Electrocardiographic artifact potentially misleading to the wrong management
Introduction
Parkinson’s disease (PD) is a common neurological disorder with depletion of dopaminergic neurons in the substantia nigra pars compacta (1). It affects approximately 1–2% of people 65 years and older (2). The motor symptoms include bradykinesia, muscular rigidity, postural and gait impairment, and rest tremor. The predominant non motor symptoms are olfactory dysfunction, autonomic dysfunction, psychiatric symptoms, sleep disorders, cognitive impairment, pain and fatigue (1). Atrial flutter (AF) is an uncommon arrhythmia encountered in clinical settings, which requires careful evaluation. It is characterized by an atrial rate of approximately 300 beats/minute and a regular ventricular rate of about 150 beats/minute. Patients usually present with symptoms of dyspnea, palpitations, fatigue, and dizziness. The risk of subsequent cerebral embolization with lone AF is as high as with lone atrial fibrillation, therefore appropriate electrocardiographic diagnosis is of utmost importance for guiding subsequent management plan (3,4).
Artifacts are a common finding in patients requiring an electrocardiogram (ECG) in the in-patient setting. Hence while making a diagnosis of tachyarrhythmia, one must always consider the possibility of an artifact. This can save unnecessary aggressive interventions, like administration of anticoagulation, that are not inconsequential. The typical resting tremor of PD is present at rest with a frequency of 4–6 hertz, which is similar to that of AF i.e., 250–350/min, and also overlaps that of ventricular tachycardia i.e., 120–250/min. Parkinsonian tremors are one of the common causes of electrocardiographic artifacts resembling AF (2,5-11).
In this case report, we present an interesting case of a diagnostic challenge manifested as an ECG recording mimicking AF in a patient with PD and discuss existing literature.
Case presentation
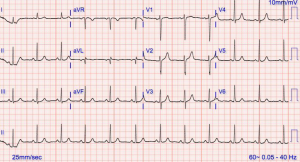
Our patient was a 72-year-old African-American female with history of PD who presented to our Emergency Department with a one day history of chest pain; which was described as midsternal tightness relieved by taking oral antacids. She denied shortness of breath, dyspnea, orthopnea, palpitations, or syncope. No other cardiovascular risk factors of significance were present. She denied any family history of heart disease. Her home medications included carbidopa-levodopa, entacapone, ranitidine and potassium chloride. Her vital signs were within normal limits (blood pressure: 110/80 mmHg; heart rate: 80 bpm; RR, 16–18; afebrile). Physical exam was remarkable for bilateral resting hand tremors at a frequency of 6–8 hertz and mild cogwheel rigidity in both upper extremities. Her initial labs were within normal limits with 2 negative troponins (<0.015×2), sodium of 145, potassium of 3.7, chloride of 112, carbon dioxide of 26, creatinine of 0.6, magnesium of 22, and BNP of 19. Initial ECG was interpreted as AF prompting admission (Figure 1). After careful review of her ECG by a cardiologist, several features such as sharply contoured upright p waves in all leads, different flutter wave morphologies in the same leads, more prominence of “pseudo-flutter” waves in the limb leads compared to the precordial leads, and return to isoelectric baseline after sharp peaked p waves, questioned the diagnosis of AF. Also, the RR interval was not consistently a multiple of PP interval. Additionally, our patient had upright p waves in V1 that in case of AF is indicative of cavotricuspid-isthmus origin. However with cavotricuspid-isthmus origin, inferior leads will usually have negatively deflected p waves, but in our patient both V1 and the inferior leads had an upward deflection, which again favors the diagnosis of artifact over flutter. A repeat 12 lead ECG clearly demonstrated normal sinus rhythm (Figure 2), and the patient remained completely asymptomatic throughout the stay. A 48-hour Holter monitoring in the clinic later confirmed consistent sinus rhythm with no evidence of any arrhythmias.

Discussion
Artifact is a common finding in the EKG of patients in hospital setting. It can mimic a number of arrhythmias causing patients to be subjected to unnecessary and potentially dangerous therapeutic interventions (6). Consistency of parkinsonian tremor closely mimics that of AF as seen in our case, making this an uncommon but potentially misleading associated phenomenon. With our patient, a misdiagnosis of AF could have led to lifelong anticoagulation, given her CHA2DS2-VASc score of 2 (12).
Hwang et al. performed a study in which they enrolled 100 patients with parkinsonian resting tremor to assess the frequency and patterns of tremor-induced artifacts in outpatient setting. The study demonstrated high frequency of artifacts in PD patients and showed baseline undulation in 78% of patients and AF/fibrillation or ventricular tachycardia mimics in 11% of patients. Patients with high tremor scores, as judged by neurologist, were more prone to develop AF/fibrillation or ventricular tachycardia mimics (2). The copies of ECGs were evaluated by postgraduate year 1, neurology residents, internal medicine residents and cardiologists, who were given relevant medical information and were asked to recommend patient management based on their readings of the ECG. The rate of ECG misreading leading to spurious diagnosis of AF/fibrillation or ventricular tachycardia and prescription of anticoagulation was 14.3% (3/11 patients) with automated electrocardiograph, 45% (5/11 patients) with postgraduate year 1 residents, 9.1% (1/11 patients) with neurology residents, and 9.1% (1/11 patients) with internal medicine residents. Cardiology chief residents and fellows correctly identified all artifacts, indicating that professional training is associated with better judgment (2).
