Monitoring of colonoscopy quality indicators in an academic endoscopy facility reveals adherence to international recommendations
Introduction
Colonoscopy is the most widely used examination for colorectal cancer (CRC) screening and follow-up. Given its ability to remove pro-malignant lesions, it has significantly reduced the incidence and the mortality of CRC (1). That being the case, a low detection rate of these lesions could increase the risk for a subsequent CRC. At the same time, variations among endoscopists in the performance of colonoscopy have been documented (2,3), indicating the need of measuring quality in colonoscopy and optimizing its effectiveness, when needed.
Several societies such as European Society of Gastrointestinal Endoscopy (ESGE), the American College of Gastroenterology (ACG), and the American Society for Gastrointestinal Endoscopy (ASGE) have proposed more than 40 quality indicators (4-6) for colonoscopy. The most widely used quality indicator for screening endoscopy, adenoma detection rate (ADR), defined as the proportion of screening colonoscopies that detect at least one adenoma has been correlated with the risk for interval cancers (2). Other important key quality indicators are cecal intubation rate (minimum standard: ≥90%), rate of adequate bowel preparation (minimum standard: ≥90%), complication rate (minimum standard: ≤0.5% for 7-day readmission rate) and withdrawal time (minimum standard: mean 6 min) (4,5). Sedation administration rate (SAR) is also used as a quality indicator since there is evidence that it correlates with higher patient satisfaction and procedural quality (7,8).
Measuring and improving lower gastrointestinal (LGI) endoscopy performance gives the opportunity for self-improvement for each endoscopist individually and for applying plans to optimize facility’s service (9).
The aim of this audit was the measurement of four quality indicators—SAR, colonoscopy completion rate (CCR), ADR and early complications rate (CR)—in all colonoscopies performed in an academic endoscopy facility in Athens, Greece during 2013 and 2015.
Methods
Design and definitions
Retrospective analyses of four quality indicators—SAR, CCR, ADR and CR—in colonoscopies performed during 2013 and 2015, respectively. Data were retrieved from our facility’s records.
We define SAR as the proportion of colonoscopies with intravenous sedation-analgesia administration, CCR as the proportion of colonoscopies where cecum or terminal ileum was intubated or the anastomosis after resection was reached, ADR as the proportion of colonoscopies with at least one histologically confirmed adenoma and early CR as the proportion of colonoscopies associated with complications occurring during colonoscopy or until discharge.
We used three patients’ cohorts (A, B and C) in order to run separate investigations for each quality indicator in different populations. Cases with intention for total colonoscopy constituted cohort A, whereas cohort A excluding cases with bowel obstruction comprised cohort B. Cohort C included CRC screening cases (asymptomatic subjects aged 50 years or older without personal or family history of colorectal neoplasia (in case of family history of colorectal neoplasia, the age limit was lowered, accordingly) within cohort B.
Different quality indicators measurements were applied in each cohort: we assessed reasons for incomplete colonoscopy and measured SAR and CR in cohort A, we measured SAR, CR and CCR in cohort B and finally, we measured all four indicators in cohort C.
Participating endoscopists were aware of the upcoming internal evaluation. The head of the facility disclosed the results of endoscopists performance, individually. In addition, a special meeting of the staff was held to present and discuss the overall performance of the facility.
Population and procedures
The selected quality indicators are measured and recorded in all procedures that intend to visualize the whole colon at the endoscopy facility of the Hepatogastroenterology Unit of Attikon University General Hospital in Athens, Greece.
Colonoscopies were performed daily, by or under the supervision of experienced gastroenterologists. Trainee participation occurred routinely, but not always; trainees started the examination and proceeded until no further progression. A consultant took over in these cases.
Procedures were performed using Olympus CF-Q145L or CF-Q165L standard-definition white-light colonoscopes (Olympus Corporation, Tokyo, Japan) after bowel preparation with 4 L of polyethylene glycol. Bowel preparation quality was characterized as adequate (excellent/good) or inadequate (fair/poor) for the right (caecum, ascending, and transverse) and the left (descending, sigmoid, and rectum) colon, separately, using a modified Boston bowel preparation scale (BBPS) (10).
Vital signs, such as heart rate, arterial blood pressure and oxygen saturation, and level of consciousness were monitored during the examination. Supplemental oxygen was routinely delivered via nasal catheters. Intravenous conscious sedation (midazolam) and analgesia (pethidine) was administered on demand. Flumazenil and/or naloxone were used to reverse sedation/analgesia, if needed.
Endpoints
The primary endpoint of the study was the overall measurement of the four quality indicators during the studied periods.
