Incretin-based therapy and pancreatitis: accumulating evidence and unresolved questions
Incretin-based therapy consists of two different classes of medication: glucagon-like peptide-1 (GLP-1) receptor agonists (GLP-1 RAs) and dipeptidyl peptidase-4 (DPP-4) inhibitors. Since the approval of exenatide, the first GLP-1 RA, and sitagliptin, the first DPP-4 inhibitor, by the U.S. Food and Drug Administration (FDA) in 2005 and 2006, respectively, incretin-based therapy is becoming a major option for the treatment of type 2 diabetes (T2DM) (1). While DPP-4 inhibitors enhance endogenous incretin [GLP-1 and glucose-dependent insulinotropic polypeptide (GIP)] action, GLP-1 RAs stimulate the GLP-1 receptor at a supra-physiological level. Since both agents enhance glucose-dependent insulin secretion and also suppress glucagon secretion in a glucose-dependent manner, the risk of hypoglycemia is very low unless they are combined with sulfonylureas, glinides or insulin. In addition, GLP-1 RAs, but not DPP-4 inhibitors, suppress gastric emptying and satiety, thereby inducing weight reduction. Recent cardiovascular outcome trials (CVOTs) have shown that GLP-1 RAs, liraglutide and semaglutide, improved CV outcomes in patients with T2DM and high CV risk (2,3). Liraglutide has also been shown to improve renal outcome (4). Based on these results, the American Diabetes Association (ADA) states that therapy with liraglutide should be considered for patients with T2DM and atherosclerotic cardiovascular disease (ASCVD) (5).
Incretin-based therapy has generally been well-tolerated with few serious adverse events, although gastrointestinal symptoms are commonly seen in subjects treated with GLP-1 RAs, which usually resolve spontaneously 2 to 4 weeks after the initiation of therapy. However, a rare but serious adverse event associated with incretin-based therapy is acute pancreatitis (AP).
After marketing of incretin-based drugs, cases of AP have been reported and the FDA has ordered a warning label (6,7). Several cohort studies suggested increased risk of AP with incretin-based therapies (8,9), and this subject has been extensively discussed (10,11). Although pooled analysis of phase 3 trials has shown no excess risk of AP with incretin-based therapy (12), the number of events was small.
In 2017, a meta-analysis of three CVOTs of DPP-4 inhibitors including 18,238 patients treated with DPP-4 inhibitors and 18,157 placebo-treated patients has been reported (13), showing increased risk of AP with treatment with DPP-4 inhibitors (odds ratio =1.79; 95% CI, 1.13–2.82; P=0.013). On the other hand, a meta-analysis of three CVOTs of GLP-1 RAs showed no excess risk of AP compared with placebo (14). Therefore, it is under debate whether DPP-4 inhibitors and GLP-1 RAs have different risk profiles of AP.
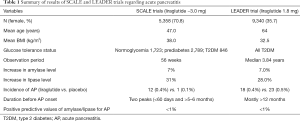
Recently, Steinberg et al. have provided new evidence regarding liraglutide and the risk of AP (15,16). They conducted a secondary analysis of pooled data from the Satiety and Clinical Adiposity-Liraglutide Evidence in individuals with and without diabetes (SCALE) clinical development program (15). The analysis included four randomized, placebo-controlled trials comprising the SCALE phase 3a clinical trial program of liraglutide 3.0 mg for weight management (n=5,358 with BMI ≥30, or 27 to <30 kg/m2 with ≥1 comorbid condition). Of these, 1,723 subjects had normoglycemia, 2,789 had prediabetes and 846 had T2DM. Participants were randomized to liraglutide 3.0 mg (n=3,302), liraglutide 1.8 mg (n=211, only T2DM) or placebo (n=1,845). Subjects with a history of idiopathic AP or chronic pancreatitis were excluded from the SCALE program. Relationships between serum amylase/lipase activity at baseline and during treatment and events of AP were investigated.
