Have the annual trends of total hip arthroplasty in rheumatoid arthritis patients decreased?
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune inflammatory disease that is characterized by systemic inflammation and synovial inflammation (1). The disease leads to functional disability, significant pain, and eventual permanent joint destruction as a result of the prolonged inflammation within the synovium that causes damage to the cartilage and bone. The treatment goals of RA are to slow the progression of the disease and minimize joint damage; however, joint destruction can still occur over time and may ultimately require surgical intervention. Researchers have found that approximately 3% to 25% of RA patients will require lower extremity total joint arthroplasty (2-4). As such, total hip arthroplasty (THA) has been documented as an acceptable and effective means of increasing the quality of life and functional measures in RA patients (5,6).
Disease progression and quality of life have significantly improved with the recent use of disease modifying anti-rheumatic drugs (DMARDs) for the medical management of RA (7-9). Moreover, in a recent systematic review, their efficacy has been shown to be beneficial in terms of clinical response and radiographic progression of disease in RA patients (10). In addition, the various DMARDs have been shown to have similar efficacy for the treatment of RA (11); therefore, prompt initiation of DMARD therapy is recommended by the American College of Rheumatology (12). With the increased use of DMARDs, it remains unclear whether or not there has been any effect on the annual rates of THA.
Therefore, considering the increased use of DMARDs, the purpose of this study was to examine the annual changes in the number of THAs in this population of patients. Specifically, we evaluated: (I) the annual trends of THAs due to RA in the United States population; (II) the annual trends in the proportion of THAs due to RA in the United States.
Methods
Data source
This study used the Nationwide Inpatient Sample (NIS) from 2002 to 2013. The NIS database is the largest publicly available all-payer inpatient admissions database in the United States and is part of the Healthcare Cost and Utilization Project (13). Approximately 7 to 8 millions inpatient records are collected annually, which is roughly a 20% random stratified sample of inpatient admissions. Within the database are patient demographics along with hospitalization variables, comorbidities, International Classification of Diseases, Ninth Revision (ICD-9) procedure and diagnosis codes, total in-hospital charges, hospital lengths of stay, and discharge dispositions. Since the NIS data is de-identified and publically available, this study was deemed exempt by the hospital’s Institutional Review Board.
Study population
This study identified all patients who had a primary THA, defined by the ICD-9 procedure code 81.51, performed between January 1, 2002 and December 31, 2013 (n=3,135,904). Then, to create a cohort of RA patients who underwent THA, an additional query was performed to identify all patients who had RA defined by the ICD-9 diagnosis code 714.0.
Data analysis
The incidences of THAs due to RA were obtained by dividing the number of THAs due to RA by the annual US population, obtained from the census bureau. The proportion of THAs due to RA was also evaluated for each year by dividing the number of THAs due to RA by the total number of THAs. Poisson regression analysis was used to analyze whether there was an annual increase in the incidence of the THAs due to RA in the United States population, due to the count nature of the dependent variable. The United States population was used as an offset term in the regression model. The changes in the incidence of THAs are represented using incidence rate ratios (IRRs), with IRR >1 denoting an increase in the procedural volume. Linear regression analyses were used to study the annual changes in the proportion of THAs due to RA. The annual change in the proportion of THAs due to RA is denoted by the regression coefficient (slope). A P value of less than 0.05 was used as the threshold for statistical significance. The 95% confidence intervals were calculated for the different measures used in the study. All of the data were analyzed with SPSS version 23 (IBM Corporation, Armonk, New York, USA).
Results
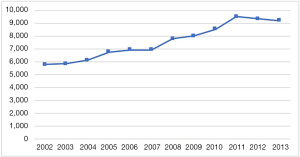
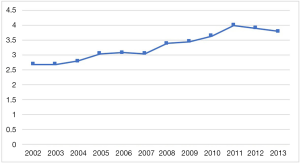
A total of 90,487 patients who had a diagnosis of RA and underwent THA over the specified time period were identified. The annual number of THAs with a diagnosis of RA increased by 59.3% from 5,764 to 9,180 (Figure 1). After normalizing to the US population, the incidence of THAs with RA increased from 2.7 to 3.8 THAs per million US adults [IRR =1.04 (95% CI: 1.04–1.04), P<0.001) (Figure 2).
