The management of a blood donor bitten by a snake
Introduction
The worldwide burden of snakebite is high. In fact, venomous snakes are found in many regions of the world and are a threat to public health, especially in the rural tropics where they are most abundant. Out of more than 3,000 species of snakes in the world, about 600 are venomous and over 200 are considered to be clinically significant (1). Annually, snakebites cause about 125,000 deaths and the permanent disabling or disfiguring of 400,000 people, mainly in developing countries (2-4). The individuals affected are mostly women, children and agricultural workers in poor rural communities (2). In the World Health Organization (WHO) database and image library, species of venomous snakes are listed in two categories according to the degree of public health risk that they present (1):
- Category 1 (highest medical importance): highly venomous snakes that are common or widespread and cause numerous snakebites, resulting in high levels of morbidity, disability or mortality;
- Category 2 (secondary medical importance): highly venomous snakes capable of causing morbidity, disability or death, for which exact epidemiological or clinical data may be lacking; and/or are less frequently implicated (due to their activity cycles, behaviour, habitat preferences or occurrence in areas remote to large human populations).
In Italy, viper bites are an infrequent event, though envenomation can cause severe complications, especially in children, related to their dose/body size ratio. Four species of poisonous snakes are present in Italy (1): the common viper (Vipera aspis), common throughout the country; the Vipera berus, found mainly in the Alps; the Vipera ammodydes found in the mountainous and hilly regions of North-East Italy; the Vipera ursini, found in the mountains of Central Italy, whose bite is never fatal (Table 1).
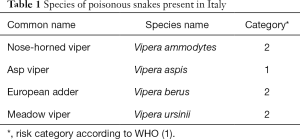
Full table
Blood Transfusion Services (BTS) have the responsibility to collect blood only from donors who are at low risk for any infection that could be transmitted through transfusion and who are unlikely to jeopardize their own health by blood donation. A rigorous process to assess the suitability of prospective donors is therefore essential to protect the safety and sufficiency of the blood supply, and safeguard the health of recipients of transfusion and blood donors themselves, while ensuring that suitable donors are not deferred unnecessarily. Persons disqualified from donating blood are known as “deferred” donors. A prospective donor may be deferred at any point during the “blood donor selection process”. A person can be deferred temporarily for a condition that is usually reversible, or permanently if he/she suffers from a certain medical condition (5).
Although people who have been bitten by a snake rarely wish to donate blood within a “short” time, it is however important to evaluate their eligibility to donate blood or blood components as their donation could be a problem for donor management, especially if a specific policy is not in place.
The aim of this manuscript is to summarise the worldwide existing donor deferral policy for snakebites and to provide some indications in order to facilitate decision-making and to guarantee maximum safety for the donors as well as for the recipients.
Snakebite effects on the human body
Snakebites often result in two puncture wounds from the reptile’s fangs. While most snakebites are innocuous as they are caused by non-poisonous species, sometimes poisoning does occur when venomous species are involved (6).
A dry bite is a “venomous snake bite without envenoming”, in which no venom is released. At least 25% of snakebite cases can be dry bites. Dry bites can occur from all venomous snakes, but their frequency varies from species to species (6).
The function of venomous snakebites is to immobilise the prey and to facilitate its digestion (7). The toxic component of snake venom can be classified into four broad categories: enzymes, polypeptides, glycoproteins, and low molecular weight compounds. They can also be classified as protein (90–95%) and non-protein (5–10%) compounds (7). Snake venom can be classified into haemotoxic, neurotoxic, necrotoxic, cardiotoxic, and nephrotoxic since snake venom has different predominant effects depending on the family (e.g., the venom of Crotalidae and Viperidae snakes is more haemotoxic and necrotoxic, whereas venom of the Elapidae subfamily is mainly neurotoxic) (8).