Over 56 weeks, liraglutide 3.0 mg versus placebo was associated with a 7% increase in mean level of amylase and a 31% increase in mean level of lipase activity. Similar changes in amylase/lipase levels were observed with liraglutide 1.8 mg. However, few subjects had elevations to 3 times the upper limit of normal (ULN) for amylase or lipase (<0.1% and 2.9% with liraglutide 3.0 mg), and the enzymes returned to baseline levels after liraglutide discontinuation. Twelve participants developed AP during (n=9, 0.3%) or after (n=3, 0.1%) liraglutide 3.0 mg treatment versus one (0.1%) with placebo, all of whom were from SCALE Trial 1. Five of 12 AP cases with liraglutide 3.0 mg had gallstone disease evident at AP onset. Amylase/lipase elevations before AP onset showed very low positive predictive value for AP (<1%).
Strengths of the study include a prospective, randomized, controlled study design with a large sample size and relatively long duration of follow-up. Amylase/lipase activity was measured regularly, and the diagnosis of AP was adjudicated by an independent, blinded committee.
Accompanying this paper, a sub-analysis of the LEADER (Liraglutide Effect and Action in Diabetes: Evaluation of cardiovascular outcome Results) trial regarding relationships between amylase/lipase levels and AP onset in patients with T2DM treated with liraglutide 1.8 mg has been reported in the same issue of Diabetes Care (16). The LEADER trial included a total of 9,340 patients with T2DM and high CV risk randomized to either liraglutide or placebo with median follow-up of 3.84 years. During the study, 18 (0.4%) liraglutide-treated and 23 (0.5%) placebo patients developed AP confirmed by adjudication. Prior history of pancreatitis did not increase the risk of AP onset after liraglutide treatment. Compared with the placebo group, liraglutide-treated patients had increases in serum amylase and lipase of 7.0% and 28.0%, respectively. Similar to the analysis of the SCALE trial, elevations of amylase and lipase levels did not predict future risk of AP in patients treated with liraglutide.
These results provide a clearer picture of the association between liraglutide and AP onset. First, liraglutide increases serum amylase/lipase levels by approximately 7% and 30%, respectively, in a dose-independent manner, irrespective of the presence or absence of diabetes. Second, the increases in amylase/lipase levels are seen as early as 4 weeks after introducing liraglutide therapy. Third, the increases in amylase/lipase levels are reversible after discontinuing the therapy. Fourth, the elevations of amylase/lipase levels are not predictive of AP onset.
Although elevations of amylase/lipase levels with GLP-1 RAs therapy were confirmed by these studies, the mechanisms by which GLP-1 RAs increase these serum enzyme levels remain unclear. Recent studies have shown that the GLP-1 receptor is weakly expressed in acinar cells (17) and, in mice, GLP-1 increases amylase secretion from acinar cells (18,19). A study in mice also has shown that 4 weeks of GLP-1 treatment increases protein synthesis in acinar cells and pancreatic mass, reflecting an increase in acinar cell mass without changes in ductal compartments or beta cell mass (20). Therefore, GLP-1 may enhance acinar cell protein synthesis including amylase and lipase. However, the effects of GLP-1 on exocrine function and pancreatic morphology have not been confirmed in non-human primates or humans (21-25). Another hypothesis is that GLP-1 increases the permeability of the basolateral membrane of acinar cells, resulting in enhanced transfer of pancreatic enzymes into blood, which needs further investigation.
The other mechanism of AP onset in patients with incretin-based therapy is gallstone-related pancreatitis. Increased incidence of gallbladder-related adverse events such as cholelithiasis and acute cholecystitis have been reported in patients treated with GLP-1 RA therapy (26) and also in both the LEADER and SCALE trials (2,27). Since GLP-1 suppresses gastrointestinal movement, gallbladder and biliary tract motility may also be suppressed by GLP-1, leading to gallstone formation (28). Weight loss and change in food components after GLP-1 RA therapy may also contribute to production of gallstones. The relatively longer duration between initiation of GLP-1 RA therapy and onset of AP seems to be consistent with this hypothesis, and indeed 50% of AP was attributable to gallstones in the SCALE program (15).
