinal non-ischemic disorders (37,39). In a meta-analysis evaluating the performance of several biomarkers for intestinal ischemia, Evennett et al. calculated a 0.80 (95% CI: 0.66–0.91) sensitivity and a very modest 0.50 (95% CI: 0.31–0.69) specificity of white blood cell count for diagnosing intestinal ischemia (7). Matsumoto et al. studied 208 patients with a clinical suspicion of acute intestinal ischemia reported a receiver operating characteristic (ROC) curve for white blood cell count of only 0.54 (95% CI: 0.39–0.70) to distinguish intestinal ischemia from non-ischaemic diseases (40). Thuijls et al. performed leukocyte counts in patients with or without mesenteric ischemia, and failed to find any significant difference between groups 13.9×109/L vs. 12.7×109/L; P=0.89) (19). Unlike these findings, other authors reported that leukocytosis can be considered a potential predictor for transmural bowel necrosis (odds ratio, 1.3, P<0.0001) (41), as well as a significant predictor of mortality (42) in patients with acute mesenteric ischemia.
Additional inflammatory biomarkers, such as C-reactive protein (CRP) or interleukin-6 (IL-6), have been investigated in intestinal ischemia diagnostics. Salem et al. concluded that CRP values tend to increase later than those of IL-6, and the former biomarker seems hence of little help for differentiating non-specific abdominal pain and surgical conditions requiring operative or non-operative intervention (43). Lammers et al. measured IL-6 levels in 15 patients with acute transient intestinal ischemia induced during elective open surgery for treatment of abdominal subrenal aortic aneurysm, and observed a considerable increase of concentration between pre-ischemic condition (i.e., 11.28±3.4 pg/mL) and intestinal ischemia (109±85.9 pg/mL; P<0.002) (44). More recently, Sgourakis et al. studied 14 patients with bowel ischemia and 42 with other abdominal disorders, reporting that IL-6 efficiently discriminate mesenteric ischemia from other pathologies (45). Notably, a IL-6 cut-off of 27.7 pg/mL was characterized by both sensitivity and specificity of 1.00.
Procalcitonin (PCT) is a 116 amino acids protein, prohormone of calcitonin, secreted from liver parenchyma cells and from other sources (including leukocytes) during severe bacterial infections (46). Since the disruption of gut wall integrity after intestinal ischemia potentially leads to the translocation of microbiota and/or their toxic products, the measurement of PCT may be seen as a valuable aid for diagnosing or monitoring intestinal ischemia. Karabulut et al. studied 21 New Zealand rabbits divided into 3 groups of 7 animals each (control, Sham and ischemia groups), reporting that the PCT values increased from the 1st hour after ischemia and thereafter, up to 6 hours (47). Different findings were published in an ensuing study. Karaca et al. induced experimental mesenteric ischemia in rats, and reported that PCT values display a late increase after mesenteric ischemia (i.e., after 6 hours), and can hence be only proposed as a late biomarker (48). Cosse et al. also investigated the role of PCT for discriminating patients with and without intestinal ischemia. In their meta-analysis, including five studies and totaling 659 patients, the AUC for detecting intestinal ischemia was comprised between 0.77–0.92, whilst the sensitivity and specificity ranged between 0.72–1.00 and 0.68–0.91, respectively (49). Notably, the positive and negative predictive values for diagnosing acute intestinal ischemia were also comprised between 0.27–0.90 and 0.81–1.00, respectively. More recently, Cosse et al. studied 128 patients with intestinal ischemia, and reported that PCT values were significantly correlated with intestinal necrotic damage, degree of extension of tissue damage and mortality (50).
