Total knee arthroplasty fibrosis following arthroscopic intervention
Introduction
With more than 980,000 knee arthroscopic procedures performed each year in the United States alone, it is not surprising that many patients undergoing total knee arthroplasty (TKA) have also undergone a previous arthroscopic procedure (1,2). Currently, 12% of TKA recipients in the United States have experienced the procedure prior to joint arthroplasty (3,4). A large reason for so many arthroscopic procedures is that, in general, arthroscopy is considered to be a relatively benign procedure with limited trauma to periarticular soft tissues (5). Also, knee arthroscopy before TKA is often considered a minor surgical procedure and many surgeons do not consider it a risk factor for complications or poor outcomes after TKA (5,6). Despite this paradigm, multiple studies have shown potential complications resulting from knee arthroscopy (5-8). With the incidence of both knee arthroscopy and TKA increasing, it is important to determine the possible effects of prior arthroscopy on the success of TKA.
The overall complication rate, including infections pulmonary embolism, and arthrofibrosis, for knee arthroscopy is roughly 5% (6). Although these complications do not all impact the success of a future TKA, some, such as infection, can make future surgeries more complicated. Joint infection can lead to soft tissue damage, resulting in scar tissue formation, making future knee surgeries more technically challenging (9,10). Even if no obvious, superficial complications occur from knee arthroscopy, changes in deeper tissue layers may still occur. Thickened tissue resulting from previous surgery increases the chances of wound healing problems and subsequent infections after TKA (9). Similarly, post-arthroscopic bleeding, as well as the osmolality differences between the normal saline used to irrigate and the native synovial fluid (282 vs. 420 mOs), might lead to capsular reactions and resultant capsular thickening (11). This thickened tissue brings with it an increased risk for functional impairment, pain, and considerable patient dissatisfaction after TKA (12). Despite a conflicting and small body of literature arguing whether or not prior arthroscopy impacts TKA success, there is a distinct lack of literature examining quantifiable changes to the knee tissue after arthroscopy (3,4,7,8,13,14). Identifying patients at risk for complications or poor outcomes after TKA is essential for surgical planning; therefore, it is important to determine if prior knee arthroscopy results in appreciable changes to the capsular tissue of the knee.
The purpose of this study was to compare a matched cohort of patients undergoing TKA to evaluate whether there was capsular reaction in those who had a prior arthroscopic surgery compared to those who did not. More specifically, the groups were compared histologically for: (I) synovial thickness; (II) cellularity; and (III) the amount of fibrous tissue.
Methods
Patient selection
A total of 80 prospective patients undergoing TKA were consented for this study with institutional review board approval. Prior to their TKA, 40 consecutive patients who had previously undergone arthroscopy were matched to 40 consecutive patients who had not undergone arthroscopy. Patient mean age was 62 years (range, 42 to 83 years) and there were 23 women and 17 men, who had a mean BMI of 34 kg/m2 (range, 23 to 45 kg/m2). Patients with potentially confounding medical comorbidities that could cause fibrosis, such as pseudogout, rheumatoid arthritis, and/or hemarthrosis, were excluded from this analysis.
Histologic evaluation
During their TKA procedure, all patients underwent an intraoperative biopsy of their knee capsule and fat pad. These samples were preserved in formalin and the sections were sent to pathology. The pathologist was blinded to the cohort from whom the sample came from. Samples were classified as equivocal, slight to moderate, and moderate to severe based on standard, established pathological criteria. Specifically, each knee capsule and fat pad biopsy was assessed for the degree of synovial thickness, the cell count, and the presence of fibrous tissue.
Data analysis
A student’s two-tailed t-test was used to compare the results from histological evaluations. A P<0.05 was used as the threshold for statistical significance. Statistical analysis was performed using SPSS version 24 (IBM corporation, Armonk, NY, USA).
Results
Synovial thickness
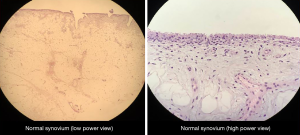
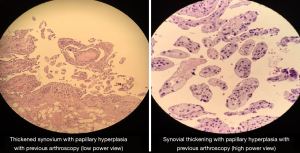
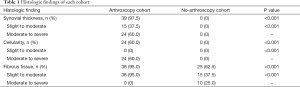
Thirty-nine (97.5%) out of the 40 patients who had a previous arthroscopic procedure also had an increase in synovial thickness. Of these 39 patients, 15 (38%) had a slight to moderate increase in thickness, while 24 patients (62%) had moderate to severe increase in synovial thickness. From the cohort of patients who did not undergo a previous arthroscopic procedure, zero patients had an increase in synovial thickening. Therefore, there was a significantly higher proportion of patients who had increased synovial thickness in the prior arthroscopy group as compared to the no-prior arthroscopy group (97.5% vs. 0%, P<0.001) (Table 1, Figures 1,2).