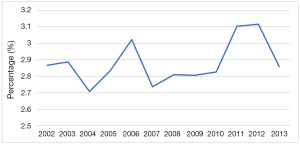
Out of the 201,167 THAs in 2002, 5,764 (2.87%) were due to RA, whereas, out of the 321,005 THAs in 2013, 9,180 (2.86%) were due to RA. The prevalence of RA in those who underwent THA remained the same from 2002 to 2013 [coefficient =0.01 (95% CI: −0.01 to 0.04), P=0.200] (Figure 3) .
Discussion
There has been a significant impact on the treatment of RA due to newer pharmaceutical innovations. Moreover, disease progression and joint destruction have decreased with the use of DMARDs (10). Chronic, as well as newly diagnosed, RA patients are now being managed with DMARDs as their primary treatment (14,15). Additionally, patients have reported considerable improvements in quality of life, as measured by health assessment surveys and disability questionnaire scores, with early and aggressive treatment (16). After analyzing the annual trends of RA patients who underwent THA, the present study found that there was no significant change in the prevalence of THA between 2002 and 2013.
There were several limitations to this study. There are inherent limitations with the use of large administrative databases for retrospective analysis. All databases have the potential for bias with data entry and errors in reporting diagnosis codes (17). Additionally, the accuracy of the diagnosis of RA within administrative databases has been debated (18), since it has been reported that there is a low positive predictive value when using diagnosis codes alone for the identification of patients who have RA (19). On the other hand, Bozic et al. (20) found that patient records were in line with coding comorbidity data from large administrative databases. The positive predictive value for a clinical diagnosis of RA, and the accuracy of the databases, may be strengthened since the patients diagnosed with RA by coding data from large databases required a surgical intervention (21,22). Furthermore, medications that patients were taking during their hospitalization were not reported in the NIS database, therefore information regarding RA patients’ DMARD use could not be determined; however, biological agent monotherapy as a treatment plan has been reported in approximately 34% of RA patients (1) and methotrexate monotherapy treatment has been recorded in as many as 50% of RA patients (23). Additionally, hydroxychloroquine was found to be the most commonly prescribed drug by a survey questionnaire sent to rheumatologists (24). Noteworthy is the increase in the United States population from approximately 288 million to 316 million during our study period, which could have potentially inflated the study results and overestimated the trends of THA if the increase in the population was skewed towards an older-aged demographic. Despite these limitations, we believe that the results of the present study provide an important insight into recent trends of THA in RA patients.
Previous studies have found a stable trend in the number of RA-associated surgical procedures performed annually, which is in accordance with the results of the present study. Momohara et al. (25) conducted a multicenter study in Japan and found that the total number of THAs and total knee arthroplasties (TKA) had remained stable between 1998 to 2008. Similarly, Yasui et al. (26) showed that the number of total joint arthroplasties, including knee, hip, elbow, shoulder, and ankle, had remained stable over the 3-year study period, despite an increase in the proportion of patients taking biological DMARDs. Manrique Arija et al. (27) also reported that there was no change in the number of THAs performed annually in RA patients at a single hospital in Spain from 1998 to 2007. An aging population may mask the true efficacy of DMARD therapy, despite the breakthroughs in the medical management of RA. Alternatively, new advances in THA have significantly improved patient quality of life and satisfaction (28), while shorter hospital stays, improved pain control, and earlier achievement of rehabilitation goals have been accomplished with breakthroughs in anesthetic regimens and postoperative pain management (29-31). Considering all of these factors, the threshold for RA patients to opt for surgical management may, therefore, be lower than it was in the past.
However, previous studies contradict the results of this investigation. Shourt et al. (32) showed that the rates of THA, TKA, joint reconstruction procedures, revision arthroplasty, and soft tissue procedures were trending downward over a 27-year period in Minnesota. Likewise, da Silva et al. (33) showed from 1955 to 1995, that the rates of THAs, TKAs, and revision of total joint arthroplasties among RA patients in Rochester, Minnesota have declined. This was similar to the results found by Hekmat et al. (16), who used a community-based register in Sweden and found a decrease in the annual incidence of THAs from 1997 to 2007. The effectiveness of DMARDs and their impact on the rate of THAs in RA patients must be inferred due to the ethical dilemmas centred around withholding treatments in order to conduct clinical research (34). The findings presented by these studies lend support to a more significant impact of the medical management of RA. Alternatively, a greater emphasis on the early detection and treatment of RA may have led to a decrease in the rate of THAs in RA patients and improved patient outcomes (35).