Biomarkers of thrombosis
D-dimer, the degradation product of the stabilized fibrin, is a marker of activation of both coagulation and fibrinolysis, and its plasma values hence increases in all those clinical conditions characterized by formation and ensuing dissolution of blood clots (51). Several studies have been published on the diagnostic role of this biomarker in acute intestinal diseases, generating often controversial evidence (52-55). D-dimer was shown to display good diagnostic performance in thrombo-embolic occlusion of the superior mesenteric artery (52,56), but it diagnostic efficiency seems overall less satisfactory in nonvascular acute intestinal ischemia (e.g., strangulated small-bowel obstruction) (57). The sensitivity and specificity of D-dimer for diagnosing strangulated obstruction were found to be 0.60 and 0.68, respectively (57). In another study, Block et al. (37) by investigated 10 patients with intestinal ischemia and 61 without, reporting that a D-dimer concentration >0.9 mg/L was associated with sensitivity, specificity and accuracy of 0.60, 0.82 and 0.79, respectively.
With the aim of summarizing the data published in different studies, three meta-analysis included D-dimer for evaluating biomarkers performance in intestinal ischemia. In a meta-analysis including only 3 studies, D-dimer was characterized by an OR an AUC of 5.77 and 0.53, respectively (7). This diagnostic performance was however lower compared to D-lactate (OR, 10.75; AUC, 0.86, respectively), glutathione S-transferase (OR, 8.82; AUC, 0.87, respectively) and I-FABP (OR, 7.62; AUC, 0.78, respectively). In this same article, the pooled sensitivity and specificity of D-dimer were 0.89 (95% CI: 0.77–0.96) and 0.40 (95% CI: 0.33–0.47) (7).
Cudnik et al. performed another meta-analysis including 5 articles, and calculated a pooled D-dimer sensitivity and specificity of 0.96 (95% CI: 0.89–0.99) and 0.40 (95% CI: 0.33–0.47) (58). More recently, Sun et al. performed a meta-analysis including 12 studies published between the years 2004–2016 and totaling 1,300 patients with suspected acute intestinal ischemia (59). The AUC of D-dimer for diagnosing acute intestinal ischemia was found to be 0.81 (95% CI: 0.78–0.84), whilst the combined sensitivity and specificity were 0.94 (95% CI: 0.87–0.97) and 0.50 (95% CI: 0.40–0.61), respectively. As clearly shown by the results of these three meta-analysis, the diagnostic specificity of D-dimer remains very modest, typically comprised between 0.40 and 0.50. Therefore, the most place use of this biomarker is for ruling out acute intestinal ischemia rather than for making a final diagnosis (7,60).
Biomarkers of gut wall damage and dysfunction
Citrulline (C6H13N3O3), which could be originally identified and isolated from the juice of the watermelon (Citrullus vulgaris) (61), is a non-proteinogenic amino acid synthesized from glutamine by the small bowel enterocytes and is a precursor for de novo synthesis of arginine. After release from enterocytes into the portal circulation, citrulline reaches the systemic circulation and is metabolized by the kidneys, where is converted into arginine and then released into plasma (62). Therefore, the plasma values of citrulline are mostly dependent on gut synthesis and renal metabolism, and are correlated with the enterocyte mass (63,64). It is thus predictable that all clinical conditions characterized by a reduction of enterocyte mass (e.g., short bowel syndrome, villous atrophy diseases, Crohn’s disease, acute mucosal enteropathy and antineoplastic treatments) will be associated with a decreased citrulline plasma concentration (65). Conversely, the plasma values of this biomarker increase in parallel with impaired renal function (66).
The half-life of citrulline is approximately 3 hours and its concentration is not significantly influenced by nutritional status or inflammatory conditions (65,67). Cakmaz et al. recently performed an experimental investigation in 21 Wistar albino rats divided into three groups (control group, short-term ischemia group and prolonged ischemia group), and reported that plasma citrulline values were significantly reduced in short-term and prolonged ischemia groups compared to the control rats (P=0.002), whilst the decrease was also larger in prolonged ischemia compared to short-term ischemia (P=0.011) (68). Kulu et al. studied 48 patients with acute abdominal symptoms (69), and reported that patients with acute mesenteric ischemia (n=23) had citrulline values lower than those with other acute abdominal conditions. Despite the encouraging evidence that has been published, other studies will be needed, however, to fully evaluate the diagnostic accuracy of citrulline in the setting of acute intestinal ischemia.
