Comparison of the efficacy of dispensing granules with traditional decoction: a systematic review and meta-analysis
Introduction
Traditional Chinese Medicine (TCM) has developed for thousands of years in China. The most common preparation of TCM is decoction, which is made by mixing particular herbs together and boiling them for half an hour or more after soaking. This traditional prescription and preparation exist for more than 2,000 years. Traditional decoction is considered to be absorbed efficiently with high bioavailability, but it is difficult to control the quality of each component herb, boiling time and amount of water, which results in inconsistent quality of traditional decoction and limits the application in clinical practice.
The innovative preparation of TCM, dispensing granules, which is also known as decocting-free granules, has been developed for about 20 years and prescribed by traditional medicine practitioners in several countries, such as China, Japan, Korea, or even United States. Dispensing granules are produced by Good Manufacturing Practice (GMP) qualified pharmaceutical companies (1,2). They are extracted from raw materials of individual Chinese herbal medicine, followed by the procedure of concentration, drying and granulation (3). Patients or traditional medicine practitioners can easily mix and dissolve different dispensing granules with hot water and get decoction.
However, controversies have accompanied with the application of dispensing granules since their appearance. Because dispensing granules are boiled with herbs separately while traditional decoctions are boiled with mixed herbs synchronously, which may bring about chemical changes. The differences in chemical component and bioactivity have been inconsistently reported between dispensing granules and traditional decoction in different studies (4-6), which may result in different clinical efficacy. Thus, we developed the present systematic review and meta-analysis to assess the efficacy of dispensing granules compared with traditional decoction.
Methods
Inclusion and exclusion criteria
The inclusion criteria of this review are: (I) randomized controlled trials (RCTs) for patients treated by dispensing granules comparison with traditional decoction; (II) the administration route was oral; (III) the participants ≥30 in both treatment group and control group; (IV) the outcomes should assess the efficacy of dispensing granules comparing with traditional decoction.
The exclusion criteria: (I) animal experiments; (II) the dispensing granules were not produced by medical corporations; (III) study protocols; (IV) systematic reviews/meta-analyses.
Search strategy
We searched the China National Knowledge Infrastructure (CNKI), Wanfang Databases, Cochrane Library, PubMed since their inception to 9, September, 2016. The Search strategy for PubMed was: ((((((random*[Title/Abstract]) OR (((“Clinical Trials as Topic”[Mesh]) NOT “Clinical Trials, Phase I as Topic”[Mesh]) OR “Observational Studies as Topic”[Mesh])) OR ((((“Clinical Trial” [Publication Type]) NOT “Clinical Trial, Phase I” [Publication Type])) OR “Observational Study” [Publication Type]))) AND (((((decoction[Title/Abstract]) OR decocta[Title/Abstract]) OR decoctum[Title/Abstract]) OR apozem[Title/Abstract]) OR elixation[Title/Abstract])) AND ((granule*[Title/Abstract]) OR herb*[Title/Abstract])). The Search strategy for Cochrane Library was:
#1 decoction:ti,ab,kw or decocta:ti,ab,kw or decoctum:ti,ab,kw or apozem:ti,ab,kw or elixation:ti,ab,kw (word variations have been searched);
#2 granule*:ti,ab,kw or herb*:ti,ab,kw (Word variations have been searched);
#3 random*:ti,ab,kw (Word variations have been searched);
#4 #1 and #2 and #3.
We used suitable terms for Chinese databases. There was no language restriction, but the published RCTs were eligible.
Study identification and data extraction
Two authors (Qiu RJ and Zhao C) reviewed the titles and abstracts for all of searched studies independently. If it is difficult to confirm whether the studies were eligible or not, we would retrieve full texts for further identification. If there were disagreements or controversies between the two authors, the third author (Shang HC) was invited to evaluate.
Two authors (Qiu RJ and Zhao C) extracted data and evaluated methodological quality of studies independently. We used the Cochrane Reviewer’s Handbook 5.0 to assess the risk of bias for all of the eligible articles. The data extraction included first author’s name, published time, diagnosis, the sample size, interventions and comparisons, duration of treatment time, outcomes, adverse effects. The data were validated by a third author (Shang HC). Any disagreements were resolved by discussion.
