Trends in total ankle arthroplasty and revisions in the Medicare database
Introduction
Total ankle arthroplasty (TAA) has been utilized by orthopedic surgeons since the 1970’s but was fraught with high failure rates and unacceptable patient outcomes (1). This has led to ankle arthrodesis becoming the favored treatment option (2). As new prosthetic designs and techniques emerged, improved outcomes and decreased failure rates have brought TAA back as a viable alternative to arthrodesis. However, the literature still suggests that the failure rate of TAA is about 10–20% within 10 years (3,4). Furthermore, TAA has been shown to have a significantly higher revision rate compared with total knee arthroplasty (TKA) and total hip arthroplasty (THA) (5,6). Current literature has not adequately investigated the recent trends in TAA utilization and revision rate. The purpose of this study was to determine the trends in TAA utilization and the rate of revision TAA by analyzing a comprehensive Medicare database for procedures performed between 2005 and 2012.
Methods
A retrospective review of a large comprehensive Medicare database within the PearlDiver Supercomputer application (Warsaw, IN) of the index procedures TAA and revision TAA will be conducted. The PearlDiver database is a publicly available, Health Insurance Portability and Accountability Act (HIPAA)-compliant national database compiled from a collection of Medicare records. This database contains current procedural terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) codes from 2005 to 2012.
Patients who underwent TAA and revision TAA were identified by Current Procedural Terminology (CPT)-27702, 27703, and International Classification of Disease ninth revision (ICD) codes 81.56, 81.59 respectively. The primary outcomes of this study were annual revision incidence, annual TAA utilization, and annual revision burden on the healthcare system. Revision burden was defined as a ratio of revisions to the sum of revision and primary procedures. Demographic data such as age, gender, and geographical location of patients was also examined. Statistical analysis of this study was performed with Minitab v17 (State college, PA) and was primarily descriptive including calculating the compound annual growth rate (CAGR) through the standard formula of utilization. Paired t-tests were utilized where appropriate.
Results
Our search returned a total of 7,181 TAAs and 1,431 revision TAAs within the study period of 2005–2012. Within our study period there was a 16.37% CAGR for TAA and a 7.74% CAGR for revision TAA. There was an overall revision incidence of 19.93% (−7.41% CAGR) and a revision burden of 16.62% (−6.17%). Annual utilization, revision incidence, and revision burden is detailed within Table 1.
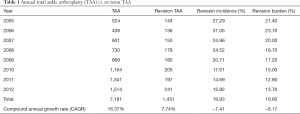
Full table
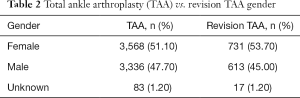
Amongst females there were 3,568 TAA (51.10%) and 731 revision TAA (53.70%) compared with 3,336 TAA (47.70%) and 613 revision TAA (45.00%) amongst males Table 2. The majority of TAA were found in the 65–69 age group (30.90%) followed by the 70–74 age group (25.40%). The majority of revision TAA were performed in the 65–69 age group (26.30%) followed by the <65 year age group (23.30%). A breakdown of TAA and revision TAA amongst all age groups is listed in Table 3.
Full table
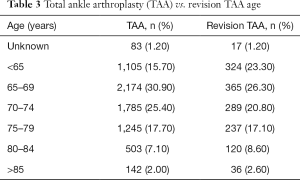
Full table
The highest number of TAA and revision TAA were performed in the South (35.50%, 36.30%) and the lowest in the Northeast (10.40%, 11.60%) geographic regions Table 4.
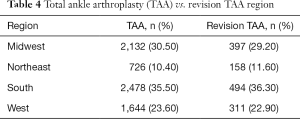
Full table
Discussion
The purpose of this study was to determine the trends in TAA utilization and the rate of revision TAA by analyzing a comprehensive Medicare database for procedures performed between 2005 and 2012.
The primary questions of our study were to determine:
- What are the trends in TAA utilization?
- What is the revision incidence and revision burden of TAA?
- What are the demographic considerations in TAA and revision TAA such as age and gender?
Currently the gold standard of surgical treatment for end stage arthritis that has failed conservative management is ankle arthrodesis (7). Advances in TAA technology has led to better prosthetics, improved techniques, and increased interest in TAA (8,9). This is supported by the results of our study, which describe an increase in the utilization of TAA from 524 in 2005 to 1,514 in 2012 (CAGR 16.37%). A recent study comparing the trends in TAA versus ankle arthrodesis further supported these findings by describing a steady increase in TAA utilization from 2006–2010. Nevertheless, ankle arthrodesis was still performed six times more frequently (2). Our data is further supported by a study on TAA utilization that investigated international registries, including Australia, England/Wales, Finland, New Zealand, Norway, and Sweden, that found an increase of TAA procedures performed from 191 in 2000 to 911 in 2011 (10).
Failed TAA can have serious consequences including below the knee amputation (11,12). Thus it is important to consider the revision incidence and burden of TAA. The results of the present study found a revision incidence of 19.93% and a revision burden of 16.6%. This is supported by a study on the Scandinavian Total Ankle Replacement (STAR) system implanted in 51 ankles that found a revision rate of 23.5% (13). This is further supported by a recent study which investigated joint registries in Norway, Sweden and New Zealand for the STAR (Waldemar Link, Hamburg, Germany); Agility (DePuy, Warsaw, IN 46582); Büchel-Pappas (Endotec, Orange, NJ); Hintegra (Newdeal SA, Vienne, France); Mobility (DePuy, Warsaw, IN 46582); Ramses (Laboratoire Fournitures Hospitalieres, Heimsbrunn, France) ankle implants and found an average revision rate of 21.8% after 5 years, and 43.5% after 10 years regardless of implant type (5).
