Aspirin and diabetes mellitus in primary prevention: the Endless Conundrum
Cardiovascular disease is the leading cause of morbidity and mortality in our societies (1). The rupture of an atherosclerotic plaque may result in the creation of a thrombus that can generate an acute infarction (2).
A drug with an intense antiplatelet effect would have a significant impact in morbi-mortality. In this context, low dose aspirin (LDA) has been the cornerstone for treatment of coronary artery disease during the last 35 years. LDA has been an example of the success of translational research. Starting with the publication of its pharmacodynamics, thromboxane (TX) B2 inhibition, to a large number of adequately sized, placebo-controlled clinical trials (3).
The effectiveness of LDA in clinical practice is based on several studies that have shown the saturability of LDA in the general population, even with doses of 30–40 mg/day and the dose dependence of its side effects (mainly bleeding complications).
LDA has been evaluated in a large number of clinical trials from healthy persons (primary prevention) to high-risk patients presenting an acute myocardial event or an acute cerebrovascular event (secondary prevention).
Regarding the secondary prevention of cardiovascular disease, the evidence of LDA is solid. The proportional reduction of events was not different between primary and secondary randomized trials (4), but the absolute risk reduction was higher in secondary vs. primary prevention. LDA reduced vascular mortality, yielding a reduction of 1% of acute coronary events. LDA significantly reduced the aggregate of all strokes in the secondary prevention randomized trials and also was able to reduce a 10% reduction in total mortality (4).
Regarding the primary prevention of cardiovascular events, the Anti-Thrombotic Trialists (ATT) included the first six primary-prevention trials (4-10). LDA induced a significant reduction in cardiovascular events (stroke, myocardial infarction or vascular death) of 0.06% per year. This result was mainly the effect of a reduction in nonfatal myocardial infarction of 0.05 per year. Stroke and vascular mortality were not reduced. On the other hand, LDA treatment increased gastrointestinal bleeds of 0.04 per year. Another important point showed by this meta-analysis was that risk factors for coronary events are also risk factors for bleeding.
In the current situation where the modifiable risk factors are treated more aggressively (active life styles, cholesterol control or use of statins, smoke cessation, obesity control, hypertension and drug prescription, optimal treatment of diabetes mellitus (DM), heart failure and atrial fibrillation) the absolute benefits and hazards of LDA versus previous interventions are likely to be approximately evenly balanced.
With these premises, The Japanese Primary Prevention of Atherosclerosis with Aspirin for Diabetes (JPAD) trial was a randomized, open-label trial with the objective to evaluate if LDA was able to reduced cardiovascular events in Japanese patients with type 2 DM and without pre-existing cardiovascular disease (11). Previous subgroups analysis had evaluated the effect of LDA in DM with divergent results (4,6,9,12).
Two thousand five hundred thirty-nine patients were randomly allocated to receive LDA or no aspirin. The conclusion of this study published in 2008 was that LDA once a day was not able reduce the risk of cardiovascular events in this population. Interestingly, the haemorrhagic complications (stroke and gastrointestinal) were not significantly different between both groups (11). The ratio of cardiovascular events in this study was low, probably due to a lower incidence of cardiovascular disease in this Japanese population (lower body mass index among others modifiable factors).
Four meta-analysis published in the last years included patients of higher risk (periphery artery disease and/or diabetes) based in three additional trials. These meta-analyses concluded that LDA was not able to reduce significantly the incidence of stroke, cardiovascular and all-cause mortality and coronary heart disease (9,12-16). Some authors have argued that to effect of heterogeneity, these results are not comparable to what has been previously published by the ATTs (9,11,12).
After the end of the JPAD study, the patients were followed until 2015 and the results (JPAD2) of this research is here commented as editorial. The primary end points were cardiovascular events (fatal and not fatal), the same in the first study published in 2008. Haemorrhagic complications, gastrointestinal bleeding and haemorrhagic stroke were also evaluated. The analysis was performed as per-protocol cohort. Analyses on an intention-to-treat cohort were also performed (17).