Data synthesis
We used RevMan 5.1.0 software which provided by the Cochrane Collaboration for data analyses. Meta-analysis was performed if the disease, prescription, treatment duration and outcomes were the same or similar. If the I square (I2) value exceeded 50% or P<0.1, it signified heterogeneity existing. We would pool data with fixed effects model if I2<50%; otherwise we would use random effects model (7). If there were sufficient number of studies, we would explore publication bias with funnel plot analysis.
Results
The literature search
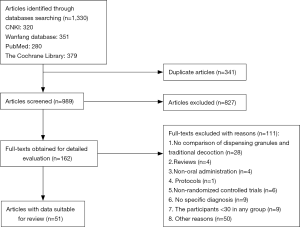
We searched 1,330 articles from 4 electronic databases according to the inclusive criteria. A total of 341 duplicate articles were excluded. After reading the titles and abstracts, 827 articles which did not meet the inclusive criteria were excluded. We retrieved 162 full-texts for further identification, 111 articles were removed with reasons. In the end, 51 eligible RCTs and 7,035 participants were included for this systematic review (Figure 1).
The characteristics of RCTs
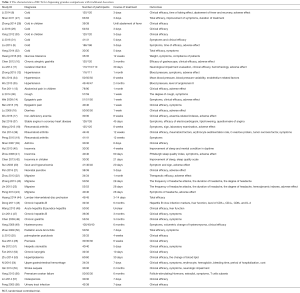
In the 51 RCTs, there were 33 different kinds of diseases for investigation, of which 8 RCTs observed common cold, 4 RCTs observed migraine. For rheumatoid arthritis, insomnia and hypertension, there were 3 RCTs reported respectively. The last RCTs reported different kinds of diseases in one or two trials. The majority of the interventions were treatment based on syndrome differentiation, but based on a fixed prescription. The outcomes were synthetic effects such as total/clinical efficacy for the majority of RCTs. Meanwhile, they preferred to assess symptoms rather than objective index or laboratory examination. Nineteen RCTs (37.3%) reported the adverse effect (8-26). The characteristics of these RCTs are in Table 1.
Full table
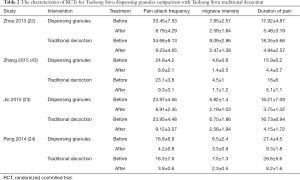
After assessing all of the trials, 4 RCTs which compared dispensing granules and traditional decoction with Taohong Siwu prescription in patients with migraine can be conducted meta-analysis in the efficacy of pain attack frequency, migraine intensity and duration of pain (22-24,43). The characteristics of the 4 RCTs are in Table 2.
Full table
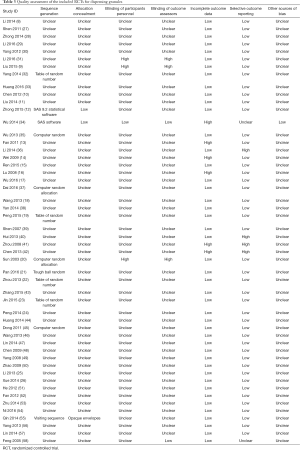
Methodological assessment
The majority of trials were in low methodological quality. Only 11 (21.6%) trials (12,19-23,32,34-35,37,45) were in low risk of bias in sequence generation, of which provided appropriate methods of randomization, such as computer random or table of random number. while 1 trial (55) was in high risk of bias because of the inappropriate methods of sequence generation. The last trials proclaimed that they were randomized trials, but there were no methods of randomization providing. Three trials (5.9%) mentioned appropriate methods of allocation concealment and had low risk of bias in it, the rest of them were unclear (12,34,55). One trial (34) provided the method of blinding for the participants, the outcome assessors and the statisticians did not know the allocation. One trial was in low risk of blinding of outcome assessors (58). The remaining trials did not mention if they took the methods of blind. Five trials (13,14,16,34,41) reported incomplete outcome data and in high risk of bias, while the last trials reported complete outcome data. We found 6 trials (11.8%) were in high risk of bias of selecting outcome data from their reporting (34,36,40-42,58). Because of limit reporting information, we did not know if the risk of other sources of bias existed except one (34). The assessment of risk of bias for the included trials of dispensing granules is in Table 3.