Snakebites have a wide range of effects, which go from simple puncture wounds to life-threatening illness and death (9-12). As far as venomous snakes concerned, the degree of intoxication and symptoms vary greatly: (I) no intoxication (“dry” bite); (II) mild intoxication (local oedema and pain); (III) moderate intoxication (pain, oedema spreading out from the bite zone, and systemic signs); and (IV) severe intoxication (shock, severe coagulopathy, and massive oedema) (10). The severity and outcome of a snakebite depend on the following factors: (I) bite localization; (II) snake’s size, condition of glands and teeth, bite angle, and bite duration; (III) microflora of the snake’s mouth and patient’s skin; (IV) patient’s age, weight, and state of health; (V) patient’s activity after a bite that influences the spread of the venom. Snake venom causes local and systemic body reactions (10).
Local signs are puncture wounds inflicted by the snake’s fangs; there can be one, two, or in rare cases more than two (9-12). The wound oozes with sero-haemorrhagic fluid and non-coagulant blood. Local oedema typically develops in a few to a maximum of 30 minutes. The skin becomes red and painful; this depends on the species of the snake in question. The venom of Viperidae snakes is characterized by a dominating cytotoxic effect; therefore, the pain is severe and burning. Petechiae, ecchymoses, and in rare cases vesicles as well as local tissue necrosis appear rapidly.
Systemic signs and symptoms are generalized, mainly haematologic and neuromuscular (9-12). General symptoms are weakness, fatigue, anxiety, tachycardia, weak pulse, bradycardia, tachypnea, sweating, nausea and vomiting, diarrhoea and acute abdominal pain, hypothermia or chills and fever, regional lymphadenopathy, lymphangitis (developing in 1–2 days), metal taste in mouth, headache, thirst, pulmonary oedema, heart failure, hypotension, collapse, shock, cerebral anoxia (sleepiness, slurred speech, disorientation, delirium, loss of consciousness), and anaphylactic reaction to venom proteins (facial, tongue, and epiglottic angioedema, which causes respiratory tract obstruction). If hypotension rapidly develops, it is one of the main signs of intoxication. If present, renal damage manifests as proteinuria, haemoglobinuria, myoglobinuria, azotemia, and anuria. A convulsive syndrome may occur due to cerebral anoxia caused by hypotension and anaemia, and not due to direct venom neurotoxicity. An electrocardiogram (ECG) may show nonspecific changes of the ST segment and the T wave, and episodes of atrial fibrillation. Haematological changes appear as coagulopathy and haemorrhagic syndrome ranging from local bleeding to profuse blood loss: bleeding from gums and nose, haematemesis, melena, haematuria, petechiae, and ecchymoses in the snakebite area. Bleeding may occur from the kidneys, lungs, peritoneum, rectum, vagina, endometrium, and pathological sites such as peptic ulcers. There might be a slightly noticeable icterus. Laboratory tests show prolonged prothrombin and activated partial thromboplastin time (APTT), decreased fibrinogen, plasminogen, factor XIII, factor V, antithrombin III, protein C levels, thrombocytopenia, elevated D-dimer level, morphological erythrocyte changes and anaemia, as well as neutrophilic leucocytosis. Neuromuscular damage manifests as paresthesias in the perioral region and fingers, muscular fasciculations, spasms, weakness, diplopia, hypersalivation, ptosis, myosis, dysphonia, dysphagia, trismus, respiratory dysfunction, and paralysis. The main reasons for death are shock, intracranial haemorrhage in the hypophysis, alimentary tract haemorrhage, and renal tubular necrosis.
As soon as the patient reaches hospital it is important to assess circulation, airway and breathing (CAB) before starting any kind of treatment, this includes appropriate management of any active bleeding and of the airway to avoid respiratory failure or aspiration (12,13). Monitoring of vital signs can be useful to forecast complications (13). After these measures have been taken care of, hydration through the use of a saline solution or Ringer’s lactate solution is necessary, as snake venom is capable of moving intravascular fluid to the “interstitial space”. Laboratory tests that are useful in these settings are complete blood count (CBC), prothrombin time (PT)/partial thromboplastin time (PTT), serum electrolytes, creatinine phosphokinase (CPK), urinalysis, blood urea nitrogen (BUN) and creatinine and a cross-match for blood. The wound should be inspected. The most important decision in managing a case of snakebite is to decide whether to administer an antivenomous serum or not (12). An antivenom is the mainstay of treatment of snakebite envenoming. However, adverse reactions to the antivenoms that are available are common in many parts of the world where snakebites are frequent (14).