In conclusion, the present study was able to analyze the annual trends of RA patients who underwent THA by using the NIS database, demonstrating that the rates of THA performed in RA patients had remained relatively stable over the past decade. Our findings are most likely due to the overshadowing effect that the increase in the United States population by roughly 28.8 million people during the study period had on the efficacy of DMARDs. Longer observational studies are needed with a more stable populace in order to determine the true impact of DMARDs on THA in RA patients. Also, studies using mono- and dual therapy should be conducted, and the trends of THA in each treatment group compared, in order to determine the impact of the various DMARDs on disease progression.
Acknowledgements
None.
Footnote
Conflicts of Interest: MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc., Sage, Stryker: IP royalties, Surgical Techniques International, TissueGene. M Chughtai: DJ Orthopaedics, Sage Products, Stryker. The other authors have no conflicts of interest to declare.
Ethical Statement: This study was deemed exempt by the hospital’s Institutional Review Board.
References
- Detert J, Klaus P. Biologic monotherapy in the treatment of rheumatoid arthritis. Biologics 2015;9:35-43. [PubMed]
- Wolfe F, Zwillich SH. The long-term outcomes of rheumatoid arthritis: a 23-year prospective, longitudinal study of total joint replacement and its predictors in 1,600 patients with rheumatoid arthritis. Arthritis Rheum 1998;41:1072-82. [Crossref] [PubMed]
- Hotfiel T, Carl HD, Eibenberger T, et al. Cementless femoral components in bicondylar hybrid knee arthroplasty in patients with rheumatoid arthritis: A 10-year survivorship analysis. J Orthop Surg (Hong Kong) 2017;25:2309499017716252. [Crossref] [PubMed]
- Schrama JC, Espehaug B, Hallan G, et al. Risk of revision for infection in primary total hip and knee arthroplasty in patients with rheumatoid arthritis compared with osteoarthritis: a prospective, population-based study on 108,786 hip and knee joint arthroplasties from the Norwegian Arthroplast Register. Arthritis Care Res (Hoboken) 2010;62:473-9. [Crossref] [PubMed]
- Jones CA, Voaklander DC, Johnston DW, et al. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol 2000;27:1745-52. [PubMed]
- Wiklund I, Romanus B. A comparison of quality of life before and after arthroplasty in patients who had arthrosis of the hip joint. J Bone Joint Surg Am 1991;73:765-9. [Crossref] [PubMed]
- Picchianti-Diamanti A, Germano V, Ferlito C, et al. Health-related quality of life and disability in patients with rheumatoid, early rheumatoid and early psoriatic arthritis treated with etanercept. Qual Life Res 2010;19:821-6. [Crossref] [PubMed]
- Schiff MH, Yu EB, Weinblatt ME, et al. Long-term experience with etanercept in the treatment of rheumatoid arthritis in elderly and younger patients: patient-reported outcomes from multiple controlled and open-label extension studies. Drugs Aging 2006;23:167-78. [Crossref] [PubMed]
- Mathias SD, Colwell HH, Miller DP, et al. Health-related quality of life and functional status of patients with rheumatoid arthritis randomly assigned to receive etanercept or placebo. Clin Ther 2000;22:128-39. [Crossref] [PubMed]
- Nam JL, Ramiro S, Gaujoux-Viala C, et al. Efficacy of biological disease-modifying antirheumatic drugs: a systematic literature review informing the 2013 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis 2014;73:516-28. [Crossref] [PubMed]
- Donahue KE, Jonas DE, Hansen RA, et al. Drug therapy for rheumatoid arthritis in adults: an update [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US), 2012.
- Saag KG, Teng GG, Patkar NM, et al. American College of Rheumatology. American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum 2008;59:762-84. [Crossref] [PubMed]
- HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, Rockville, MD. 2013. Available online: www.hcup-us.ahrq.gov/nisoverview.jsp. 2015. n.d.