Full table
The efficacy of dispensing granules
For the 51 dispensing granules compared with traditional decoction, only 6 (11.8%) RCTs reported that the therapeutic efficacy of dispensing granules were significantly better than traditional decoction in patients with epigastric pain, stable angina, neonatal jaundice, herpetic stomatitis, chronic laryngitis, and hyperlipidaemia (15,21,37,51-53). Though another 4 (7.84%) trials described that there were no significant differences in total clinical efficacy between dispensing granule group and traditional decoction group, 1 trial (27) presented that participants with cold need much more time to bring down a fever in traditional decoction, 1 trial (33) showed that participants in dispensing granule group were much more satisfied with treatment, the other 2 trials reported that dispensing granules could improve the symptoms of headache and sweat significantly when compared with traditional decoction in patients with cold (9,31). One (1.96%) trial presented that traditional decoction had better benefit in treating insomnia in menopausal women (40). One RCT reported that traditional decoction could decrease the level of systolic blood pressure significantly compared with other groups, however, the other outcomes, such as the changes of blood pressure variability and endothelium function showed no significant differences between dispensing granules and traditional decoction (34). One trial compared dispensing granules with traditional decoction in treating upper gastrointestinal hemorrhage, the results showed that traditional decoction had better effect on improving symptoms, nevertheless, dispensing granules had better effect on improving hemorrhage, shortening hospitalization time and lowering cost (54).
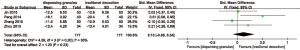
All of the last 38 (74.5%) RCTs showed that the efficacy of dispensing granules were similar with traditional decoction. Because of the disparate diseases and prescriptions distributed in different trials, we could not synthesize data for the majority of RCTs. But 4 trials (22-24,43) were pooled in meta-analysis, which compared the efficacy of dispensing granules and traditional decoction with Taohong Siwu prescription in patients with migraine. We conducted meta-analysis for the variation of the pain attack frequency, migraine intensity and pain duration before and after treatment. At last, for the efficacy of lowering pain attack frequency, the I2=42%, the heterogeneity can be accepted. We pooled data with fixed effects model. The weighted mean difference (WMD) =−1.03, 95% confidence interval (CI): −1.96 to −0.1, P<0.05, which reflected that dispensing granules had better effect on lowering pain attack (Figure 2). For the efficacy of improving migraine intensity, the I2=92%, though the result showed that there was no statistical significance with random effects model, we should draw a conclusion prudently. Migraine intensity is a subjective symptom, patients’ pain score report may be influenced by other factors and resulted in heterogeneity. All of the 4 RCTs did not use blinding methods, which result in inaccurate report and high heterogeneity (Figure 3). For the efficacy of lowering pain duration, the I2=35%, the heterogeneity can be accepted. We pooled data with fixed effects model. The dispensing granules versus traditional decoction was WMD =0.13, 95% CI: −0.08 to 0.34, P>0.05, which reflected that dispensing granules and traditional decoction had the similar effect on lowering pain duration (Figure 4). Though there were 4 RCTs can be conducted meta-analysis, we still could not draw a definite conclusion for the efficacy of decocting-free granules from these low quality and small sample trials.


From the results of systematic review, we should draw a prudent conclusion that the efficacy of dispensing granules was equivalent to traditional decoction. First, the majority of trials observed subjective outcomes, and the researchers assessed the results mainly based on patients’ self-report. The methods of blinding were unclear in most RCTs, which may result in overrating the therapeutic effect. Second, 15.7% (8/51) RCTs reported the disease of cold, a self-limited illness, which made it difficult to ascertain that whether the treatment effect due to herbs. Third, it may exist high risk of bias after we assessed the methodological quality, which made the reliability of trials decrease.
