Full spectrum endoscopy for an easy and adequate visualization of Vater’s papilla
Introduction
Patients with classical familial adenomatous polyposis (FAP) should undergo screening for proximal small bowel tumors. Standard (i.e., forward-viewing) upper gastrointestinal (GI)-endoscopy does not allow an adequate examination of the duodenum, especially of the peri-ampullary region; therefore, complementary use of side-viewing endoscopes is mandatory, as visible ampullary lesions require histological assessment (1). A novel Full-Spectrum Endoscopy® (FUSE®) (EndoChoice Inc., Atlanta, GA, USA) esophagogastroduodenoscope (EGD), that provides a high-definition 245° field of view with two imagers on the front and left side of the endoscope, has been recently introduced. This endoscope allows the endoscopist to perform a forward-viewing examination with an adequate visualization of the ampullary region. Here we report the case of a male patient with FAP, who underwent upper GI endoscopy with the FUSE-EGD system.
Case presentation
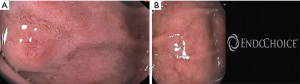
A 20-year-old Caucasian male patient, who underwent prophylactic colectomy 5 years ago because of classical FAP, was referred to our facility for upper GI screening. For this purpose, we used the FUSE-EGD, which allowed an adequate visualization of Vater’s papilla with an easy maneuverability (Figure 1). The endoscopist who performed the procedure reported that the FUSE-EGD was superior to standard forward-viewing endoscope in terms of diagnostic accuracy. No adverse event occurred.
Discussion
Classical FAP is an autosomal dominant disease caused by mutations in the Adenomatous Polyposis Coli (APC) gene. It is characterized by the presence of hundreds of colorectal adenomas and is also associated to extracolonic manifestations. The malignant potential of colorectal adenomas evolves rapidly over time and since all patients with FAP will eventually develop colorectal cancer (CRC), prophylactic colectomy, which is considered the treatment of choice in these patients, should be performed in their second decade of life (2).
Aside from the worrisome CRC risk, duodenal adenomas can also be found in about 50–90% of FAP patients. They usually occur in the ampullary or periampullary area, presenting as flat, whitish, small lesions (<5 mm), difficult to differentiate from the surrounding normal mucosa (3). Although the malignant degeneration of duodenal adenomas is usually slower compared to colonic lesions (adenoma-carcinoma sequence may take up to 15–20 years), endoscopists performing duodenal examination should accurately identify and assess duodenal lesions (1,2). Particular attention should be paid to the detection of large (>1 cm) lesions, as they have been shown to have foci of high-grade dysplasia in up to 50% of patients, and this significantly increases the syndrome’s malignant potential (4).
Current guidelines suggest periodical upper GI screening, with the first endoscopic examination to be performed at 25–30 years. Adequate screening should include the evaluation of gastric mucosa with a forward-viewing gastroscope, followed by a side-viewing duodenoscopy in order to ensure an optimal duodenal examination (1,2).
However, the endoscopic examination of duodenum can be tricky; indeed, evaluation of the ampulla can be difficult either because of anatomical reasons (e.g., narrow lumen) or complex maneuverability of the side-viewing endoscope, is time-consuming and painful for the patient. Moreover, it is associated with increased peri-procedural costs, and duodenoscopes are not always available in most endoscopy units. Lastly, concerns about the cleanliness of duodenoscopes have been recently raised. Therefore, in light of what stated above, it is of main importance to use an endoscope that allows adequate and easy visualization of the duodenum and the ampullary region (5).
The advent of a novel endoscopic platform, Full Spectrum Endoscopy® (FUSE®, EndoChoice Inc., Atlanta, Georgia, USA) that allows a panoramic field of view (245° for gastroscope, 330° for colonoscope), led to a revolution in the examination of GI regions that were previously considered as “invisible”, such as the proximal side of colonic folds/flexures (6). It has been shown in literature that FUSE is superior to conventional colonoscopy, as it is associated to a reduction in overall and proximal colorectal adenoma miss rates (7,8). Similarly, the new upper GI endoscope represents a sophisticated technical innovation, as it allows an accurate inspection of both gastric and duodenal mucosa (including the peri-ampullary region) in a single procedure (9). However, FUSE technology has a limitation, which may negatively influence its widespread use. Such limitation is represented by high costs, which may be difficult to afford as, currently, there are many financial barriers and limited economic resources in the endoscopic field (10).
In conclusion, FAP patients require periodical endoscopic examination for the risk of duodenal adenomas. A combination of forward- and side-viewing endoscopy is necessary to ensure an adequate inspection of the duodenal mucosa. FUSE-EGD represents a potential alternative, as it combines two procedures in one, thus increasing the accuracy and acceptability of upper GI screening in FAP patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Syngal S, Brand RE, Church JM, et al. ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol 2015;110:223-62. [Crossref] [PubMed]
- Vasen HF, Moslein G, Alonso A, et al. Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut 2008;57:704-13. [Crossref] [PubMed]
- Saurin JC, Pioche M, Rivory J. Surveillance of duodenal adenomas in familial adenomatous polyposis patients: medical objectives and technical requirements. Endosc Int Open 2015;3:E456-7. [Crossref] [PubMed]
- Groves CJ, Saunders BP, Spigelman AD, et al. Duodenal cancer in patients with familial adenomatous polyposis (FAP): results of a 10 year prospective study. Gut 2002;50:636-41. [Crossref] [PubMed]
- Gralnek IM. Evaluation of the EndoChoice full spectrum endoscopy (Fuse) platform for upper endoscopy and colonoscopy Expert Rev Med Devices 2016;13:313-9. [Crossref] [PubMed]
- Gkolfakis P, Tziatzios G, Dimitriadis GD, et al. New endoscopes and add-on devices to improve colonoscopy performance. World J Gastroenterol 2017;23:3784-96. [Crossref] [PubMed]
- Papanikolaou IS, Apostolopoulos P, Tziatzios G, et al. Lower adenoma miss rate with FUSE vs. conventional colonoscopy with proximal retroflexion: a randomized back-to-back trial. Endoscopy 2017;49:468-75. [Crossref] [PubMed]
- Ratone JP, Bories E, Caillol F, et al. Impact of Full Spectrum Endoscopy® (Fuse®, EndoChoice®) on adenoma detection: a prospective French pilot study. Ann Gastroenterol 2017;30:512-7. [PubMed]
- Kakushima N, Takizawa K, Tanaka M, et al. A novel wide viewing endoscope for upper gastrointestinal screening: a pilot study. Endosc Int Open 2016;4:E190-2. [Crossref] [PubMed]
- Triantafyllou K, Gkolfakis P, Viazis N, et al. A 13-year time trend analysis of 3724 small bowel video capsule endoscopies and a forecast model during the financial crisis in Greece. Eur J Gastroenterol Hepatol 2017;29:185-91. [Crossref] [PubMed]