Secondary endpoint was the measurement of individual endoscopist performance during the audited periods.
Ethical considerations
This audit being part of continuous quality improvement program required neither Institutional Review Board approval nor specific informed consent (data retrieved from patients’ records were de-identified). However, patients provided standard informed consent before colonoscopy.
Statistical analysis
Continuous variables are presented as means (standard deviations) or medians (interquartile range). Binary variables are reported as percentages with corresponding 95% confidence intervals (CI) using normal approximation (Wald) test. For percentages ranging between 0–1, the Clopper-Pearson exact test was used to calculate their 95% CI. Non-parametric tests were used to detect differences, as appropriate. A P value less than 0.05 indicated a statistical significance.
Results
During the audited periods, 3,707 colonoscopies were performed in our facility. After excluding referrals for polypectomy and cases in which there was no intention for whole colon examination, 1,016 and 1,213 exams were included in the analysis for the years 2013 and 2015, respectively. These cases comprised cohort A. and their baseline characteristics are listed in Table 1. Trainees either initiated or performed the colonoscopy under the supervision of a senior endoscopist in 70.8% and 70.3% of the cases for the audited periods. The main indication for the procedures was symptoms evaluation for both periods; however a significant increase in the number of CRC screening cases was apparent in 2015. According to the ASA classification (11), there were significantly less cases with severe comorbidities in 2015 and according to the modified BBPS scale used in our facility, there were significantly more cases with adequate bowel preparation in 2015 as compared to 2013. The distribution of incomplete colonoscopy etiologies was similar among the two periods; however, there were significantly more complete colonoscopy cases in 2015. After excluding the cases with bowel obstruction due to tumor or severe inflammation, there remained 999 and 1,207 cases for the years 2013 and 2015 comprising cohort B. Among them there were 262 and 415 CRC screening cases (cohort C) for the same years.

Full table
Primary endpoint outcomes
Table 2 tabulates the primary endpoints outcomes according to the period of evaluation. In 2015, SAR surpassed the level of 90 in cohort A. and this rate remained over 90% in cohorts B and C, as well.

Full table
CCRs in cohorts B and C were higher than the recommended levels (90% and 95%, respectively) in both studied periods, although the lower CI of CCR in 2013 was just below 95% in cohort C. A significant increase of CCR was detected in 2015 (98.1% vs. 94.8%, P<0.0001) compared to 2013 only in cohort B.
ADR was similar [27.1% (21.7–32.5%) and 27% (22.7–31.3%)] in the two audited periods. When splitting ADR results according to patients gender, ADR was higher than 30% in males only in 2015 [39.4% (32.1–46.8%)], while the lower CI of the indicator did not reach this margin [33.8% (25.8–41.9%) ] in 2013. For females, ADR was not constantly over 20% [20.2% (13.2–27.1%) and 18.4% (13.6–23.3%) for years 2013 and 2015, respectively].
CR was 0.1% in the two periods. There was one cardiopulmonary event reversed with ventilation and pharmacological interventions in 2013 and one surgically managed perforation in 2015. No complication occurred in cohort C. and no death occurred, as well.
Trainee involvement had no significant effect on the colonoscopy quality indicators during the two periods.
Secondary endpoint outcomes
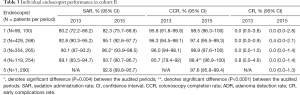
One of the participating endoscopist was hired at the end of 2013; therefore his performance has been measured only for 2015. Another endoscopist performed colonoscopies only during the first half of 2013 and another one practiced colonoscopies during the last trimester of this year. All five endoscopists performed colonoscopies in 2015. Given these remarks, the number of procedure performed by endoscopist was quite variable during the first period, while it was more homogeneous in 2015 when four out of five endoscopists performed or supervised more than 200 colonoscopies each (cohort A). There was also significant (P<0.0001) variability regarding trainees’ participation in senior endoscopists lists (cohort A) ranging from 53.3% to 85.8% in 2013 and from 54.9% to 85.9% in 2015.
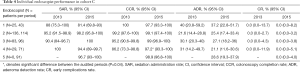
Variability among endoscopists regarding the four quality indicators during the study periods was also evident, as shown in Tables 3 and 4. SAR exhibited significant variability in cohorts B (80–96%) and C (81–100%) in the two periods. This variability is attributed to one endoscopist who offers unsedated colonoscopy to almost 20% of the patients.
Full table
Full table
CCR was less variable among endoscopists in cohorts B and C. and the only endoscopist with low performance in 2013 significantly (P<0.04) improved in 2015.