The adverse effect of dispensing granules
Eight RCTs (15.7%) reported the adverse effect in dispensing granules treatment group. One showed that the rate of adverse events were similar between two groups without specific description (12). The others presented that the common adverse effect in dispensing granules were nausea, vomiting, diarrhea, stomachache, or epigastric discomfort (17,22-24,26,57). Because the majority of included RCTs did not mention adverse events, so it is difficult to estimate the safety of dispensing granules compared with traditional decoction.
Publication bias
There were no sufficient number of appropriate studies to conduct funnel plot analysis, so the publication bias was unclear for this systematic review.
Discussion
Definitely, dispensing granules are convenient to patients, which can set them free from decocting. It is not merely saving time, but also easy to carry with, which may improve the patients’ compliance. However, whether dispensing granules take the same effect as well as traditional decoction, or whether they can substitute traditional decoction and be widespread used in clinical practice still keep uncertain. The most important thing is to provide enough high quality evidence of efficacy and safety for dispensing granules. At present, there are disputes existing.
First, the chemical consistency between traditional decoction and dispensing granules remain unclear. The herbs of dispensing granules are decocted respectively, while they are decocted together in traditional decoction, which may result in chemical inconsistency and influence clinical efficacy. The chromatograms of high performance liquid chromatography (HPLC) showed similarity in traditional decoction and dispensing granule decoction, but the content of baicalin was higher in dispensing granule decoction than in traditional decoction (59). A research showed that the content of glycyrrhizic acid was higher when decocted them as a whole than separately decocted (60). Other experiments revealed that components of Sanhuang Xiexintang changed during decocting when compared with dispensing granule (61). An animal experiment showed that there was no significant differences between Sanhuang Xiexintang traditional decoction and dispensing granule decoction in treating auricle swelling induced by xylene and tail-cut hemostasis in mice (62). But there are no clinical trials proving the similar efficacy of them.
Second, there were significant differences in chemical components when the dosage ratio was the same between traditional decoction and dispensing granule decoction (63). It is worthy to further investigate for the variation of chemical ingredients between dispensing granules and traditional decoction. Nevertheless, the components of herbs are complex, and it is hard to ascertain the bioactive substances of TCM. So the curative effect is much more important than components for TCM. From this systematic review, though 74.5% RCTs reported dispensing granules had similar clinical efficacy with traditional decoction, it should be cautious to draw firm conclusions that dispensing granules may substitute traditional decoction in clinical practice. The majority of trials were small sample with low methodological quality, which lowered the value of evidence. Meanwhile, researchers studied different diseases with different prescriptions, which made it difficult to merge data. Furthermore, some of diseases included in this review were self-limited disease and treatment duration was short, which made it difficult to ascertain whether the efficacy were due to herbs or not. The majority of outcomes were symptom-associated or patient-reported, which may exist bias in some extent.
Third, according to compatibility of TCM theory, compatibility of different herbs may take the effect of toxicity reducing and efficacy enhancing via boiling. Dispensing granules are extracted from single herb and lack the process of mixed boiling. Whether the toxicity of dispensing granules is increased or not keep unclear. On the other hand, some herbs should be decocted for a long time than others to generate effective ingredients or reduce toxicity, such as gypsum fibrosum, aconiti lateralis radix praeparata, aconiti radix cocta and talcum. Some herbs should be decocted later and boiled for shorter time than other herbs, such as menthae haplocalycis herba, uncariae ramulus cum uncis, to avoid the effect ingredients from being destroyed or volatilized (64). The extraction processes are non-transparent for the production of dispensing granules, so the safety keeps unknown when they are mixed together.