A tetanus prophylaxis should be administered as the spores of the bacteria Clostridium tetani might enter the body when the snake bites. An antibiotic prophylaxis should not be administered, unless it is known that an incision of the bite has been performed or the poison has been sucked out of the wound. In these cases, a broad-spectrum antibiotic can be given. If the wound becomes infected, antibiotics are given according to the flora cultured from the wound’s secretions; in 90% of cases, Enterobacter spp., Pseudomonas spp., and Clostridium perfringens (9-13) are found.
For symptomatic treatment, antiemetic and antihistaminic drugs are given; following haemorrhage, fresh plasma, cryoprecipitate, and platelet mass are used; hypotension is corrected by crystalloids and vasopressors; pain is relieved by nonsteroidal anti-inflammatory drugs; and muscle spasms or seizures are treated with calcium gluconate.
The policies
Blood donor selection criteria is in place to ensure that only blood donors who meet the criteria are eligible to donate blood. An individual who does not meet the blood donor selection criteria will be deferred from blood donation (5,15-17). Blood donation deferral is a precautionary measure taken to protect the blood donor during the blood donation process as well as the patient who receives the transfusion. The period of deferral depends on the specific reason for disqualification (5,15-19). There are two types of deferral: (I) temporary deferral or (II) permanent deferral (5). An individual clinical and anamnestic evaluation is performed in the pre-donation phase.
For a donor who wishes to donate blood or blood components after being bitten by a snake, some recommendations stating the recommended deferral period for deferred donors have been provided by international or national health authorities (Table 2).
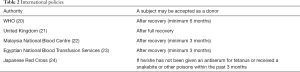
Full table
In 2009, in its publication “Safe blood and blood products. Module 1: safe blood donation”, the WHO stated that a person may be accepted as donors after recovering from a snakebite (minimum 6 months) (20).
The Joint Professional Advisory committee (JPAC) of the United Kingdom Blood Transfusion Services (UKBTS) in the “Whole blood and component donor selection guidelines (WB&C-DSG)” stated that donors must not donate until fully recovered and that in the donor evaluation the deferral period for surgery, transfusions or wounds, mouth and skin ulcers must be taken into account (21).
The Malaysia National Blood Centre, Ministry of Health in “Transfusion practice guidelines for clinical and laboratory personnel” recommended a deferral of 3 months after recovery from snakebite (22).
Moreover, also the Egyptian National Blood Transfusion Services indicated a deferral period of 3 months (23).
According to the Japanese Red Cross, anyone who has been given an antiserum for tetanus, snakebite or other poisons, etc. within the past 3 months may not donate blood (24).
Discussion
As reported in Indian studies, snakebites are the cause of 0.2% (25) to 0.481% (26) of temporary deferrals (3 months).In Italy, an estimation of the total number of snakebites per year ranges from 565 to 2,247 (3,27,28). Most subjects (about 60%) do not show any symptomatology related to envenomation (27).
From our research, it emerged that at national level there is a lack of regulations/guidelines regarding the management of candidate donors following a snakebite.
Considering the available information, at least a 3-month deferral after the snakebite event is suggested and anyway not until full recovery. Furthermore, the decision should take into account several factors: the type of snake involved (venomous or not), the characteristics of the injury, the characteristics of the venom (if released by the snake), the symptoms (local or systemic), and the treatment/s performed (surgery, transfusion therapy, supportive therapy, antibiotic therapy, etc.).
For example, in Italy, a Ministerial Decree of November 2nd, 2015 states that (29):
- Donors with a history of anaphylaxis are deferred permanently;
- Donors with acquired coagulopathy are deferred permanently;
- Donors who have been vaccinated for rabies (after exposure) are deferred for 1 year;
- Recipients of blood and blood products are deferred for 4 months following transfusion;
- Donors after undergoing major surgery are deferred for 4 months;
- Donors with a history of severe allergic reaction (excluding history of anaphylaxis) due to exposure to substances or drugs (especially penicillin, cephalosporin or insect venom from the Hymenoptera order) are deferred for 2 months from the last exposure;
- Donors with a history of recent assumption of drugs (including antibiotics) are subject to temporary deferral for a variable period of time depending on the active principle of prescribed drugs, the pharmacokinetics and the treated disease. For people taking medicines with a proven teratogenic effect, the suspension should be extended for an appropriate period in relation to the pharmacokinetic properties of the drug in question.