A wide variety of studies have been conducted comparing TAA and arthrodesis. The American Orthopedic Foot and Ankle Society recently published a position statement in which they endorse the use of TAA in patients with arthritic conditions. The statement emphasizes the improvement in quality of life, pain reduction and function, which occur mainly with TAA but also acknowledge that ankle fusion provides similar pain reduction compared to TAA. Other potential benefits of TAA over ankle arthrodesis include the decreased stress on the subtalar and midfoot joints as well as improved gait.
The results of our study show that TAA (51.1% in females vs. 47.7% in males, P=0.0001) and revision TAAs are significantly higher in females (53.7% in females vs. 45.0% in males, P=0.0001). However in contrast to our study, Henricson et al. investigated 531 prostheses where 101 were revised (19%) and determined gender to not be a significant (P=0.4) factor in revision (14). Conversely, a recent study investigated the effect of gender on 116 revised TAA patients and found that the AOFAS hindfoot score for male patients did better (76±20) than female patients (67±17, P=0.03) (15). There are few other studies investigating gender disparities as a revision risk factor.
Limitations
This study is not without limitations. The PearlDiver database is reliant upon accurate CPT or ICD coding which creates the potential for a reporting bias. Also certain patients might have received either a below knee amputation with a previous removal of implant of just a removal of implant or arthrodesis which might cause certain skewedness of the data. The type of implant used and cause for revision were not investigated within this study. However, the focus of this study was to determine the overall trends, thus potential bias should be mitigated. Additionally, comorbidities such as BMI were not stratified as a factor that can affect revision rate. However, this study benefits from a large patient population and the inclusion of eight years of data in trend analysis.
Conclusions
Our analysis of the Medicare database shows that there is a high rate of annual growth in TAA utilization (16.37%) and revision TAA (7.74%) indicating that there is an increased demand for TAA in the Unites States. However, failed TAA can have serious consequence and revision TAA remains to have suboptimal results. This study highlights the recent trends in ankle arthroplasty and serves to increase awareness of this increasingly popular procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Because of the retrospective nature of this study, i.e., via a HIPAA compliant database, no IRB approval was needed, as there are no patient identifiers.
References
- Jonck JH, Myerson MS. Revision total ankle replacement. Foot Ankle Clin 2012;17:687-706. [Crossref] [PubMed]
- Raikin SM, Rasouli MR, Espandar R, et al. Trends in Treatment of Advanced Ankle Arthropathy by Total Ankle Replacement or Ankle Fusion. Foot Ankle Int 2014;35:216-24. [Crossref] [PubMed]
- Knecht SI, Estin M, Callaghan JJ, et al. The Agility total ankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg Am 2004;86-A:1161-71. [Crossref] [PubMed]
- Bonnin M, Gaudot F, Laurent JR, et al. The Salto total ankle arthroplasty: survivorship and analysis of failures at 7 to 11 years. Clin Orthop Relat Res 2011;469:225-36. [Crossref] [PubMed]
- Labek G, Klaus H, Schlichtherle R, et al. Revision rates after total ankle arthroplasty in sample-based clinical studies and national registries. Foot Ankle Int 2011;32:740-5. [Crossref] [PubMed]
- Sadoghi P, Liebensteiner M, Agreiter M, et al. Revision Surgery After Total Joint Arthroplasty: A Complication-Based Analysis Using Worldwide Arthroplasty Registers. J Arthroplasty 2013;28:1329-32. [Crossref] [PubMed]
- Ahmad J, Raikin SM. Ankle arthrodesis: the simple and the complex. Foot Ankle Clin 2008;13:381-400. viii. [Crossref] [PubMed]
- Gougoulias NE, Khanna A, Maffulli N. History and evolution in total ankle arthroplasty. Br Med Bull 2009;89:111-51. [Crossref] [PubMed]
- Cracchiolo A 3rd, Deorio JK. Design features of current total ankle replacements: implants and instrumentation. J Am Acad Orthop Surg 2008;16:530-40. [Crossref] [PubMed]
- Roukis TS, Prissel MA. Registry data trends of total ankle replacement use. J Foot Ankle Surg 2013;52:728-35. [Crossref] [PubMed]
- Jeng CL, Campbell JT, Tang EY, et al. Tibiotalocalcaneal Arthrodesis With Bulk Femoral Head Allograft for Salvage of Large Defects in the Ankle. Foot Ankle Int 2013;34:1256-66. [Crossref] [PubMed]
- Easley ME, Adams SB, Hembree WC, et al. Results of Total Ankle Arthroplasty. J Bone Joint Surg Am 2011;93:1455-68. [Crossref] [PubMed]
- Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg Am 2003;85-A:1321-9. [Crossref] [PubMed]
- Henricson A, Skoog A, Carlsson A. The Swedish Ankle Arthroplasty Register: An analysis of 531 arthroplasties between 1993 and 2005. Acta Orthop 2007;78:569-74. [Crossref] [PubMed]
- Hintermann B, Zwicky L, Knupp M, et al. HINTEGRA revision arthroplasty for failed total ankle prostheses. J Bone Joint Surg Am 2013;95:1166-74. [Crossref] [PubMed]