The results of pancreatic enzymes in the SCALE and LEADER trials seem almost identical and complementary (Table 1). However, a striking difference is that the incidence of AP was numerically increased with liraglutide therapy in the SCALE trials (15), while it was comparable between the liraglutide and placebo groups in the LEADER trial (2). It can be assumed that the different doses of liraglutide (1.8 vs. 3.0 mg) might affect the incidence of AP. Since a higher dose (3.0 mg) of liraglutide is aimed at weight loss, the effects of GLP-1 on gastrointestinal motility including the gallbladder and biliary tract, weight loss and change in food components, all of which could contribute to gallstone synthesis, may be exaggerated compared with those with 1.8 mg of liraglutide. These factors might accelerate the production of gallstones, resulting in the increased incidence of AP seen in the SCALE program.
Full table
Thus, gallstone-related pancreatitis might explain the different incidence of AP between the two trials. However, it does not seem to explain the increased risk of AP related to DPP-4 inhibitors, since DPP-4 inhibitors do not usually affect gastrointestinal motility or induce weight loss. The use of DPP-4 inhibitors does not appear to increase gallbladder-related adverse events (26), and inconsistent results regarding changes in serum amylase/lipase levels after the use of DPP-4 inhibitors have been reported (29-33) (Table 2).

Full table
Because the increased risk of AP was originally reported in patients treated with sitagliptin or exenatide, and the proinflammatory/proliferative effects of GLP-1 on the exocrine pancreas have been suggested as the mechanism of AP onset with incretin-based therapy (34-36), AP has been thought to be a common adverse event with incretin-based therapy. However, recent meta-analyses have shown that the incidence of AP is in fact increased in patients treated with DPP-4 inhibitors, but not with GLP-1 RAs (13,14). Inhibition of DPP-4 affects not only GLP-1 level but also various other substrates including GIP, cytokines, growth factors and neuropeptides. DPP-4 (also namely CD26) is also expressed on the surface of T cells (37). Thus, DPP-4 inhibitors may affect the immune system and tissue inflammation. Recently, the development of bullous pemphigoid (BP) in patients treated with DPP-4 inhibitors has been reported (38). This adverse event may be associated with genetic factors (39). Thus, the increased risk of AP in patients treated with DPP-4 inhibitors could also be associated with inflammatory response within the pancreas predisposed by genetic factors.
Accumulating evidence has shed light on the different risk profiles of AP onset between DPP-4 inhibitors and GLP-1 RAs. The mechanisms by which DPP-4 inhibitors and GLP-1 RAs increase the risk of AP may be different, and further investigation is needed to clarify this unresolved question.
Acknowledgements
The author thanks Dr. Wendy Gray, self-employed, for editing the manuscript.
Footnote
Conflicts of Interest: Y Saisho has received honoraria from Takeda Pharmaceutical Company, Boehlinger Ingelheim and AstraZeneca, and research funding from AstraZeneca.
References
- Nauck MA, Meier JJ. The incretin effect in healthy individuals and those with type 2 diabetes: physiology, pathophysiology, and response to therapeutic interventions. Lancet Diabetes Endocrinol 2016;4:525-36. [Crossref] [PubMed]
- Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 2016;375:311-22. [Crossref] [PubMed]
- Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 2016;375:1834-44. [Crossref] [PubMed]
- Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and Renal Outcomes in Type 2 Diabetes. N Engl J Med 2017;377:839-48. [Crossref] [PubMed]