Since the outer layer of gut consists of smooth muscle cells, a transmural ischemic injury may lead to release of abundantly expressed muscle proteins (70), thus including smooth muscle protein of 22 kDa (SM22), which is known to be involved in maturation and differentiation of smooth muscle cells (71). Schellekens et al. recently developed an ELISA kit for measuring SM22, and showed that the plasma levels of this protein were significantly higher in patients with transmural ischemia (3.7–0.91 ng/mL) than in those with limited mucosal ischemic injury (0.4–0.08 ng/mL; P<0.001) or in healthy controls (0.40–0.07 ng/mL; P<0.001) (72). Notably, the peak concentrations of SM22 was reached after 6 hours, whilst the half-life of the protein was only 23 minutes.
In this same study, the I-FABP, was also measured. This biomarker is a small (12–15 kDa) cytosolic protein of luminal mature enterocytes cells of small intestine and bowel, involved in fatty acid uptake and catabolism. The plasma values of I-FABP levels were found to be significantly increased in both patients with mucosal ischemia and transmural ischemia compared to healthy controls (699–171.4 pg/mL and 952.0–259.2 vs. 217.8–13.6 pg/mL; P<0.05, for both), whilst no significant difference could be observed among patients with mucosal ischemia and transmural ischemia (P=0.77) (72).
A progressively decreasing intestinal perfusion and a loss of integrity of the enterocyte cell membrane both contribute the rapid release of I-FABP into circulation and further elimination by the kidneys (73). I-FABP can hence be measured both in serum (or plasma) and urine (74). I-FABP concentration is very low in the plasma of healthy subjects, but its value significantly increase in blood within 60 minutes after ischemia, which would lead to conclude that the release of this biomarker parallels the onset of ischemia (75).
In a recent meta-analysis including nine studies, Sun et al. calculated obtained an AUC of 0.86 (95% CI: 0.83–0.89) of I-FABP for diagnosing acute intestinal ischemia, with pooled sensitivity and specificity of 0.80 (95% CI: 0.72–0.86) and 0.85 (95% CI: 0.73–0.93), respectively (76).
Treskes and colleagues performed an even more recent meta-analysis, including 13 studies and totaling 1,435 patients (10). Merging data obtained using two different methods, the diagnostic performance was found to be better using the Uden kit (0.79 sensitivity and 0.91 specificity) compared to the Osaka kit (0.75 sensitivity and 0.79 specificity).
Conclusions
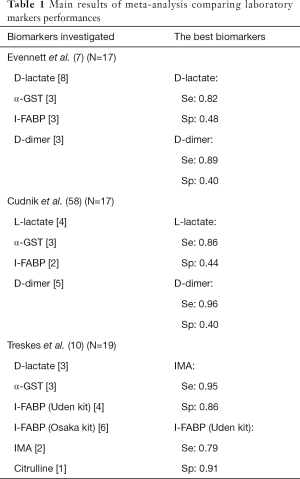
Although acute intestinal ischemia remains a relative rare condition, a timely and accurate diagnosis is needed to prevent the development of serious complications, up to death. A vast array of laboratory biomarkers has been evaluated in the diagnosis of acute intestinal ischemia (Table 1), but an ideal biomarker (i.e., rapid, stable, highly specific and sensitive, inexpensive and easy to be measured) is still seemingly missing.
