Teeth infection may “shunt” through Fontan in high-altitude conditions
Introduction
The Fontan surgery is the last staged operation for children with congenital heart disease who are not candidates for a 2-ventricle repair (1). When this procedure is performed at high altitudes, the chronic alveolar hypoxia increases pulmonary vascular resistance (PVR) leading to an increase in the right to left shunt (2). The success of this operation depends in large part on this resistance, and any factor that increases PVR will ultimately lead to a negative impact on Fontan hemodynamics (3) and to a steep rise in long-term complications.
The Fontan surgery involves the creation a conduit between the inferior vena cava and the right pulmonary artery. This conduit has a small fenestration that shunts the blood from the Fontan to the right atrium in case the pulmonary blood flow is limited increasing the preload of the systemic ventricle, at the expense of lowering the systemic oxygenation and the risks that involves the right to left shunt (i.e., embolism, systemic infection) (4).
Theoretically an increase in PVR associated with high altitude will increase the shunt through the Fontan fenestration to the right atrium and then to the systemic ventricle. Normal brushing of teeth increases the number of bacteria in the bloodstream, thus they can bypass the pulmonary circulation and get access to the systemic circulation leading to severe infections. In the literature there are many described complications of the Fontan, however, there is no description of teeth infection shunting to the brain when the patients are exposed to high altitude for a long term (5). We report a case of a patient with brain abscess associated with Streptococcus gordonii, bacteria of the normal flora of the teeth and dental plaque.
Case presentation
An 11-year old patient living in a high-altitude city in Colombia; previously known in our institution with a history of tricuspid atresia with normally related great arteries and large ventricular septal defect without pulmonary stenosis, who had undergone a fenestrated extracardiac Fontan surgery in 2010. In 2017 he presented to the emergency department with a 2-week history of headache, vomiting and fever. The parents emphasized that the patient was not the same and that during the day he developed short episodes of depersonalization and disorientation, he was on furosemide 20 mg/day, spironolactone 25 mg/day and warfarin 5 mg/day. On physical examination, he had two of the classic Cushing triad; his blood pressure was 128/85 (over 99th percentile for age), heart rate was 38 beats/min, respiratory rate was normal at 18 breaths/min, oxygen saturation was 75% while breathing ambient air, and body temperature was 36.5 °C. He was alert, oriented and had no signs of neurological deficit and dental exam revealed two dental cavities in molar teeth and signs of dental caries. Owing to the risk of bleeding (i.e., anticoagulation) and the neurological symptoms referred by the parents, the patient was admitted for further studies.
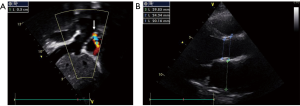
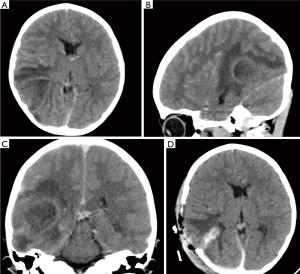
The complete blood count (CBC) revealed a white blood cell count of 13,800/µL with left deviation (84.5% of neutrophils). The C-reactive protein level was 1.11 mg/dL and the erythrocyte sedimentation rate was 2 mm/h, the international normalized ratio (INR) was 1.35. The echocardiogram revealed a dilated left ventricle with a mild decrease in ejection fraction of 55% with right to left shunt from the extracardiac Fontan to the right atrium through the fenestration without evidence of intracardiac infection (i.e., abscess) or vegetations (Figure 1A,B). Computed tomography (CT) scan showed a large mass over the occipital and parietal lobe with left ventricle compression and left midline shift (Figure 2A,B,C). With the suspicion of a pyogenic abscess versus parenchymal hemorrhage, we covered the patient with vancomycin and cefepime and discontinued anticoagulation. Considering the risk of neurological deterioration, we took the patient to surgery.
Under general anesthesia; a right occipital and parietal incision was made and a craniotomy was performed with high speed CRANIO-Blade; an approximate of 40 mL intra-axial liquid mass with profuse exudate was drained; unfortunately, the bone could not be marsupialized due to the extended infection.
The pus was sent to the microbiology laboratory for culture. A blood agar at 37 °C in ambient air, showed the growth of small non-hemolytic colonies after 72 hours of incubation. The isolation was identified as Streptococcus gordonii with the Microgen ® Strep ID Panel. Antimicrobial susceptibility was done with the modified Kirby-Bauer test, the microorganism minimum inhibitory concentrations where >8 for erythromycin (Resistant), 0.06 for penicillin (Intermediate) and 2 for Ceftriaxone (Intermediate).
A repeated CT scan (Figure 2D) was performed after the surgery. It showed a significant reduction in the midline shift and compression of left ventricle. The patient blood cultures were negative at 7 days of incubation. After the antibiotic panel result, we de-escalated to Vancomycin 400 mg intravenous (IV) every 6 hours for 42 days. The levels of Vancomycin remained at 19.43 µg/mL and the clinical response was excellent. The patient underwent molar extraction and dental capping of compromised teeth.