To provide high quality of evidence for clinical practice, well-designed, large-scale, multicenter RCTs are recommended (65,66). Definitively, RCTs are necessary to provide evidence for the average efficacy of dispensing granules comparing with traditional decoction. However, one of the characteristics of TCM is treatment based on syndrome differentiation, which equals to individualized treatment. It is inappropriate for all of patients treated with a fixed prescription. Treatments based on syndrome differentiation signify patients treated with different herbs according to different symptoms, which may result in different clinical efficacy. In our perspective, N-of-1 trials are better choice for researchers in exploring the efficacy of dispensing granules comparing with traditional decoction. N-of-1 trials are the most appropriate in chronic disease (67). Patients with chronic disease have relatively stable TCM syndromes. The prescription would not modify a lot, which provide a good condition to observe efficacy and safety of dispensing granules for researchers. The other characteristic of TCM is holism. The present evaluation method cannot reflect holistic view of TCM, especially for conflicting results in a trial. Fuzzy comprehensive evaluation may have potential benefit in evaluating the efficacy of TCM and worthy further investigation in the future.
Moreover, classical TCM prescriptions should be studied first. In China, there are more than 100 prescriptions in Treatise on Febrile Diseases, which have been used for about 2,000 years since the Eastern Han Dynasty and have been proved of good clinical efficacy. In this review, no more than 50 prescriptions were included, which was much less than frequently-used prescriptions in clinic. We propose the researchers should study a specific prescription for specific disease and compare the efficacy and safety of dispensing granules with traditional decoction.
If the efficacy and safety of dispensing granules are not inferior to traditional decoction, they are appropriate preparations to substitute traditional decoction in studying the relation of dose-effect/toxic-effect in TCM. The process is hard to control when patients boil decoction themselves. The amount of water, the time of boiling, and the container of herbs may influence the quality of decoction. However, when dispensing granules are produced in the same condition, the quality of herbs will be well controlled. Therefore, it will reduce confounding factors for research of dose-effect/toxic-effect in TCM with dispensing granules.
Conclusions
In conclusion, dispensing granules may take important role in the development of TCM. It needs much more evidence to prove the efficacy and safety of dispensing granule. N-of-1 trials and fuzzy comprehensive evaluation method are better choice for assessing the efficacy of them than RCTs. If dispensing granules are proved beneficial effect, they are appropriate preparations to study the relation of dose-effect/toxic-effect in TCM.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China [81430098].
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Zhou X, Wan J, Wu CJ, et al. Traditional Chinese Medicine formula granules and its internationalized production. China Pharmacy 2006;17:72-4.
- Tu YS, Bi XL. Traditional Chinese Medicine formula granules and its internationalized productio. World Science and Technology-Modernization of Traditional Chinese Medicine 2007;2:77-81.
- Zhang ZW, Sun XM, Zhang QX, et al. The research of Chinese herbal innovation. World Science and Technology 2002;2:34-8.
- Zhang HM, Song JZ, Tan HS, et al. From traditional decoction to modern granule: perspectives and prospects of Chinese Medicine dispensing granules. World Science and Technology-Modernization of Traditional Chinese Medicine 2012;14:1740-53.
- Zhong RK. The discussion of the advantage and shortage for Chinese dispensing granules. Journal of North Pharmacy 2011;8:73-4.
- Li CY. The advantage and shortage of Chinese decocting-free granules. Modern Medicine & Health 2011;27:898-9.
- Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, 2011. Available online: http://handbook-5-1.cochrane.org/
- Li YP, Xie WY. Comparison of Chinese dispensing granules and traditional decoction in clinical efficacy. Chongqing Medicine 2014;43:4092-3.
- Liu L, Dong C, Liu T. Chinese medicine granules and Chinese medicine decoction pieces for treating 186 cases of wind-heat common cold. Henan Traditional Chinese Medicine 2015;35:1621-3.
- Chen GY, Zhao BL, Liu QQ, et al. Observation on clinical efficacy of Chinese Dispensinggranules in treating chronic atrophic gastritis. Journal of New Chinese Mecicine 2012;44:53-4.
- Liu CZ, Li GJ, Li R, et al. Clinical research on treating cerebral infraction with Nao Quexue San. Clinical Journal of Chinese Medicine 2014;6:12-3,6.