Full table
Among the various tests, D-lactate, IMA and I-FABP are perhaps the most promising, since they are characterized by optimal sensitivity and relatively acceptable specificity, early kinetics, and can be measured with assays suited for rapid diagnosis. Yet, additional studies will be needed to assess whether any of these three biomarkers will soon be ready for being introduced into routine clinical practice.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Oldenburg WA, Lau LL, Rodenberg TJ, et al. Acute mesenteric ischemia: a clinical review. Arch Intern Med 2004;164:1054-62. [Crossref] [PubMed]
- Schoots IG, Koffeman GI, Legemate DA, et al. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. Br J Surg 2004;91:17-27. [Crossref] [PubMed]
- Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M, et al. Identification of risk factors for preoperative mortality in acute mesenteric ischemia. World J Surg 2006;30:1579-85. [Crossref] [PubMed]
- Bala M, Kashuk J, Moore EE, et al. Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World J Emerg Surg 2017;12:38. [Crossref] [PubMed]
- Peoc'h K, Nuzzo A, Guedj K, et al. Diagnosis biomarkers in acute intestinal ischemic injury: so close, yet so far. Clin Chem Lab Med 2018;56:373-85. [Crossref] [PubMed]
- Patel A, Kaleya RN, Sammartano RJ. Pathophysiology of mesenteric ischemia. Surg Clin North Am 1992;72:31-41. [Crossref] [PubMed]
- Evennett NJ, Petrov MS, Mittal A, et al. Systematic review and pooled estimates for the diagnostic accuracy of serological markers for intestinal ischemia. World J Surg 2009;33:1374-83. [Crossref] [PubMed]
- Powell A, Armstrong P. Plasma biomarkers for early diagnosis of acuteintestinal ischemia. Semin Vasc Surg 2014;27:170-5. [Crossref] [PubMed]
- Acosta S, Nilsson T. Current status on plasma biomarkers for acute mesenteric ischemia. J Thromb Thrombolysis 2012;33:355-61. [Crossref] [PubMed]
- Treskes N, Persoon AM, van Zanten ARH. Diagnostic accuracy of novel serological biomarkers to detect acute mesenteric ischemia: a systematic review and meta-analysis. Intern Emerg Med 2017;12:821-36. [Crossref] [PubMed]
- Derikx JP, Schellekens DH, Acosta S. Serological markers for human intestinal ischemia: A systematic review. Best Pract Res Clin Gastroenterol 2017;31:69-74. [Crossref] [PubMed]
- Lange H, Jäckel R. Usefulness of plasma lactate concentration in the diagnosis of acute abdominal disease. Eur J Surg 1994;160:381-4. [PubMed]
- Acosta S, Block T, Björnsson S, et al. Diagnostic pitfalls at admission in patients with acute superior mesenteric artery occlusion. J Emerg Med 2012;42:635-41. [Crossref] [PubMed]
- Kowlgi NG, Chhabra L. D-lactic acidosis: an underrecognized complication of short bowel syndrome. Gastroenterol Res Pract 2015;2015. [Crossref] [PubMed]
- Nutz V, Sommer HJ. Hyperlactacidemia in intestinal ischemia. I. Theoretical considerations Langenbecks Arch Chir 1987;370:63-8. (in German). [Crossref] [PubMed]
- Janda A, Hagmuller GW, Denck H. Lactate in the diagnosis of acute intestinal vascular occlusions Chirurg 1984;55:469-73. (in German). [PubMed]