- American Diabetes Association. 8. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018;41:S73-S85. [Crossref] [PubMed]
- Parks M, Rosebraugh C. Weighing risks and benefits of liraglutide--the FDA's review of a new antidiabetic therapy. N Engl J Med 2010;362:774-7. [Crossref] [PubMed]
- Egan AG, Blind E, Dunder K, et al. Pancreatic Safety of Incretin-Based Drugs — FDA and EMA Assessment. N Engl J Med 2014;370:794-7. [Crossref] [PubMed]
- Elashoff M, Matveyenko AV, Gier B, et al. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology 2011;141:150-6. [Crossref] [PubMed]
- Singh S, Chang HY, Richards TM, et al. Glucagonlike peptide 1-based therapies and risk of hospitalization for acute pancreatitis in type 2 diabetes mellitus: a population-based matched case-control study. JAMA Intern Med 2013;173:534-9. [Crossref] [PubMed]
- Nauck MA. A critical analysis of the clinical use of incretin-based therapies: The benefits by far outweigh the potential risks. Diabetes Care 2013;36:2126-32. [Crossref] [PubMed]
- Butler PC, Elashoff M, Elashoff R, et al. A critical analysis of the clinical use of incretin-based therapies: Are the GLP-1 therapies safe? Diabetes Care 2013;36:2118-25. [Crossref] [PubMed]
- Meier JJ, Nauck MA. Risk of pancreatitis in patients treated with incretin-based therapies. Diabetologia 2014;57:1320-4. [Crossref] [PubMed]
- Tkac I, Raz I. Combined Analysis of Three Large Interventional Trials With Gliptins Indicates Increased Incidence of Acute Pancreatitis in Patients With Type 2 Diabetes. Diabetes Care 2017;40:284-6. [Crossref] [PubMed]
- Nauck MA, Meier JJ, Schmidt WE. Incretin-based glucose-lowering medications and the risk of acute pancreatitis and/or pancreatic cancer: Reassuring data from cardio-vascular outcome trials. Diabetes Obes Metab 2017;19:1327-8. [Crossref] [PubMed]
- Steinberg WM, Rosenstock J, Wadden TA, et al. Impact of Liraglutide on Amylase, Lipase, and Acute Pancreatitis in Participants With Overweight/Obesity and Normoglycemia, Prediabetes, or Type 2 Diabetes: Secondary Analyses of Pooled Data From the SCALE Clinical Development Program. Diabetes Care 2017;40:839-48. [Crossref] [PubMed]
- Steinberg WM, Buse JB, Ghorbani MLM, et al. Amylase, Lipase, and Acute Pancreatitis in People With Type 2 Diabetes Treated With Liraglutide: Results From the LEADER Randomized Trial. Diabetes Care 2017;40:966-72. [Crossref] [PubMed]
- Pyke C, Heller RS, Kirk RK, et al. GLP-1 receptor localization in monkey and human tissue: novel distribution revealed with extensively validated monoclonal antibody. Endocrinology 2014;155:1280-90. [Crossref] [PubMed]
- Hou Y, Ernst SA, Heidenreich K, et al. Glucagon-like peptide-1 receptor is present in pancreatic acinar cells and regulates amylase secretion through cAMP. Am J Physiol Gastrointest Liver Physiol 2016;310:G26-33. [Crossref] [PubMed]
- Wewer Albrechtsen NJ, Albrechtsen R, Bremholm L, et al. Glucagon-like Peptide 1 Receptor Signaling in Acinar Cells Causes Growth-Dependent Release of Pancreatic Enzymes. Cell Rep 2016;17:2845-56. [Crossref] [PubMed]
- Koehler JA, Baggio LL, Cao X, et al. Glucagon-Like Peptide-1 Receptor Agonists Increase Pancreatic Mass by Induction of Protein Synthesis. Diabetes 2015;64:1046-56. [Crossref] [PubMed]
- Gotfredsen CF, Molck AM, Thorup I, et al. The Human GLP-1 Analogs Liraglutide and Semaglutide: Absence of Histopathological Effects on the Pancreas in Nonhuman Primates. Diabetes 2014;63:2486-97. [Crossref] [PubMed]
- Bonner-Weir S, In't Veld PA, Weir GC. Reanalysis of study of pancreatic effects of incretin therapy: methodological deficiencies. Diabetes Obes Metab 2014;16:661-6. [Crossref] [PubMed]