In addition, attention must be given to the laboratory tests in order to exclude the presence of coagulopathies and/or abnormalities, especially of a haematological nature. When the deferral period has expired, in order to assess donor eligibility, an evaluation of haemoglobin levels, white blood cells (WBCs), platelet count, electrolytes panel (sodium, potassium, chloride, bicarbonate) urea, creatinine, calcium, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total proteins, albumin, CPK, PT, PTT, antithrombin (AT) levels, and fibrinogen should be performed.
Conclusions
In Table 3, the most useful questions in the event of snakebite are reported.
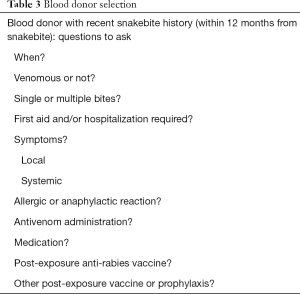
Full table
Although people who have been bitten by a snake rarely wish to donate blood within a “short” time, it is however important to evaluate their eligibility to donate blood or blood components as their donation could be a problem for donor management. Considering that the assessment of donor suitability for blood donation must stem from an individual risk assessment, some indications should be provided:
- The donor without intoxication (“dry” bite) or with mild intoxication (local oedema and pain), without any systemic, allergic or haemorrhagic symptom, without assumption of drugs or vaccination related to the snakebite episode should be deferred at least for 3 months;
- The donor with moderate intoxication (pain, oedema spreading out of the bite zone, and systemic signs) or severe intoxication (shock, severe coagulopathy, and massive oedemas) without a history of anaphylaxis or acquired coagulopathy should be deferred for at least 6 months, or until fully recovered;
- The donor with a history of anaphylaxis or acquired coagulopathy should be deferred permanently.
If the Italian legislation is taken into account, the deferral period indicated in point (I) and point (II) could be longer (29). Moreover, in order to assess donor eligibility, when the deferral period has expired, the following tests should be performed: WBC count, electrolytes panel, urea, creatinine, calcium, ALT, AST, total proteins, albumin, CPK, PT, PTT, fibrinogen, and AT.
Unfortunately, no detailed indications on blood donors’ deferral after a venomous snakebite have been provided by the European/International Health Authorities or by Transfusion Medicine Societies. In our opinion, well-defined and shared guidelines resulting from an expert working group would be appropriate to promote best and standardised practices in blood transfusion services. This would also guarantee maximum safety for both blood donors and recipients, as well as a safe, sufficient and timely supply of blood and blood products.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- WHO. Venomous snake distribution and species risk categories, 2010. Available online: http://apps.who.int/bloodproducts/snakeantivenoms/database/
- WHO. Launch of WHO Assessment and Listing of Snake Antivenoms. Available online: http://www.who.int/medicines/news/snake_antivenoms_assessment_listing/en/
- Chippaux JP. Snake-bites: appraisal of the global situation. Bull World Health Organ 1998;76:515-24. [PubMed]
- Williams D, Gutiérrez JM, Harrison R, et al. The Global Snake Bite Initiative: an antidote for snake bite. Lancet 2010;375:89-91. [Crossref] [PubMed]
- WHO. Blood Donor Selection. Guidelines on Assessing Donor Suitability for Blood Donation. Geneva: World Health Organization, 2012.