Full table
Cellularity
Twenty-four (60%) out of the forty patients who had a previous arthroscopic procedure also had an increase in cellularity. Of these 24 patients, 0 (0%) had a slight to moderate increase in cellularity, while all 24 patients (100%) had moderate to severe increase in cellularity. From the cohort of patients who did not undergo a previous arthroscopic procedure, zero patients had an increase in cellularity. Thus, there was a significantly higher proportion of patients who had increased cellularity in the prior arthroscopy group as compared to the no-prior arthroscopy group (60.0% vs. 0%, P<0.001) (Table 1).
Fibrous tissue
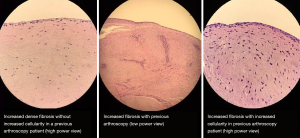
Thirty-eight (95%) out of the 40 patients who had a previous arthroscopic procedure also had an increase in fibrous tissue. Of these 38 patients, all 38 (100%) had a slight to moderate increase in fibrous tissue, while 0 patients (0%) had moderate to severe increase in fibrous tissue. From the cohort of patients who did not undergo a previous arthroscopic procedure, 25 (62.5%) patients had an increase of fibrous tissue. Fifteen (60%) of these 25 patients had a slight to moderate increase in fibrous tissue, while 10 patients (40%) had moderate to severe increase in fibrous tissue. Comparing the cohorts, there was a significantly higher proportion of patients who had increased fibrous tissue in the prior arthroscopy group as compared to the no-prior arthroscopy group (95% vs. 62.5%, P<0.001) (Table 1, Figure 3).
Discussion
Although thought by many to be a benign procedure, arthroscopic surgery may have long-term effects on capsular tissue, impacting the success of subsequent joint arthroplasty. Anecdotally, surgeons have observed that patients with prior arthroscopic surgery on their knee have a joint capsule that is thicker and denser. In the current study, histologic assessment confirms there may be increased synovial thickness, increased cellularity, as well as thickening of fibrous tissue in TKA patients who had previously undergone knee arthroscopy. Post-arthroscopic bleeding and the osmolality mismatch between synovial fluid and the saline irrigation used in arthroscopy can both lead to changes in the capsular tissue of the knee. Additionally, infection is the most common side effect of arthroscopy, which can also increase the cellularity and thickness of the tissues surrounding the knee joint (6,10). Any trauma affecting the synovial joint constitutes an irritative stimulus, thickening the capsular tissue surrounding the joint, and arthroscopy represents a trauma to the joint (15). This thickening of capsular tissue is not benign, and can lead to serious functional impairment, pain, and considerable patient dissatisfaction after TKA, making identification of patients at risk for such a complication important (12).
There are several limitations to our current study. Matching studies are inherently subject to observation bias; however, we attempted to limit this bias by blinding the pathologist to the patient groupings. Similarly, the histological features of the samples were classified subjectively, introducing the possibility of bias. Blinding the pathologist as well as utilizing the same pathologist for all sample classifications served to mitigate this possible bias. Another limitation is our low number of patients. With only 40 patients per group, our findings may not be generalizable. Despite these limitations, this matched study successfully demonstrated histological differences in the capsular tissue of patients with prior arthroscopy compared to patients without arthroscopy.
Although no studies examine the histological changes resulting from arthroscopy before TKA, multiple studies report poorer outcomes after TKA in patients with prior arthroscopy procedures (5,7,8,13). A study by Barton et al. examining 186 patients who underwent TKA less than 1 year after arthroscopy found similar results to the current study (13). Patients reported significantly poorer outcomes after TKA if the joint arthroplasty was performed less than 6 months after arthroscopy, and the re-operation rate in the prior arthroscopy group was significantly higher than the non-arthroscopy group (13). Similarly, Werner et al. found TKA within 6 months of arthroscopy is associated with an increased risk for postoperative stiffness and infection (8). Another study by Piedade et al. found that prior soft tissue knee surgery, including arthroscopy, resulted in poorer outcomes after primary TKA as compared to a cohort without prior surgery (7). An additional study by Piedade also found decreased implant survivorship and higher revision rates in patients undergoing TKA after arthroscopy (5). Overall, several studies report increased TKA complication rates after arthroscopy, many of which could arguably result from the histological changes reported in the current study.
Despite studies showing complication rate increases after TKA in patients with prior arthroscopy, some literature continues to report that there is no correlation between prior arthroscopy and decreased success of subsequent TKA (3,14). A study by Issa et al. looking at 62 knees with prior arthroscopy compared to 438 without previous arthroscopy found that prior knee arthroscopy had no impact on success of subsequent TKA (14). Issa et al. looked specifically at implant survivorship and radiographic analysis but failed to assess capsular thickening (14). Viste et al. similarly found that there was no difference in post-operative range of motion in TKA patients with previous arthroscopy as compared to those without previous arthroscopy; however, there was no assessment of capsular changes (3). They also found 5-year revision rates to be similar between the groups (3). Despite several studies showing no adverse outcomes in TKA patients with a history of arthroscopy, none of the studies examined histological changes following arthroscopy or the long-term survival of the TKA in these patients. Similarly, no studies examined long term losses in range of motion after TKA in patients with prior arthroscopy. Although our study demonstrated capsular thickening and fibrotic changes in knee tissue after arthroscopy, we cannot make assertions regarding possible timelines of complications without further research; therefore, these studies may not actually contradict our findings.