- Zhong JB, Feng XG, Lu WX, et al. Clinical study of traditional Chinese medicine formula granules on multi-center' randomized controlled and non-inferiority of essential hypertension. Shanghai Journal of Traditional Chinese Medicine 2015;49:35-8.
- Fan MH. Clinical observation of 168 cases of infantile abdominal pain treated with the granules and decoction prepared with modified Xiangsha Liujunzi Tang and Wuyao San. World Journal of Integrated Traditional and Western Medicine 2011;6:408-9,49.
- Wei LF, Tian YZ, Xia JQ, et al. Comparison of the clinical effects between dispensing granules and traditional decoction of Liangfu Wan in treating patients withepigastric pain. Lishizhen Medicine and Materia Medica Research 2009;20:612-4.
- Ren XM. The comparison of clinical efficacy for Liangfuwan dispensing granules and traditional decoction in treating epigastric pain. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2015;3:35-6.
- Lu M, Tian YZ, Xia JQ, et al. Clinical study on drug grannies of Huoxiang-Zhengqisan for the treatment of cold wetness diarrhea. Guiding Journal of Traditional Chinese Medicine and Pharmacolog 2008;14:7-9,13.
- Wu W, Li QJ. Effect comparsion between Traditional Chinese Medicine granule preparation and traditional decoction of Guipi Decoction in treating women with iron deficiency anemia. Chinese Archives of Traditional Chinese Medicine 2016;34:750-3.
- Wang AW, Wang NN, Sun HS, et al. Comparison of the clinical effects between compatible granule and traditional decoction of Duhuo-Jisheng Tang in treating patients with rheumatoid arthritis. Chinese Journal of Hospital Pharmacy 2013;33:300-3.
- Peng M. Research on the effect of formula granule of Duhuo Jisheng decoction and traditional prepared drug in pieces on the biochemical index and clinical symptoms of patients with rheumatoid arthritis. Guangming Journal of Chinese Medicine 2015;30:2106-9.
- Sun WF, Xu W, Yao FQ, et al. Effect of Xiezhuo chubi decoction in decreasing serum uric acid in gout patients. Chinese Journal of Clinical Rehabilitation 2003;7:2962-3.
- Pan N. Comparison of Chinese berbal Tuihuangtang granules and traditional decoction in clinical efficacy. China Practical Medical 2016;11:187-8.
- Zhou QY, Mou Q. The clinical practice and efficacy of Chinese decocting-free granules and traditional decoction in treating migraine. Lishizhen Medicine and Materia Medica Research 2013;24:2201-2.
- Jin XJ. The efficacy of Chinese decoctiong-free granules and traditional decoction in treating migraine. Medical Information 2015;28:256-7.
- Peng M. Comparison of Traditional Chinese Medicine decoction pieces and decocting-free granules in treating migraine in clinical efficacy. Chinese Medicine Modern Distance Education of China 2014;12:51-2.
- Li J, Li CY. The efficacy of decocting-free Chinese herbs in the treatment of palmoplantar pustulosis. China Health Care & Nutrition 2013;23:5369.
- Xue CM, Yang LY. Clinical observation of Liangxue Xiaoyin granules in treatment of psoriasis. Chinese Journal for Clinicians 2014;42:34-5.
- Shen JH. Comparison of traditional decoction and Chinese dispensing granules for Waiganfang in clinical efficacy. World Health Digest 2011;8:288-9.
- Zhong L. The clinical efficacy and pharmacological effects of Huogou Tuire dispensing granules and traditional decoction in treating exogenous fever in children. Journal of Aerospace Medicine 2014;25:392-3.
- Li Y. The comparison of Chinese dispensing granules and traditional decoction in treating wind-heat type common cold. Nei Mongol Journal of Traditional Chinese Medicine 2016;35:14-5.
- Yang WH. Huogou Tuire dispensing granules and traditional decoction in treating 120 cases with exopathic fever in children. Journal of Emergency in Traditional Chinese Medicine 2012;21:275-6.
- Li LJ. Comparison of Zisuye decoction-free granules and decoction in treating common cold due to wind-cold. Journal of North Pharmacy 2016;13:78-9.