- Ueberberg S, Jutte H, Uhl W, et al. Histological changes in endocrine and exocrine pancreatic tissue from patients exposed to incretin-based therapies. Diabetes Obes Metab 2016;18:1253-62. [Crossref] [PubMed]
- Smits MM, Tonneijck L, Muskiet MH, et al. Pancreatic Effects of Liraglutide or Sitagliptin in Overweight Patients With Type 2 Diabetes: A 12-Week Randomized, Placebo-Controlled Trial. Diabetes Care 2017;40:301-8. [Crossref] [PubMed]
- Tanaka K, Saisho Y, Manesso E, et al. Effects of Liraglutide Monotherapy on Beta Cell Function and Pancreatic Enzymes Compared with Metformin in Japanese Overweight/Obese Patients with Type 2 Diabetes Mellitus: A Subpopulation Analysis of the KIND-LM Randomized Trial. Clinical Drug Investigation 2015;35:675-84. [Crossref] [PubMed]
- Faillie JL, Yu OH, Yin H, et al. Association of Bile Duct and Gallbladder Diseases With the Use of Incretin-Based Drugs in Patients With Type 2 Diabetes Mellitus. JAMA Intern Med 2016;176:1474-81. [Crossref] [PubMed]
- Pi-Sunyer X, Astrup A, Fujioka K, et al. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N Engl J Med 2015;373:11-22. [Crossref] [PubMed]
- Meier JJ, Rosenstock J. Therapy: Gastrointestinal safety of incretin therapies: are we there yet? Nat Rev Gastroenterol Hepatol 2016;13:630-2. [Crossref] [PubMed]
- Lando HM, Alattar M, Dua AP. Elevated amylase and lipase levels in patients using glucagonlike peptide-1 receptor agonists or dipeptidyl-peptidase-4 inhibitors in the outpatient setting. Endocr Pract 2012;18:472-7. [Crossref] [PubMed]
- Tokuyama H, Kawamura H, Fujimoto M, et al. A low-grade increase of serum pancreatic exocrine enzyme levels by dipeptidyl peptidase-4 inhibitor in patients with type 2 diabetes. Diabetes Res Clin Pract 2013;100:e66-9. [Crossref] [PubMed]
- Sato S, Saisho Y, Kou K, et al. Efficacy and Safety of Sitagliptin Added to Insulin in Japanese Patients with Type 2 Diabetes: The EDIT Randomized Trial. PLoS One 2015;10:e0121988. [Crossref] [PubMed]
- Shetty AS, Nandith A, Snehalath C, et al. Treatment with DPP-4 inhibitors does not increase the chance of pancreatitis in patients with type 2 diabetes. J Assoc Physicians India 2013;61:543-4. [PubMed]
- Lehrke M, Marx N, Patel S, et al. Safety and Tolerability of Linagliptin in Patients With Type 2 Diabetes: A Comprehensive Pooled Analysis of 22 Placebo-controlled Studies. Clin Ther 2014;36:1130-46. [Crossref] [PubMed]
- Matveyenko AV, Dry S, Cox HI, et al. Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin. Diabetes 2009;58:1604-15. [Crossref] [PubMed]
- Gier B, Matveyenko AV, Kirakossian D, et al. Chronic GLP-1 Receptor Activation by Exendin-4 Induces Expansion of Pancreatic Duct Glands in Rats and Accelerates Formation of Dysplastic Lesions and Chronic Pancreatitis in the KrasG12D Mouse Model. Diabetes 2012;61:1250-62. [Crossref] [PubMed]
- Butler AE, Campbell-Thompson M, Gurlo T, et al. Marked Expansion of Exocrine and Endocrine Pancreas With Incretin Therapy in Humans With Increased Exocrine Pancreas Dysplasia and the Potential for Glucagon-Producing Neuroendocrine Tumors. Diabetes 2013;62:2595-604. [Crossref] [PubMed]
- Yazbeck R, Howarth GS, Abbott CA. Dipeptidyl peptidase inhibitors, an emerging drug class for inflammatory disease? Trends Pharmacol Sci 2009;30:600-7. [Crossref] [PubMed]
- Attaway A, Mersfelder TL, Vaishnav S, et al. Bullous pemphigoid associated with dipeptidyl peptidase IV inhibitors. A case report and review of literature. J Dermatol Case Rep 2014;8:24-8. [Crossref] [PubMed]
- Ujiie H, Muramatsu K, Mushiroda T, et al. HLA-DQB1*03:01 as a Biomarker for Genetic Susceptibility to Bullous Pemphigoid Induced by DPP-4 Inhibitors. J Invest Dermatol 2017. [Epub ahead of print]. [Crossref] [PubMed]