- Gold BS, Dart RC, Barish RA. Bites of venomous snakes. N Engl J Med 2002;347:347-56. [Crossref] [PubMed]
- Bottrall JL, Madaras F, Biven CD, et al. Proteolytic activity of Elapid and Viperid Snake venoms and its implication to digestion. J Venom Res 2010;1:18-28. [PubMed]
- Theakston RD, Laing GD. Diagnosis of snakebite and the importance of immunological tests in venom research. Toxins (Basel) 2014;6:1667-95. [Crossref] [PubMed]
- Junghanss T, Bodio M. Medically important venomous animals: biology, prevention, first aid, and clinical management. Clin Infect Dis 2006;43:1309-17. [Crossref] [PubMed]
- Adukauskienė D, Varanauskienė E, Adukauskaitė A. Venomous snakebites. Medicina (Kaunas) 2011;47:461-7. [PubMed]
- Mehta SR, Sashindran VK. Clinical features and management of snake bite. Med J Armed Forces India 2002;58:247-9. [Crossref] [PubMed]
- Isbister GK, Brown SG, Page CB, et al. Snakebite in Australia: a practical approach to diagnosis and treatment. Med J Aust 2013;199:763-8. [Crossref] [PubMed]
- Avau B, Borra V, Vandekerckhove P, et al. The Treatment of Snake Bites in a First Aid Setting: A Systematic Review. PLoS Negl Trop Dis 2016;10:e0005079. [Crossref] [PubMed]
- de Silva HA, Ryan NM, de Silva HJ. Adverse reactions to snake antivenom, and their prevention and treatment. Br J Clin Pharmacol 2016;81:446-52. [Crossref] [PubMed]
- De Kort W, Mayr W, Jungbauer C, et al. Blood donor selection in European Union directives: room for improvement. Blood Transfus 2016;14:101-8. [PubMed]
- Lieshout-Krikke RW, Domanovic D, De Kort W, et al. Selection strategies for newly registered blood donors in European countries. Blood Transfus 2017;15:495-501. [PubMed]
- De Paschale M, Latella S, Gatti A, et al. Presence of anti-HBs antibodies in blood donors 18-22 years after vaccination and implications for the selection of candidates for plasmapheresis for the production of hyperimmune plasma. Blood Transfus 2015;14:509-12. [PubMed]
- Angheben A, Boix L, Buonfrate D, et al. Chagas disease and transfusion medicine: a perspective from non-endemic countries. Blood Transfus 2015;13:540-50. [PubMed]
- Kaur G, Kaur P. Syphilis testing in blood donors: an update. Blood Transfus 2015;13:197-204. [PubMed]
- World Health Organization. Safe blood and blood products. Module 1: Safe blood donation. Geneva: World Health Organization, 2002. Available online: http://www.who.int/bloodsafety/transfusion_services/bts_learningmaterials/en/index.html
- United Kingdom Blood Transfusion Services (UKBTS). Whole Blood and Component Donor Selection Guidelines (WB&C-DSG). Release 21, 2014. Available online: https://www.transfusionguidelines.org/export/dsg/dsg-wb-pdf/203/21/01/dsg-wb_203_21_01.pdf
- Malaysia Ministry of Health. Malaysia National Blood Centre. Transfusion Practice Guidelines for Clinical and Laboratory Personnel. 3rd ed, 2008. Available online: http://hsajb.moh.gov.my/versibaru/uploads/bloodbank/garispanduan2.pdf
- Egyptian Ministry of Health. Egyptian National Blood Transfusion Standards. 2nd ed. Egypt: Egyptian Ministry of Health, 2011.
- Japanese Red Cross. Available online: http://www.jrc.or.jp/donation/about/refrain/
- Vimal M, Sowmya S, Nishanthi A, et al. Evaluation of blood donor deferral causes: a retrospective study from South India. Annals of Pathology and Laboratory Medicine 2016;3:606-11.
- Paparatnam K, Rajani K. An evaluation of blood donor deferral causes at tertiary care centre of Srikakulam district. J Evolution Med Dent Sci 2016;5:1349-51. [Crossref]
- Pozio E. Venomous snake bites in Italy: epidemiological and clinical aspects. Trop Med Parasitol 1988;39:62-6. [PubMed]
- Chippaux JP. Epidemiology of snakebites in Europe: a systematic review of the literature. Toxicon 2012;59:86-99. [Crossref] [PubMed]
- Disposizioni relative ai requisiti di qualità e sicurezza del sangue e degli emocomponenti. Ministerial Decree of 2nd November, 2015. Official Journal of the Italian Republic (series n. 300), 2015.