- Kurimoto Y, Kawaharada N, Ito T, et al. An experimental evaluation of the lactate concentration following mesenteric ischemia. Surg Today 2008;38:926-30. [Crossref] [PubMed]
- Aydin B, Ozban M, Serinken M, et al. The place of D-dimer and L-lactate levels in the early diagnosis of acute mesenteric ischemia. Bratisl Lek Listy 2015;116:343-50. [PubMed]
- Thuijls G, van Wijck K, Grootjans J, et al. Early diagnosis of intestinal ischemia using urinary and plasma fatty acid binding proteins. Ann Surg 2011;253:303-8. [Crossref] [PubMed]
- Demir IE, Ceyhan GO, Friess H. Beyond lactate: is there a role for serum lactate measurement in diagnosing acute mesenteric ischemia? Dig Surg 2012;29:226-35. [Crossref] [PubMed]
- de Vrese M, Koppenhoefer B, Barth CA. D-lactic acid metabolism after an oral load of DL-lactate. Clin Nutr 1990;9:23-8. [Crossref] [PubMed]
- Ewaschuk JB, Naylor JM, Zello GA. D-lactate in human and ruminant metabolism. J Nutr 2005;135:1619-25. [Crossref] [PubMed]
- Isfordink CJ, Dekker D, Monkelbaan JF. Clinical value of serum lactate measurement in diagnosing acute mesenteric ischaemia. Neth J Med 2018;76:60-4. [PubMed]
- Lippi G, Montagnana M, Salvagno GL, et al. Standardization of ischemia-modified albumin testing: adjustment for serum albumin. Clin Chem Lab Med 2007;45:261-2. [Crossref] [PubMed]
- Lippi G, Montagnana M, Salvagno GL, et al. Potential value for new diagnostic markers in the early recognition of acute coronary syndromes. CJEM 2006;8:27-31. [Crossref] [PubMed]
- Montagnana M, Lippi G, Regis D, et al. Evaluation of cardiac involvement following major orthopedic surgery. Clin Chem Lab Med 2006;44:1340-6. [Crossref] [PubMed]
- Dominguez-Rodriguez A, Abreu-Gonzalez P. Current role of ischemia-modified albumin in routine clinical practice. Biomarkers 2010;15:655-62. [Crossref] [PubMed]
- Montagnana M, Lippi G, Volpe A. Set al. Evaluation of cardiac laboratory markers in patients with systemic sclerosis. Clin Biochem 2006;39:913-7. [Crossref] [PubMed]
- Lippi G, Montagnana M, Guidi GC. Albumin cobalt binding and ischemia modified albumin generation: an endogenous response to ischemia? Int J Cardiol 2006;108:410-1. [Crossref] [PubMed]
- Gunduz A, Turedi S, Mentese A, et al. Ischemia modified albumin in the diagnosis of acute mesenteric ischemia: a preliminary study. Am J Emerg Med 2008;26:202-5. [Crossref] [PubMed]
- Polk JD, Rael LT, Craun ML, et al. Clinical utility of the cobalt-albumin binding assay in the diagnosis of intestinal ischemia. J Trauma 2008;64:42-5. [Crossref] [PubMed]
- Gunduz A, Turkmen S, Turedi S, et al. Time-dependent variations in ischemia-modified albumin levels in mesenteric ischemia. Acad Emerg Med 2009;16:539-43. [Crossref] [PubMed]
- Dundar ZD, Cander B, Gul M, et al. Serum ischemia-modified albumin levels in an experimental acute mesenteric ischemia model. Acad Emerg Med 2010;17:1233-8. [Crossref] [PubMed]
- Uygun M, Yilmaz S, Pekdemir M, et al. The diagnostic value of ischemia-modified albumin in a rat model of acute mesenteric ischemia. Acad Emerg Med 2011;18:355-9. [Crossref] [PubMed]
- Delaney CP, O'Neill S, Manning F, et al. Plasma concentrations of glutathione S-transferase isoenzyme are raised in patients with intestinal ischaemia. Br J Surg 1999;86:1349-53. [Crossref] [PubMed]