- Gaffo A, Saag KG, Curtis JR. Treatment of rheumatoid arthritis. Am J Health Syst Pharm 2006;63:2451-65. [Crossref] [PubMed]
- Sizova L. Approaches to the treatment of early rheumatoid arthritis with disease-modifying antirheumatic drugs. Br J Clin Pharmacol 2008;66:173-8. [Crossref] [PubMed]
- Hekmat K, Jacobsson L, Nilsson JÅ, et al. Decrease in the incidence of total hip arthroplasties in patients with rheumatoid arthritis--results from a well defined population in south Sweden. Arthritis Res Ther 2011;13:R67. [Crossref] [PubMed]
- George J, Newman JM, Ramanathan D, et al. Administrative databases can yield false conclusions-an example of obesity in total joint arthroplasty. J Arthroplasty 2017;32:S86-S90. [Crossref] [PubMed]
- Vinet E, Kuriya B, Widdifield J, et al. Rheumatoid arthritis disease severity indices in administrative databases: a systematic review. J Rheumatol 2011;38:2318-25. [Crossref] [PubMed]
- Ng B, Aslam F, Petersen NJ, et al. Identification of rheumatoid arthritis patients using an administrative database: a veterans affairs study. Arthritis Care Res (Hoboken) 2012;64:1490-6. [Crossref] [PubMed]
- Bozic KJ, Bashyal RK, Anthony SG, et al. Is administratively coded comorbidity and complication data in total joint arthroplasty valid? Clin Orthop Relat Res 2013;471:201-5. [Crossref] [PubMed]
- Stundner O, Danninger T, Chiu YL, et al. Rheumatoid arthritis vs osteoarthritis in patients receiving total knee arthroplasty: perioperative outcomes. J Arthroplasty 2014;29:308-13. [Crossref] [PubMed]
- Yoshihara H, Yoneoka D, Margalit A, et al. Rheumatoid arthritis patients undergoing total hip and knee arthroplasty have better in-hospital outcomes compared with non-rheumatoid arthritis patients. Clin Exp Rheumatol 34:270-5. [PubMed]
- Sulaiman W, Toib A, Chandrashekhar G, et al. The trends of DMARDS prescribed in rheumatoid arthritis patients in Malaysia. Oman Med J 2009;24:260-06. [PubMed]
- Pope JE, Hong P, Koehler BE. Prescribing trends in disease modifying antirheumatic drugs for rheumatoid arthritis: a survey of practicing Canadian rheumatologists. J Rheumatol 2002;29:255-60. [PubMed]
- Momohara S, Tanaka S, Nakamura H, et al. Recent trends in orthopedic surgery performed in Japan for rheumatoid arthritis. Mod Rheumatol 2011;21:337-42. [Crossref] [PubMed]
- Yasui T, Nishino J, Kadono Y, et al. Impact of biologics on the prevalence of orthopedic surgery in the National Database of Rheumatic Diseases in Japan. Mod Rheumatol 2010;20:233-7. [Crossref] [PubMed]
- Manrique Arija S, López Lasanta M, Jiménez Núñez FG, et al. Annual trends in knee and hip arthroplasty in rheumatoid arthritis 1998-2007. Reumatol Clin 2011;7:380-4. [Crossref] [PubMed]
- Zagra L. Advances in hip arthroplasty surgery: what is justified? EFORT Open Rev 2017;2:171-8. [Crossref] [PubMed]
- Peters CL, Shirley B, Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty 2006;21:132-8. [Crossref] [PubMed]
- Maheshwari AV, Blum YC, Shekhar L, et al. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res 2009;467:1418-23. [Crossref] [PubMed]
- Vadivelu N, Mitra S, Narayan D. Recent advances in postoperative pain management. Yale J Biol Med 2010;83:11-25. [PubMed]
- Shourt CA, Crowson CS, Gabriel SE, et al. Orthopedic surgery among patients with rheumatoid arthritis 1980-2007: a population-based study focused on surgery rates, sex, and mortality. J Rheumatol 2012;39:481-5. [Crossref] [PubMed]
- da Silva E, Doran MF, Crowson CS, et al. Declining use of orthopedic surgery in patients with rheumatoid arthritis? Results of a long-term, population-based assessment. Arthritis Rheum 2003;49:216-20. [Crossref] [PubMed]
- Mckeown EJ. The ethical challenges in rheumatology. Curr Rev Musculoskelet Med 2015;8:107-12. [Crossref] [PubMed]
- Almoallim H, Janoudi N, Attar SM, et al. Determining early referral criteria for patients with suspected inflammatory arthritis presenting to primary care physicians: a cross-sectional study. Open access Rheumatol 2017;9:81-90. [Crossref] [PubMed]