Conclusions
While prior knee arthroscopy has long been thought to have little impact on future knee surgeries, trauma from the procedure may, in fact, contribute to complications and poor outcomes after TKA. The results from this study indicate that in patients with a history of knee arthroscopy, increased synovial thickness, cellularity, and fibrous tissue is found. Future studies should determine the extent of the changes caused by arthroscopy, the timeline of histological changes, options to decrease the trauma cause by arthroscopy, and the best practices to optimize prior arthroscopy patients before TKA. Furthermore, future studies should also compare clinical and radiographic outcomes. The current study suggests that arthroscopic surgery may have long-lasting effects on periarticular tissue, especially the capsular tissue, which may have implications for pain and functional recovery after TKA.
Acknowledgements
None.
Footnote
Conflicts of Interest: PM Bonutti: Joint Active Systems Inc., Stryker, Zimmer. MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker: IP royalties, Surgical Techniques International, TissueGene. M Chughtai: DJ Orthopaedics, Sage Products, Stryker. The other authors have no conflicts of interest to declare.
Ethical Statement: Informed consent was received from each patient, prior to their enrollment in the study. The institution provides IRB approval, but does not assign IRB numbers.
References
- Bozic KJ, Kamath AF, Ong K, et al. Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA. Clin Orthop Relat Res 2015;473:2131-8. [Crossref] [PubMed]
- Kim S, Bosque J, Meehan JP, et al. Increase in Outpatient Knee Arthroscopy in the United States: A Comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am 2011;93:994-1000. [Crossref] [PubMed]
- Viste A, Abdel MP, Ollivier M, et al. Prior Knee Arthroscopy Does Not Influence Long-Term Total Knee Arthroplasty Outcomes and Survivorship. J Arthroplasty 2017;32:3626-31. [Crossref] [PubMed]
- Brophy RH, Gray BL, Nunley RM, et al. Total knee arthroplasty after previous knee surgery: expected interval and the effect on patient age. J Bone Joint Surg Am 2014;96:801-5. [Crossref] [PubMed]
- Piedade SR, Pinaroli A, Servien E, et al. Is previous knee arthroscopy related to worse results in primary total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 2009;17:328-33. [Crossref] [PubMed]
- Salzler MJ, Lin A, Miller CD, et al. Complications After Arthroscopic Knee Surgery. Am J Sports Med 2014;42:292-6. [Crossref] [PubMed]
- Piedade SR, Pinaroli A, Servien E, et al. TKA outcomes after prior bone and soft tissue knee surgery. Knee Surg Sports Traumatol Arthrosc 2013;21:2737-43. [Crossref] [PubMed]
- Werner BC, Burrus MT, Novicoff WM, et al. Total Knee Arthroplasty Within Six Months After Knee Arthroscopy Is Associated With Increased Postoperative Complications. J Arthroplasty 2015;30:1313-6. [Crossref] [PubMed]
- Abdel MP, von Roth P, Cross WW, et al. Total Knee Arthroplasty in Patients With a Prior Tibial Plateau Fracture: A Long-Term Report at 15 Years. J Arthroplasty 2015;30:2170-2. [Crossref] [PubMed]
- Naylor AR, Briggs MS, Kegelmeyer DK, et al. Rehabilitation and functional outcomes after extensive surgical debridement of a knee infected by fusobacterium necrophorum: a case report. Int J Sports Phys Ther 2013;8:311-27. [PubMed]
- Bar-Or D, Rael LT, Brody EN. Use of Saline as a Placebo in Intra-articular Injections in Osteoarthritis: Potential Contributions to Nociceptive Pain Relief. Open Rheumatol J 2017;11:16-22. [Crossref] [PubMed]
- Boldt JG, Munzinger UK, Zanetti M, et al. Arthrofibrosis Associated with Total Knee Arthroplasty: Gray-Scale and Power Doppler Sonographic Findings. AJR Am J Roentgenol 2004;182:337-40. [Crossref] [PubMed]
- Barton SB, McLauchlan GJ, Canty SJ. The incidence and impact of arthroscopy in the year prior to total knee arthroplasty. Knee 2017;24:396-401. [Crossref] [PubMed]
- Issa K, Naziri Q, Johnson AJ, et al. TKA results are not compromised by previous arthroscopic procedures. J Knee Surg 2012;25:161-4. [Crossref] [PubMed]
- Manunta AF, Zedde P, Pisanu F, et al. Sports-related changes of the synovial membrane. Joints 2015;2:181-7. [PubMed]