The follow-up was more than 10 years for the JPAD2 vs. 4.37 years for the JPAD. Sixth-four percent of the original patients were followed throughout the study and the conclusion was that LDA was not able reduce cardiovascular events in the per-protocol cohort. Adjusted Multivariable Cox proportional hazard model showed the same results. The incidence of gastrointestinal bleeding was doubled in the LDA vs. the placebo group.
The interest of JPAD2 trial was that there is no study analysing the effect of aspirin in a population of DM with such a long follow-up. Other trial, like the Women’s Health Study present a follow-up of 10 years, but the prevalence of DM was less than 3%.
Some limitations should be acknowledge, like the fact that we cannot consider this publication as a randomized controlled trial, but an observational continuation of a randomized trial.
It should be noted that the authors modified the definition of a bleeding event. In the JPAD trial, a significant bleeding event was considered as the composite of haemorrhagic stroke and severe GI bleeding. In the JPAD2 study, all haemorrhagic events (gastrointestinal bleeding, haemorrhagic stroke, and bleeding from any other sites) were considered bleeding events. If we analyse the data of JPAD2 in the per protocol cohort, the number of GI bleeding in the LDA group is limited to 12 episodes (1.2%), and the same number in the group of non-LDA (1%), P=0.7. In the same way, if we annotate all GI bleeding events of the JPAD, we observe 12 events in the LDA group vs. 4 in the non-LDA group. In this case, the primary analysis based on the per-protocol principle vs. intention-to-treat has the same result, but it is not the case when we analyse the GI bleeding complications and also if we modify the definition of bleeding (Table 1). In resume, the authors maintained the end point and the interpretation (per-protocol) but changed the definition of GI and the interpretation of the bleeding complications (intention-to-treat).

Full table
The justification of these findings is based in an increase platelet turnover in the DM population (18-20). The duration of platelet COX-1 inhibition is shortened, with a probably recovery of the platelet capacity to synthesize TXA2 during the 24 h dosing interval. In this context, it has been recommended to prescribe aspirin twice per day in this population. In the obese population, a higher degradation and a decrease absorption is probably present, resulting in a lower concentration of the drug and secondary a lower inhibition of COX-1 enzyme. It should be noted that in many cases, both mechanism can be present at the same time due to the high incidence of obesity in DM patients.
As commented before, due to the fact that the modifiable risk factors are treated more aggressively the incidence of cardiovascular events is very low. In this context the number of patients needed to find differences between groups should be much higher than the studies performed 30 years ago.
These results are in the same direction of other three randomized trials (9,12,17). LDA was not able to reduce the risk of cardiovascular events in any subgroups of patients divided by sex, with or without DM or in the total group of patients with high risks factors of cardiovascular disease. With all these data, the level of evidence (LOE) of LDA in the recent guidelines is LOE C or expert consensus LOE E, and only in high risk patients (21).
It should be noted the effect of LDA in the prevention of cancer. Three meta-analyses showed the effect of LDA in the prevention of cancer (22-24). LDA treatment reduced risk of cancer with distant metastasis, mainly due to a reduction of adenocarcinomas linked to metastatic disease (20). These publications point that LDA would be able to help in treatment of cancers and to prevent metastasis.
To help the clinician to optimize the use of LDA, Table 2 that shows eight strategies to optimize de use of aspirin and decrease the risk of bleeding in the primary prevention of cardiovascular disease in patients with DM.
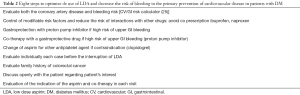
Full table
In conclusion, in this study even in patients with atherosclerotic risk factors and DM, LDA was unable to show any benefit in primary prevention of cardiovascular events. The number of GI bleeding events is higher, but if we analyse it in relation to the per protocol cohort, the bleeding incidence is the same. On the other hand, some evidence points that LDA may be of benefit in prevention of colorectal cancer. Through analysis of this study and other primary prevention ongoing trials such as ACCEPT-D, ASCEND, ARRIVE, ASPREE, the scientific community will eventually be able to determine the overall benefit of aspirin in primary prevention of adverse health-related events.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Word Health Organization. Available online: http://www.who.int/en/. last accessed in May 2015 [homepage on the Internet].