- Gearhart SL, Delaney CP, Senagore AJ, et al. Prospective assessment of the predictive value of alpha-glutathione S-transferase for intestinal ischemia. Am Surg 2003;69:324-9. [PubMed]
- Block T, Nilsson TK, Björck M, et al. Diagnostic accuracy of plasma biomarkers for intestinal ischaemia. Scand J Clin Lab Invest 2008;68:242-8. [Crossref] [PubMed]
- Choukér A, Martignoni A, Schauer RJ, et al. Alpha-gluthathione S-transferase as an early marker of hepatic ischemia/reperfusion injury after liver resection. World J Surg 2005;29:528-34. [Crossref] [PubMed]
- Sise MJ. Mesenteric ischemia: the whole spectrum. Scand J Surg 2010;99:106-10. [Crossref] [PubMed]
- Matsumoto S, Sekine K, Funaoka H, et al. Diagnostic performance of plasma biomarkers in patients with acute intestinal ischaemia. Br J Surg 2014;101:232-8. [Crossref] [PubMed]
- Emile SH. Predictive Factors for Intestinal Transmural Necrosis in Patients with Acute Mesenteric Ischemia. World J Surg 2018;42:2364-72. [Crossref] [PubMed]
- Paladino NC, Inviati A, Di Paola V, et al. Predictive factors of mortality in patients with acute mesenteric ischemia. A retrospective study. Ann Ital Chir 2014;85:265-70. [PubMed]
- Salem TA, Molloy RG, O'Dwyer PJ. Prospective study on the role of C-reactive protein (CRP) in patients with an acute abdomen. Ann R Coll Surg Engl 2007;89:233-7. [Crossref] [PubMed]
- Lammers KM, Innocenti G, Venturi A, et al. The effect of transient intestinal ischemia on inflammatory parameters. Int J Colorectal Dis 2003;18:78-85. [Crossref] [PubMed]
- Sgourakis G, Papapanagiotou A, Kontovounisios C, et al. The value of plasma neurotensin and cytokine measurement for the detection of bowel ischaemia in clinically doubtful cases: a prospective study. Exp Biol Med (Maywood) 2013;238:874-80. [Crossref] [PubMed]
- Lippi G, Sanchis-Gomar F. Procalcitonin in inflammatory bowel disease: Drawbacks and opportunities. World J Gastroenterol 2017;23:8283-90. [Crossref] [PubMed]
- Karabulut K, Gül M, Dündar ZD, et al. Diagnostic and prognostic value of procalcitonin and phosphorus in acute mesenteric ischemia. Ulus Travma Acil Cerrahi Derg 2011;17:193-8. [Crossref] [PubMed]
- Karaca Y, Gündüz A, Türkmen S, et al. Diagnostic Value of Procalcitonin Levels in Acute Mesenteric Ischemia. Balkan Med J 2015;32:291-5. [Crossref] [PubMed]
- Cosse C, Sabbagh C, Kamel S, et al. Procalcitonin and intestinal ischemia: a review of the literature. World J Gastroenterol 2014;20:17773-8. [Crossref] [PubMed]
- Cosse C, Sabbagh C, Browet F, et al. Serum value of procalcitonin as a marker of intestinal damages: type, extension, and prognosis. Surg Endosc 2015;29:3132-9. [Crossref] [PubMed]
- Lippi G, Franchini M, Targher G, et al. Help me, Doctor! My D-dimer is raised. Ann Med 2008;40:594-605. [Crossref] [PubMed]
- Acosta S, Björck M. Acute thrombo-embolic occlusion of the superior mesenteric artery: a prospective study in a well defined population. Eur J Vasc Endovasc Surg 2003;26:179-83. [Crossref] [PubMed]
- Tan WW, Zhang M. Clinical value of D-dimer for early diagnosis and severity of ischemic bowel disease. Lab Med Clin 2016;13:1497-9.