Discussion
Brain abscess is a serious and life-threatening clinical entity, due to the spread from a contiguous focus of infection like hematogenous seeding from a distant source (6). The diagnosis of brain abscess is considered definite if bacterial organisms are isolated from abscess pus or cerebral spinal fluid cultures. The isolated organisms vary with underlying medical or surgical conditions. In this case confirmation of abscess has come about upon CT scan findings characteristic of brain abscess and bacterial growth from the pus culture.
The Streptococcus viridans group readily colonizes the dental plaque and it has been described as a potential etiology of brain abscess. This group is composed of several species, and particularly the S. anginosus group species are usually isolated from brain abscesses (7). In our case we reported Streptococcus gordonii as the isolate; to date, it has not been described as the etiology of brain abscess in the context of Congenital Heart Disease. This specie has the same potential to colonize the dental plaque as Streptococcus sanguinis (8). Other viridans group bacteria isolated from brain abscesses had been described in patients with Congenital Heart Disease (9); highlighting the importance of dental care in patients with right to left shunt diseases.
Our theory is that the patient was colonized with Streptococcus gordonii, and probably tooth brushing or previous dental procedures disrupted the surface of gingival tissue and caused bacteremia (10). All these bacteria bypassed through the Fontan fenestration to the right atrium and then to the systemic circulation. Although it has been reported that immunosuppressed patients are the population at risk of having Streptococcus viridans brain abscess (11), we assume that in the context of congenital heart disease with Fontan palliation the regular seeding of bacteria in the brain can lead to chronic infections (Figure 3).
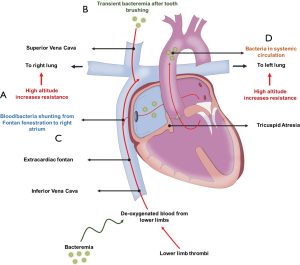
Unique physiological changes caused by Fontan circulation include a single-ventricle circulation, passive venous flow to the lungs instead of the normal pulsatile lung perfusion, systemic venous hypertension, and scarring in the heart (12). Thus, there is a concern about the negative impact that chronic teeth infection and altitude may have on the outcome of the Fontan procedure. Since low PVR is a major criterion for the successful creation of a Fontan circulation and high-altitude may rise PVR in response to reduction in the partial pressure of oxygen (3) we conclude that dental infections associated with increased altitude altered Fontan hemodynamics can lead to severe infections. We ought to provide the patients the recommendation of living in low altitude cities and keep an excellent dental hygiene.
Acknowledgements
The authors thank all the medical staff involved in patient care.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the mother of the patient included in the study.
References
- D’Udekem Y, Iyengar AJ, Cochrane AD, et al. The Fontan procedure: contemporary techniques have improved long-term outcomes. Circulation 2007;116:I157-64. [Crossref] [PubMed]
- Day RW, Orsmond GS, Sturtevant JE, et al. Early and intermediate results of the Fontan procedure at moderately high altitude. Ann Thorac Surg 1994;57:170-6. [Crossref] [PubMed]
- Johnson JT, Lindsay I, Day RW, et al. Living at altitude adversely affects survival among patients with a Fontan procedure. J Am Coll Cardiol 2013;61:1283-9. [Crossref] [PubMed]
- Lemler MS, Scott WA, Leonard SR, et al. Fenestration improves clinical outcome of the fontan procedure: a prospective, randomized study. Circulation 2002;105:207-12. [Crossref] [PubMed]
- Mehrotra A, Khanna P, Kumar S, et al. Renal abscess after the Fontan procedure: a case report. J Med Case Rep 2011;5:50. [Crossref] [PubMed]
- Patel K, Clifford DB. Bacterial brain abscess. Neurohospitalist 2014;4:196-204. [Crossref] [PubMed]
- Doern CD, Burnham CA. It's not easy being green: the viridans group streptococci, with a focus on pediatric clinical manifestations. J Clin Microbiol 2010;48:3829-35. [Crossref] [PubMed]
- Zheng W, Tan MF, Old LA, et al. Distinct Biological Potential of Streptococcus gordonii and Streptococcus sanguinis Revealed by Comparative Genome Analysis. Sci Rep 2017;7:2949. [Crossref] [PubMed]
- Solanki R, Subramanian S, Lakshmi V, et al. Brain abscess due to Streptococcus oralis in an immunocompetent patient. Indian J Med Microbiol 2014;32:179-80. [Crossref] [PubMed]
- Lockhart PB, Brennan MT, Sasser HC, et al. Bacteremia associated with toothbrushing and dental extraction. Circulation 2008;117:3118-25. [Crossref] [PubMed]
- Vidal JE, Tuon FF. Brain abscess due to viridans streptococci in a severely immunosuppressed HIV-infected patient. Int J STD AIDS 2009;20:654-6. [Crossref] [PubMed]
- McRae ME. Long-term issues after the Fontan procedure. AACN Adv Crit Care 2013;24:264-82. [Crossref] [PubMed]