Tremor induced artifact can be misinterpreted as supraventricular tachyarrhythmias or ventricular arrhythmias if the amplitude is sufficient (13). Several clinical and electrographic characteristics to differentiate tremor induced artifacts from cardiac arrhythmias should be routinely observed. When obtaining an EKG, it is prudent to minimize environmental interference, such as patient movement from speaking, electromagnetic interference from cell phones, and to limit muscle tremor if possible (i.e., hypothermic or convulsive patients) (14). EKG characteristics to suggest tremor induced arrhythmia include abrupt onset and termination, presence of normal p wave and/or QRS complex prior to and after arrhythmia, uncharacteristic p wave and/or QRS complex morphology with sharp contours, absence of arrhythmia in all leads, and on careful inspection the presence of normal p wave and/or QRS complex that march out throughout the event (15). In the setting of suspected tremor induced ventricular arrhythmias, hemodynamic stability is expected and strengthens the diagnosis.
Lastly, it’s important to note that parkinsonian tremor is present in the limbs and face but not in the trunk; therefore, the tremor induced artifacts are present in corresponding limb-leads and less so in the precordial leads.
Clinical implication of misdiagnosis of AF or atrial fibrillation and subsequent therapeutic interventions are many. Firstly, prescription of anticoagulation with spurious diagnosis of AF poses the risk of serious intracranial hemorrhage in patients with advanced stages of PD in which postural instability and falls are common. Secondly, it causes unnecessary emotional stress on patient and families. Lastly, the prescriptions of anticoagulation and associated hospital/clinical visits causes financial burden on patients/families and contributes towards increasing health care cost burden.
In conclusion, our case report highlights several differentiating electrocardiographic features of tremor induced artifacts from those of AF. Correct and accurate diagnosis requires a careful inspection of the ECG and clinical correlation with the patient’s symptoms. This is critically important, in order to avoid wrong treatment and unnecessary interventions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: An informed consent was obtained from the patient to publish this case report.
References
- Kalia LV, Lang AE. Parkinson’s disease. Lancet 2015;386:896-912. [Crossref] [PubMed]
- Hwang WJ, Chen JY, Sung PS, et al. Parkinsonian tremor-induced electrocardiographic artifacts mimicking atrial flutter/fibrillation or ventricular tachycardia. Int J Cardiol 2014;173:597-600. [Crossref] [PubMed]
- Granada J, Uribe W, Chyou PH, et al. Incidence and predictors of atrial flutter in the general population. J Am Coll Cardiol 2000;36:2242-6. [Crossref] [PubMed]
- Halligan SC, Gersh BJ, Brown RD Jr, et al. The natural history of lone atrial flutter. Ann Intern Med 2004;140:265-8. [Crossref] [PubMed]
- Parkin TW, Connolly DC. Muscle-tremor artifact due to parkinson's syndrome. it stimulated atrial flutter and disappeared during sleep. Postgrad Med 1965;37:718-20. [Crossref] [PubMed]
- Chase C, Brady WJ. Artifactual electrocardiographic change mimicking clinical abnormality on the ECG. Am J Emerg Med 2000;18:312-6. [Crossref] [PubMed]
- Vanerio G. Tremor as a cause of pseudo atrial flutter. Am J Geriatr Cardiol 2007;16:106-8. [Crossref] [PubMed]
- Nam MC, Best L, Greaves K, et al. Global pseudo-atrial flutter ECG appearance secondary to unilateral parkinsonian tremor. BMJ Case Rep 2016;2016. [PubMed]
- Hwang WJ. Tremor-induced electrocardiographic artifact mimicking atrial flutter. Acta Neurol Taiwan 2008;17:151-2. [PubMed]
- Prabhavathi B, Ravindranath KS, Moorthy N, et al. Pseudo-atrial flutter/fibrillation in Parkinson’s disease. Indian Heart J 2009;61:296-7. [PubMed]
- Nolan NS, Koerber SM, Balla S. Pseudoatrial Flutter Waves -- When a Flutter Is Not a Flutter. JAMA Intern Med 2016;176:298-9. [Crossref] [PubMed]
- Lip GY. Using the CHA(2)DS(2)-VASc score for stroke risk stratification in atrial fibrillation: a clinical perspective. Expert Rev Cardiovasc Ther 2013;11:259-62. [Crossref] [PubMed]
- Patel S. Electrocardiographic artifact mimicking ventricular tachycardia during high-frequency oscillatory ventilation: a case report. Am J Crit Care 2006;15:310-1. [PubMed]
- Van Mieghem C, Sabbe M, Knockaert D. The clinical value of the ECG in noncardiac conditions. Chest 2004;125:1561-76. [Crossref] [PubMed]
- Knight BP, Pelosi F, Michaud GF, et al. Clinical consequences of electrocardiographic artifact mimicking ventricular tachycardia. N Engl J Med 1999;341:1270-4. [Crossref] [PubMed]