- Patrono C, García Rodríguez LA, Landolfi R, et al. Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med 2005;353:2373-83. [Crossref] [PubMed]
- Patrignani P, Filabozzi P, Patrono C. Selective cumulative inhibition of platelet thromboxane production by low-dose aspirin in healthy subjects. J Clin Invest 1982;69:1366-72. [Crossref] [PubMed]
- Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009;373:1849-60. [Crossref] [PubMed]
- Peto R, Gray R, Collins R, et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed) 1988;296:313-6. [Crossref] [PubMed]
- Steering Committee of the Physicians' Health Study Research Group. Preliminary report: Findings from the aspirin component of the ongoing Physicians' Health Study. N Engl J Med 1988;318:262-4. [Crossref] [PubMed]
- Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. The Medical Research Council's General Practice Research Framework. Lancet 1998;351:233-41. [Crossref] [PubMed]
- Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 1998;351:1755-62. [Crossref] [PubMed]
- de Gaetano G. Collaborative Group of the Primary Prevention Project. Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice. Collaborative Group of the Primary Prevention Project. Lancet 2001;357:89-95. [Crossref] [PubMed]
- Ridker PM, Cook NR, Lee IM, et al. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005;352:1293-304. [Crossref] [PubMed]
- Ogawa H, Nakayama M, Morimoto T, et al. Low-dose aspirin for primary prevention of atherosclerotic events in patients with type 2 diabetes: a randomized controlled trial. JAMA 2008;300:2134-41. [Crossref] [PubMed]
- Sacco M, Pellegrini F, Roncaglioni MC, et al. Primary prevention of cardiovascular events with low-dose aspirin and vitamin E in type 2 diabetic patients: results of the Primary Prevention Project (PPP) trial. Diabetes Care 2003;26:3264-72. [Crossref] [PubMed]
- Fowkes FG, Price JF, Stewart MC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA 2010;303:841-8. [Crossref] [PubMed]
- Belch J, MacCuish A, Campbell I, et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. BMJ 2008;337:a1840. [Crossref] [PubMed]
- Bartolucci AA, Tendera M, Howard G. Meta-analysis of multiple primary prevention trials of cardiovascular events using aspirin. Am J Cardiol 2011;107:1796-801. [Crossref] [PubMed]
- Raju N, Sobieraj-Teague M, Hirsh J, et al. Effect of aspirin on mortality in the primary prevention of cardiovascular disease. Am J Med 2011;124:621-9. [Crossref] [PubMed]
- Berger JS, Lala A, Krantz MJ, et al. Aspirin for the prevention of cardiovascular events in patients without clinical cardiovascular disease: a meta-analysis of randomized trials. Am Heart J 2011;162:115-24.e2. [Crossref] [PubMed]
- Seshasai SR, Wijesuriya S, Sivakumaran R, et al. Effect of aspirin on vascular and nonvascular outcomes: meta-analysis of randomized controlled trials. Arch Intern Med 2012;172:209-16. [Crossref] [PubMed]
- Ikeda Y, Shimada K, Teramoto T, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA 2014;312:2510-20. [Crossref] [PubMed]
- Patrono C, Rocca B. Type 2 Diabetes, Obesity, and Aspirin Responsiveness. J Am Coll Cardiol 2017;69:613-5. [Crossref] [PubMed]
- Fox CS, Golden SH, Anderson C, et al. Update on Prevention of Cardiovascular Disease in Adults With Type 2 Diabetes Mellitus in Light of Recent Evidence: A Scientific Statement From the American Heart Association and the American Diabetes Association. Diabetes Care 2015;38:1777-803. [Crossref] [PubMed]
- Rothwell PM, Wilson M, Price JF, et al. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet 2012;379:1591-601. [Crossref] [PubMed]
- Mills EJ, Wu P, Alberton M, et al. Low-dose aspirin and cancer mortality: a meta-analysis of randomized trials. Am J Med 2012;125:560-7. [Crossref] [PubMed]
- Algra AM, Rothwell PM. Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol 2012;13:518-27. [Crossref] [PubMed]
- Lanas A, Polo-Tomás M, Casado-Arroyo R. The aspirin cardiovascular/gastrointestinal risk calculator--a tool to aid clinicians in practice. Aliment Pharmacol Ther 2013;37:738-48. [Crossref] [PubMed]