- Yang T, Sheng R, Yan BH, et al. Comparison of the efficacy between Qingqiao Kangdu decocting-free granules and traditional decoction in the treatment of common cold with exogenous wind-heat syndrome. Journal of Traditional Chinese Medicine 2014;55:2114-6.
- Huang YM. The efficacy of Qushihuazhuotang dispensing granules in treating impaired glucose tolerance. Cardiovascular Disease Journal of Integrated Traditional Chinese and Western Medicine (Electronic) 2016;4:111-2.
- Wu C, Zhang J, Zhao Y, et al. Chinese herbal medicine bushen qinggan formula for blood pressure variability and endothelial injury in hypertensive patients: a randomized controlled pilot clinical trial. Evid Based Complement Alternat Med 2014;2014:804171. [Crossref] [PubMed]
- Wu CX, Zhang JC, Liu Y, et al. The efficacy of different preparations for Bushen Qianggan Formula in treating patients with hypertension caused by yin deficiency and yang excess and the level of Angiotensin II. Chinese Journal of Gerontology 2013;33:1753-5.
- Li DD, Liu C. Comparative effect of different formulations of Qinzhiyuzhike Decoction in treatment of cough caused by phlegm obstruct lung. Hubei Journal of Traditional Chinese Medicine 2014;36:8-9.
- Dai YN, Wang ZS. Comparison of dispensing granules and traditional decoction for coronary heart disease mixture. Chinese Journal of Experimental Traditional Medical Formulae 2016;22:182-7.
- Yan WZ, Wang Y, Cheng XM. Effect comparison between Traditional Chinese Medicine granule preparation and traditional decoction of Duhuo Jisheng Decoction in treating rheumatoid arthritis. Journal of Chinese Medicinal Materials 2014;37:1314-5.
- Shen HS, Rao YY, Xue X. Clinical trials of Cough Mixture in treating asthma. Sichuan Medicial Journal 2007;28:177.
- Hui XG, Ren XH, Sun Q, et al. Comparison of decoction and granules for Suanzaorentang in treating female climacteric insomnia. Hebei Medicine 2013;19:1885-6.
- Zhou P, Liu W, Wang SL. The clinical observation of Qingre Huatan Anshen granules in treating330 patients with insomnia. Journal of Sichuan of Traditional Chinese Medicine 2008;26:68-9.
- Chen FM, Ma SG, Zhang XY, et al. Observation on clinical efficacy of Traditional Chinese Medicine in treatment of children with sleep disorders. Chinese Archives of Traditional Chinese Medicine 2013;31:2200-2.
- Zhang LZ. The efficacy of Chinese dispensing granules and traditional decoction in treating migraine. Journal of Clinical Medical Literature 2015;2:4373-4. (Electronic Edition).
- Huang KT, Zhou SF, Fan ZY, et al. Comparison of granules and decoction for Duhuojishengtang in treating protrusion of lumbar intervertebral disc. Chinese Manipulation & Rehabilitation Medicine 2014;5:156-7.
- Dong X, Lin YW, Chen ZX, et al. Comparison of dispensing granules and traditional decoction of Hejiefang in treating chronic hepatitis B. Journal of Chinese Medicinal Materials 2011;34:1004-6.
- Wang YZ. Chinese herbal granules in treating acute icteric hepatitis B for 50 cases. Guangming Journal of Chinese Medicine 2013;28:933-4.
- Lin WH, Wu CJ, Tian L. Comparison of clinical effect of Yinchenhao granules and decoction in treating chronic hepatitis B with liver and gallbladder damp-heat syndrome. China Pharmaceuticals 2014;23:108-9.
- Chen RF, Lin QY, Xu YZ, et al. Clinical trials of Yiweisan granule in treating chronic gastritis. Clinical Journal of TCM 2009;21:295-6.
- Yang H, Tian LJ, Geng YH, et al. Effect of Yiqizhuyu decoction on uterine myoma peri-menopausal period. Hebei Journal of Traditional Chinese Medicine 2008;30:687-8.