- Icoz G, Makay O, Sozbilen M, et al. Is D-dimer a predictor of strangulated intestinal hernia? World J Surg 2006;30:2165-9. [Crossref] [PubMed]
- Güzel M, Sözüer EM, Salt Ö, et al. Value of the serum I-FABP level for diagnosing acute mesenteric ischemia. Surg Today 2014;44:2072-6. [Crossref] [PubMed]
- Acosta S, Nilsson TK, Björck M. D-dimer testing in patients with suspected acute thromboembolic occlusion of the superior mesenteric artery. Br J Surg 2004;91:991-4. [Crossref] [PubMed]
- Bogusevicius A, Grinkevicius A, Maleckas A, et al. The role of D-dimer in the diagnosis of strangulated small-bowel obstruction. Medicina 2007;43:850-4. [Crossref] [PubMed]
- Cudnik MT, Darbha S, Jones J, et al. The diagnosis of acute mesenteric ischemia: a systematic review and meta-analysis. Acad Emerg Med 2013;20:1087-100. [Crossref] [PubMed]
- Sun DL, Li SM, Cen YY, et al. Accuracy of using serum D-dimer for diagnosis of acute intestinal ischemia: A meta-analysis. Medicine (Baltimore) 2017;96. [Crossref] [PubMed]
- Yang S, Fan X, Ding W, et al. D-dimer as an early marker of severity in patients with acute superior mesenteric venous thrombosis. Medicine (Baltimore) 2014;93. [Crossref] [PubMed]
- Mandel H, Levy N, Izkovitch S, et al. Elevated plasma citrulline and arginine due to consumption of Citrullus vulgaris (watermelon). J Inherit Metab Dis 2005;28:467-72. [Crossref] [PubMed]
- Curis E, Nicolis I, Moinard C, et al. Almost all about citrulline in mammals. Amino Acids 2005;29:177-205. [Crossref] [PubMed]
- Fragkos KC, Forbes A. Citrulline as a marker of intestinal function and absorption in clinical settings: A systematic review and meta-analysis. United European Gastroenterol J 2018;6:181-91. [Crossref] [PubMed]
- Piton G, Manzon C, Monnet E, et al. Plasma citrulline kinetics and prognostic value in critically ill patients. Intensive Care Med 2010;36:702-6. [Crossref] [PubMed]
- Crenn P, Messing B, Cynober L. Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin Nutr 2008;27:328-39. [Crossref] [PubMed]
- Lau T, Owen W, Yu YM, et al. Arginine, citrulline, and nitric oxide metabolism in end-stage renal disease patients. J Clin Invest 2000;105:1217-25. [Crossref] [PubMed]
- Curis E, Crenn P, Cynober L. Citrulline and the gut. Curr Opin Clin Nutr Metab Care 2007;10:620-6. [Crossref] [PubMed]
- Cakmaz R, Büyükaşık O, Kahramansoy N, et al. A combination of plasma DAO and citrulline levels as a potential marker for acute mesenteric ischemia. Libyan J Med 2013;8:1-6. [Crossref] [PubMed]
- Kulu R, Akyildiz H, Akcan A, et al. Plasma citrulline measurement in the diagnosis of acute mesenteric ischaemia. ANZ J Surg 2017;87:E57-60. [Crossref] [PubMed]
- Lees-Miller JP, Heeley DH, Smillie LB, et al. Isolation and characterization of an abundant and novel 22-kDa protein (SM22) from chicken gizzard smooth muscle. J Biol Chem 1987;262:2988-93. [PubMed]
- Solway J, Seltzer J, Samaha FF, et al. Structure and expression of a smooth muscle cell-specific gene, SM22 alpha. J Biol Chem 1995;270:13460-9. [Crossref] [PubMed]
- Schellekens DHSM, Reisinger KW, Lenaerts K, et al. SM22 a Plasma Biomarker for Human Transmural Intestinal Ischemia. Ann Surg 2018;268:120-6. [PubMed]
- Gollin G, Marks C, Marks WH. Intestinal fatty acid binding protein in serum and urine reflects early ischemic injury to the small bowel. Surgery 1993;113:545-51. [PubMed]
- Khadaroo RG, Fortis S, Salim SY, et al. I-FABP as biomarker for the early diagnosis of acute mesenteric ischemia and resultant lung injury. PLoS One 2014;9. [Crossref] [PubMed]
- Schellekens DH, Grootjans J, Dello SA, et al. Plasma intestinal fatty acid binding protein levels correlate with morphologic epithelial intestinal damage in a human translational ischemia-reperfusion model. J Clin Gastroenterol 2014;48:253-60. [Crossref] [PubMed]
- Sun DL, Cen YY, Li SM, et al. Accuracy of the serum intestinal fatty-acid binding protein for diagnosis of acute intestinal ischemia: a meta-analysis. Sci Rep 2016;6:34371. [Crossref] [PubMed]