ADR was highly variable among endoscopist in 2013 (ranging from 21.6% to 40%) and in 2015 (ranging from 21.1% to 37.2%). There was no difference between the endoscopists regarding ADR in males and females in 2013 (P>0.3) and in 2015 (P>0.18), respectively.
The two early complications were observed in procedures performed by two different endoscopist.
Discussion
Our audit demonstrates that overall, our Academic endoscopic facility offers high quality service regarding the endoscopic examination of the large bowel by reaching and maintaining the internationally defined standards of certain quality indicators. Nevertheless, there is some variability among individual endoscopists’ performance indicating that there is still room for improvement.
ADR is considered the most important indicator, reflecting the quality level of LGI endoscopy (12,13). In our facility, the overall mean ADR remained above the proposed by ESGE and ASGE level of 25% in both audited periods.
Beyond ADR, colonoscopy completion is of paramount importance for high performers. In both audited periods, CCR in cohorts B and C was above the recommended performance targets (all examinations ≥90%, screening ≥95%) by ASGE (14). However, according to ESGE guidelines there should be no difference of the cecal intubation rate among screening and routine examinations and the target standard for both should be at least 95% (4). On top of that, a recently published study from Norway that reported CCRs above 97% in all categories, concludes that CCRs were similar among screening and routine colonoscopies and suggested the use of one target standard for better adherence to the guidelines (15). Indeed, our audit showed that apart from 2013 cohort B cases our CCR exceeded 95%, overall.
Another significant audit finding was the very low early complication rate. Moreover, there was no complication in screening exams and there was need for surgical intervention in only one case.
Adequate sedation is a factor that determines patient satisfaction and may improve endoscopist’s comfort during colonoscopy (16). While sedation carries low risks for cardiopulmonary events, it is a costly option and requires time, facilities and personnel to monitor patients until recovery (17). SAR in both periods and in all cohorts was constantly higher than 90%, a target proposed by the Hellenic Foundation of Gastroenterology and Nutrition (18). However, it’s worthily to mention that one of the two recorded early complications was related to sedation administration.
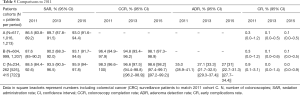
When trying to informally compare this audit results with those previously reported for the year 2011 (9), as shown Table 5, overall SAR increased numerically in 2013 and significantly in 2015, as compared to that of 2011. At the same time CCR was similar in the three audited period in cohorts B and C, respectively. Although at a glance ADR is declining, when corrected to include CRC surveillance cases in order to match the definition of cohort C in 2011, it is obvious that the results are unchanged. Finally, although low in all audited periods, the rate of early complications is at least numerically lower in the current audit.
Full table
Quality indicators have advantages and disadvantages in their application in clinical practice. The major disadvantage of ADR calculation is that it requires histology. Thus, other pathology-independent indices are warranted. In this context British researchers proposed the Performance Indicator of Colonic Intubation (PICI) as an effective tool that combines CCR, patient’s comfort and level of sedation (19) to better assess colonoscopy quality. While there is evidence that PICI correlates with polyp detection rate in screening colonoscopy cases, there is no evidence that it can replace ADR, yet.
Regarding the secondary study endpoint, our key finding as depicted in Tables 3 and 4 is the endoscopists’ variability, with the exception of CCRs where low (≤5%) inter endoscopists’ differences were detected. Moreover, there the only low performer in 2013 significantly improved CCR in 2015. Our finding is in contrast to recent studies reporting variable CCRs among endoscopists (ranging from less than 80% to over 90%) and it seems that experience and annual procedure numbers are the most influential factors for high CCRs (20,21).
Both SAR and ADR were quite variable among participating endoscopists in our audit. A huge variability in SAR has been reported among colonoscopists: 0–63.0% of patients receiving no sedation (22) and 4.1–100% of patients undergoing sedated colonoscopy (23). Similarly, high variability among endoscopists of the same unit has also been reported regarding ADR per endoscopist ranging from 21.9% to 59.8% (22).
The major advantage of our study is the continuous measurement of our colonoscopy quality performance. Our study limitations are the lack of measurement of additional quality indicators, such as colonoscope withdrawal time, which is proposed as key indicator, the relatively small number of colonoscopies overall and more specifically of the CRC screening exams, the lack of adjusting the results according to the endoscopists experience and the annual number of cases per endoscopist and the single center setting.
In conclusion, our facility adheres to the international minimum standards of LGI endoscopy providing efficient screening and routine colonoscopy services. The results reveal potential targets for performance optimization, particularly in individual level.