- Zhao L, Li AY, Qi FH. Clinical observation of Sangke granules in treating 50 children with acute bronchitis. Journal of Zhejiang University of Traditional Chinese Medicine 2009;33:774,6.
- He YC, Liu ZJ, Tian ZP, et al. Observation of Kouchuangqing decocting-free granules in treating herpetic stommightitis. Chinese Journal of Aesthetic Medicine 2012;21:267-8.
- Fan HX. Decocting-free granule of Haizao Kaiyintang in treating 32 patients with chronic laryngitis. Hunan Journal of Traditional Chinese Medicine 2012;28:72-3.
- Zhu MG, Chen GJ, Yang JB, et al. The clinical trials of Guben Tiaozhi decocting-free granules and traditional decoction in treating hyperlipemia. China Practical Medicine 2014;9:142-3.
- Ni SM, Leng JC, Fan SZ. Clinical effects of Liquorice-Ginseng Haemostatic compound in treatment of non-variceal gastrointestinal bleeding in elderly patients. China Modern Doctor 2016;54:115-9.
- Qin YW, Huang W. Observation of Buyang Huanwutang decocting-free granules for treating apoplexy sequelae in clinical effecacy. Guide of China Medicine 2014;12:269-70.
- Yang H, Jin HY, Zhang W, et al. Therapeutic evaluation of Bushenrougan therapy in the treatment of premature ovarian failure. Modern Journal of Integrated Traditional Chinese and Western Medicine 2013;30:802-3,14.
- Lin B, Yu XX, Xie JR. Observation of the efficacy for Chinese herbal granules and traditional decoction in treating osteoporosis caused by deficiency of the kidney essence. Journal of North Pharmacy 2014;11:43.
- Feng L, Fang LP, Cong P. Comparison of concentrated granules and traditional decoction for Bazhengsan. Fujian Journal of TCM 2005;36:39-40.
- Li Y, Lu DG, Lei YQ, et al. Comparison of ferulic acid and paeoniflorin between traditional slice decoction and dispensing granule decoction of Siwu Tang. Zhong Yao Cai 2008;31:125-8. [PubMed]
- Cao PX, Liang GY, Xu BX, et al. Determination of glycyrrhizic acid in MAHUANG DECOCTION by HPLC when decocted separately or as a whole. Chinese Traditional and Herbal Drugs 2001;32:24-6.
- Li SL, Song JZ, Qiao CF, et al. UPLC-PDA-TOFMS based chemical profiling approach to rapidly evaluate chemical consistency between traditional and dispensing granule decoctions of traditional medicine combinatorial formulae. J Pharm Biomed Anal 2010;52:468-78. [Crossref] [PubMed]
- Zhang XQ, Liu YW, Zhang CB, et al. Pharmacodynamic comparison between Sanhuang decoction for purging stomach-fire and its concentrated granule. Journal of Chinese Medicinal Materials 2002;25:117-9. [PubMed]
- Shang E, Zhu Z, Liu L, et al. UPLC-QTOF-MS with chemical profiling approach for rapidly evaluating chemical consistency between traditional and dispensing granule decoctions of Tao-Hong-Si-Wu decoction. Chem Cent J 2012;6:143. [Crossref] [PubMed]
- Chinese Pharmacopoeia Commission. Pharmacopoeia of the People’s Republic of China. China Medical Science Press, 2015.
- Layne K, Ferro A. Traditional Chinese medicines in the management of cardiovascular diseases: a comprehensive systematic review. Br J Clin Pharmacol 2017;83:20-32. [Crossref] [PubMed]
- Hao PP, Jiang F, Chen YG, et al. Traditional Chinese medication for cardiovascular disease. Nat Rev Cardiol 2015;12:318. [Crossref] [PubMed]
- Samuel JP, Bell CS. Unique Study Designs in Nephrology: N-of-1 Trials and Other Designs. Adv Chronic Kidney Dis 2016;23:351-4. [Crossref] [PubMed]