Acknowledgements
We would like to thank Dr. Ioannis Panayiotides, Professor of Pathology and Head of the 2nd Pathology Department, Medical School, National and Kapodistrian University of Athens, at Attikon University Hospital, Athens, Greece, for his contribution to the audit.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This audit being part of continuous quality improvement program required neither Institutional Review Board approval nor specific informed consent (data retrieved from patients’ records were de-identified). However, patients provided standard informed consent before colonoscopy.
References
- Zauber AG, Winawer SJ, Obrien MJ, et al. Colonoscopic Polypectomy and Long-Term Prevention of Colorectal-Cancer Deaths. N Engl J Med 2012;366:687-96. [Crossref] [PubMed]
- Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 2010;362:1795-803. [Crossref] [PubMed]
- Butterly L, Robinson CM, Anderson JC, et al. Serrated and adenomatous polyp detection increases with longer withdrawal time: results from the New Hampshire Colonoscopy Registry. Am J Gastroenterol 2014;109:417-26. [Crossref] [PubMed]
- Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. United European Gastroenterol J 2017;5:309-34. [Crossref] [PubMed]
- Cohen J, Pike IM. Defining and measuring quality in endoscopy. Gastrointest Endosc 2015;81:1-2. [Crossref] [PubMed]
- Endoscopy Unit Quality Indicator Taskforce ASGE, Day LW, Cohen J, et al. Quality indicators for gastrointestinal endoscopy units. VideoGIE 2017;2:119-40. [Crossref] [PubMed]
- Wang D, Chen C, Chen J, et al. The Use of Propofol as a Sedative Agent in Gastrointestinal Endoscopy: A Meta-Analysis. PLoS One 2013;8. [Crossref] [PubMed]
- Bannert C, Reinhart K, Dunkler D, et al. Sedation in screening colonoscopy: impact on quality indicators and complications. Am J Gastroenterol 2012;107:1837-48. [Crossref] [PubMed]
- Triantafyllou K, Sioulas AD, Kalli T, et al. Optimized sedation improves colonoscopy quality long-term. Gastroenterol Res Pract 2015;2015. [Crossref] [PubMed]
- Calderwood AH, Jacobson BC. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc 2010;72:686-92. [Crossref] [PubMed]
- American Society of Anesthesiologists. ASA Physical status classification system. Available online: www.asahq.org/resources/clinical-information/asa-physical-status-classification-system, last accessed 01 November 2017.
- Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370:1298-306. [Crossref] [PubMed]
- Kaminski MF, Wieszczy P, Rupinski M, et al. Increased rate of adenoma detection associates with reduced risk of colorectal cancer and death. Gastroenterology 2017;153:98-105. [Crossref] [PubMed]
- Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015;81:31-53. [Crossref] [PubMed]
- Hoff G, Holme Ø, Bretthauer M, et al. Cecum intubation rate as quality indicator in clinical versus screening colonoscopy. Endosc Int Open 2017;5:E489-95. [Crossref] [PubMed]
- Lin OS. Sedation for routine gastrointestinal endoscopic procedures: a review on efficacy, safety, efficiency, cost and satisfaction. Intest Res 2017;15:456-66. [Crossref] [PubMed]
- Leung FW, Aljebreen AM, Brocchi E, et al. Sedation-risk-free colonoscopy for minimizing the burden of colorectal cancer screening. World J Gastrointest Endosc 2010;2:81-9. [Crossref] [PubMed]
- Paspatis GA, Manolaraki MM, Tribonias G, et al. Endoscopic sedation in Greece: results from a nationwide survey for the Hellenic Foundation of Gastroenterology and Nutrition. Dig Liver Dis 2009;41:807-11. [Crossref] [PubMed]
- Valori RM, Damery S, Gavin DR, et al. A new composite measure of colonoscopy: the Performance Indicator of Colonic Intubation (PICI). Endoscopy 2018;50:40-51. [PubMed]
- Cotton PB, Connor P, McGee D, et al. Colonoscopy: practice variation among 69 hospital-based endoscopists. Gastrointest Endosc 2003;57:352-7. [Crossref] [PubMed]
- Harewood GC. Relationship of colonoscopy completion rates and endoscopist features. Dig Dis Sci 2005;50:47-51. [Crossref] [PubMed]
- Lee TJ, Rutter MD, Blanks RG, et al. Colonoscopy quality measures: experience from the NHS Bowel Cancer Screening Programme. Gut 2012;61:1050-7. [Crossref] [PubMed]
- Ball AJ, Rees CJ, Corfe BM, et al. Sedation practices and comfort during colonoscopy: lessons learnt from a national screening programme. Eur J Gastroenterol Hepatol 2015;27:741-6. [Crossref] [PubMed]


